Patient Preparation
- Same for PET and SPECT
- Fast for ≥6 hrs (except water intake)
- Avoid caffeine for ≥12 hours
- Avoid theophylline-containing medications for ≥ 48 hours
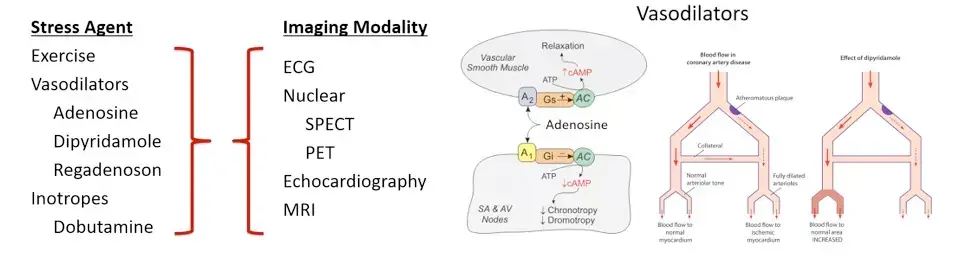
Vasodilators
- Most commonly, vasodilators are used to ↑ blood flow to normally perfused areas of the myocardium, uncovering potential areas of decreased perfusion caused by fixed coronary stenoses.
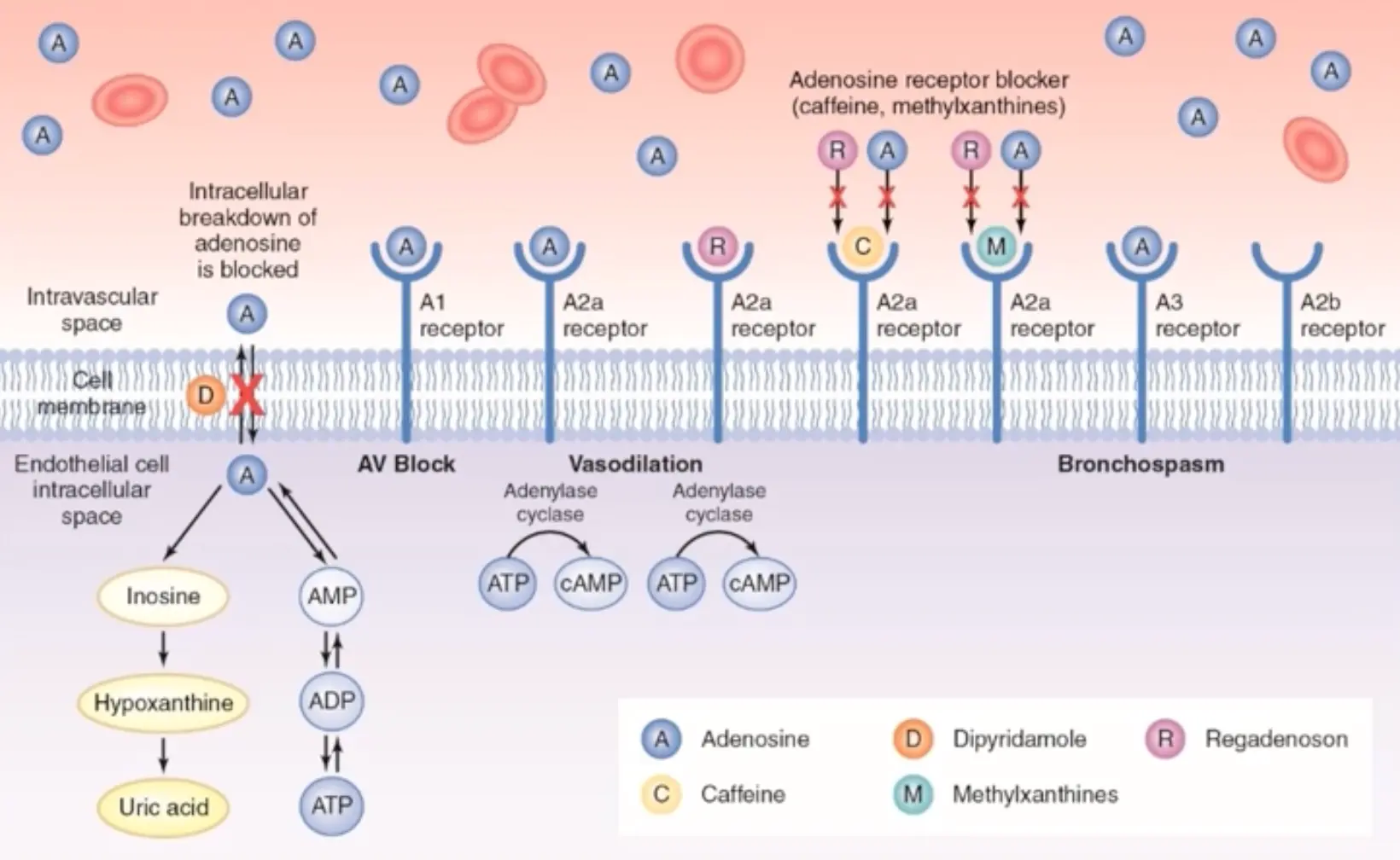
- All vasodilators act through the adenosine pathway leading to vascular smooth muscle vasorelaxation.
- Figure source
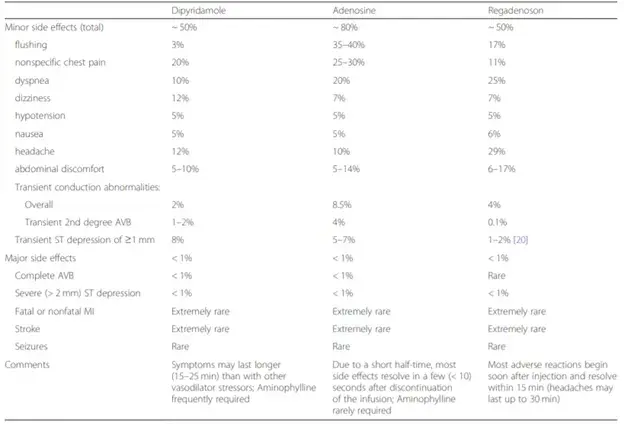
- Side effects with vasodilators 1
- Vasodilators are safe in patients with a history of COPD or asthma, but do not give vasodilators in a patient with a recent exacerbation or active wheezing.
- Indications for reversal of vasodilators (although most side effects are self-limiting)
- Indications for reversal include severe hypotension, 2nd- or 3rd-degree heart block, ST depression with angina, wheezing, or intolerable symptoms.
- Adenosine almost never requires reversal due to the short half-life.
- For mild symptoms, ask patient to consume coffee ☕️ or diet soda 🥤 after completing the test.
- Reversal agents:
- Aminophylline 50-250mg IV over 1 minute (do not give if having a seizure as this lowers the seizure threshold).
- IV theophylline 50mg slow injection over 1 minute.
- IV caffeine 60mg in 25mL of D5W over 3-5 minutes.
- PO caffeine 60-160mg
Adenosine
- See Adenosine
- Adenosine directly activates the A2a receptor causing coronary vasodilation, but also activates other adenosine receptors.
- Half-life is 2-10 seconds.
- Off-target effects:
- A1 receptor: AV block, chest pain and tachypnea
- A2b receptor: peripheral vasodilation (headache, diarrhea)
- A2b/A3 receptor: bronchospasm
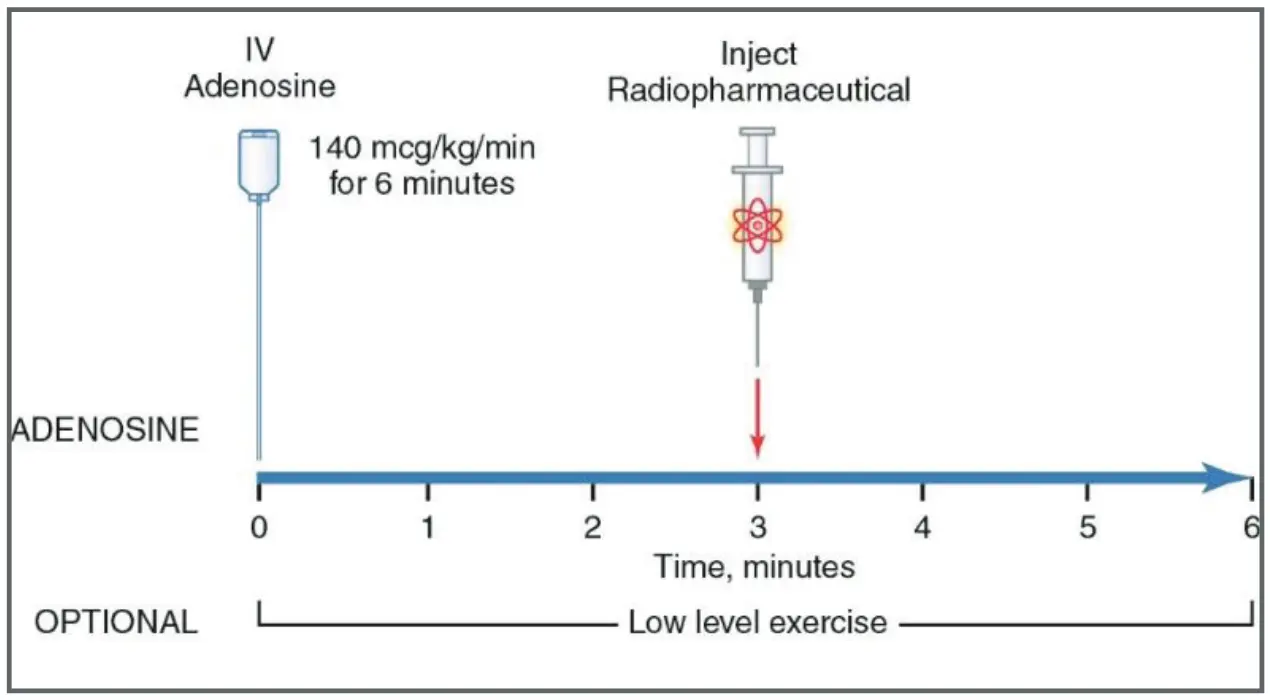
- Protocol: continuous infusion of 140 mcg/kg/min for 6 minutes, inject radiotracer at 3 minutes.
- Contraindications: bronchospasm, hypotension, heart block.
Regadenoson (Lexiscan)
- Regadenoson (Lexiscan): Directly activates A2a receptors with high affinity and low off-target effects causing coronary vasodilation.
- -selective adenosine receptor agonist
- Half-life for hyperemia is 3-5 minutes.
- Peak-effect onset at ~1 min post bolus injection with a duration of approximately 8 to 10 minutes at ≥80% peak effect
- Triphasic half-life so may have side effects of headache, chest pain, diarrhea for 15-20 minutes.
- Off-target effects are less than with adenosine.
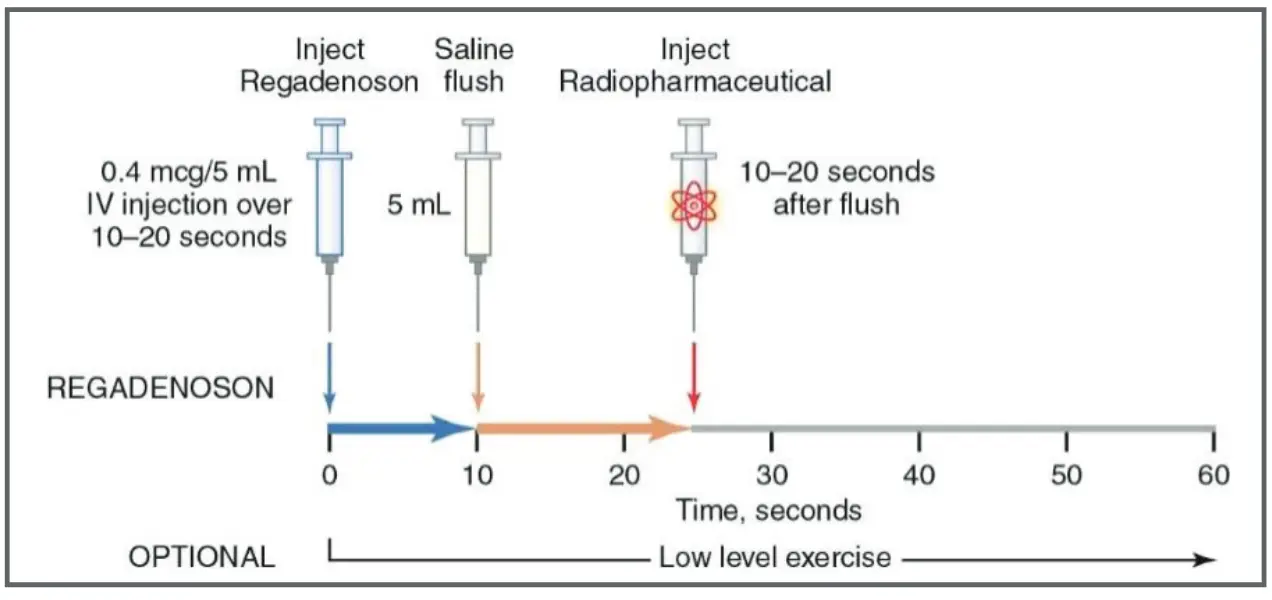
- Protocol: rapid injection over 10 seconds followed by saline flush. Radionuclide is injected 10-20 seconds after saline.
- Caution: seizures, LBBB, pacemaker.
- Bradyarrhythmias with regadenoson are thought to be secondary to vagal stimulation via the A2a receptor in the hypothalamus and nucleus solitarius.
- ADVANCE trial compared Regadenoson vs Adenosine
- Run-in phase to ensure all participants tolerated adenosine
- tl;dr: regadenoson provided similar Dx information compared to standard adenosine infusion. There were no serious AEs with regadenoson and regadenoson was better tolerated.
Dipyridamole (Persantine)
- Dipyridamole (Persantine): Phosphodiesterase inhibitor that prevents intracellular reuptake of adenosine.
- Half-life: Maximal hyperemia in 15 minutes. Alpha half-life is 30-60 minutes, beta half-life 10 hours.
- Off-target effects: Similar potential to adenosine. May have late symptoms after aminophylline reversal agents have worn off.
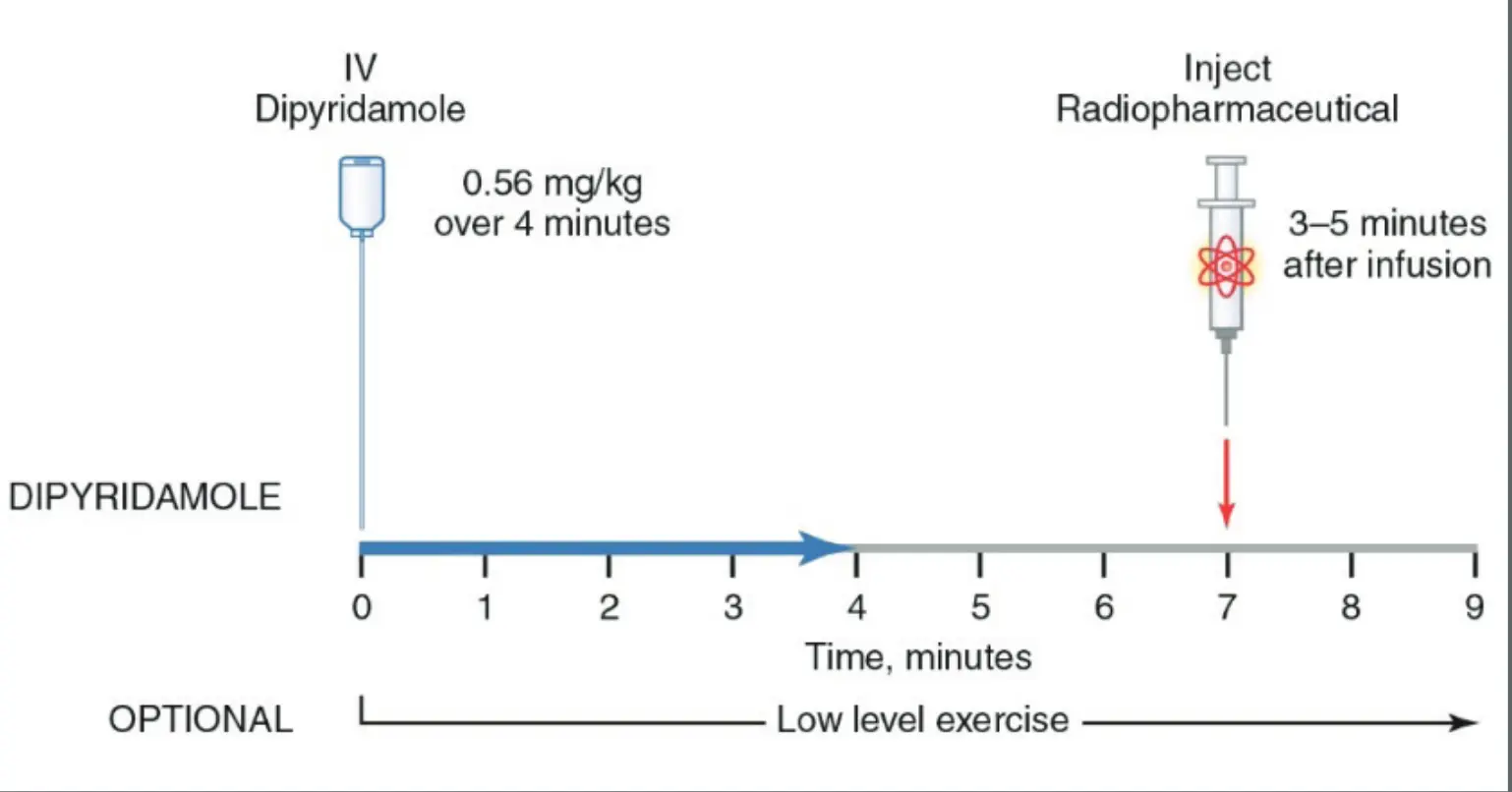
- Protocol: Infusion over 4 minutes, then inject radiotracer 3-5 min after dipyridamole infusion is complete.
- Consider using preferentially if history of seizure, pacemaker, LBBB.
The rate of side effects for vasodilator agents are seen in the above table.
Contraindications to Vasodilators
- Patients with significant reactive/bronchospastic lung disease with ongoing wheezing or recent exacerbation requiring steroids/significant escalation of medical therapy
- Second degree Mobitz Type 2 or third-degree AV block without a functioning pacemaker
- Severe symptomatic bradycardia without a functioning pacemaker
- Profound sinus bradycardia (heart rates per 40/min)
- Symptomatic aortic aneurysm
- Recent (<48 hours) use of dipyridamole or dipyridamole-containing medications (for regadenoson and adenosine)
- Ingestion of caffeinated foods or beverages within the last 12-24 hours
- Seizure disorder active within the last 6 months
- Junctional rhythm
- Acute left ventricular thrombus, especially mobile, protruding, or pedunculated
Indications for reversal/termination of Vasodilators
- Same are those mentioned for Exercise
- Symptomatic hypotension (SBP <90 mmHg)
- Wheezing
- Development of persistent second degree or complete AV block
- Other significant cardiac arrhythmia
- Excessive STD (horizontal or downsloping) >2 mm from baseline
- Severe or increasing chest pain of unclear etiology
- Can be considered in the presence of less-severe side effects or ischemic ECG changes if at least 1 minute has elapsed since radiotracer injection
Dobutamine
- Beta-adrenergic agonist:
- Hemodynamic effects similar to exercise
- Increases in coronary flow less than vasodilator stress
- Protocol: administered incrementally beginning at a dose of 5-10 mcg/kg/min, which is increased at 3-minute intervals to 20, 30, and 40 mcg/kg/min.
- Radiotracer is injected once ≥85% MPHR achieved with DBA infusion continuing for 1 minute after tracer injection.
- Use a weight-based dose up to 250 lbs.
- Dose increased incrementally to 40 mcg/min/kg
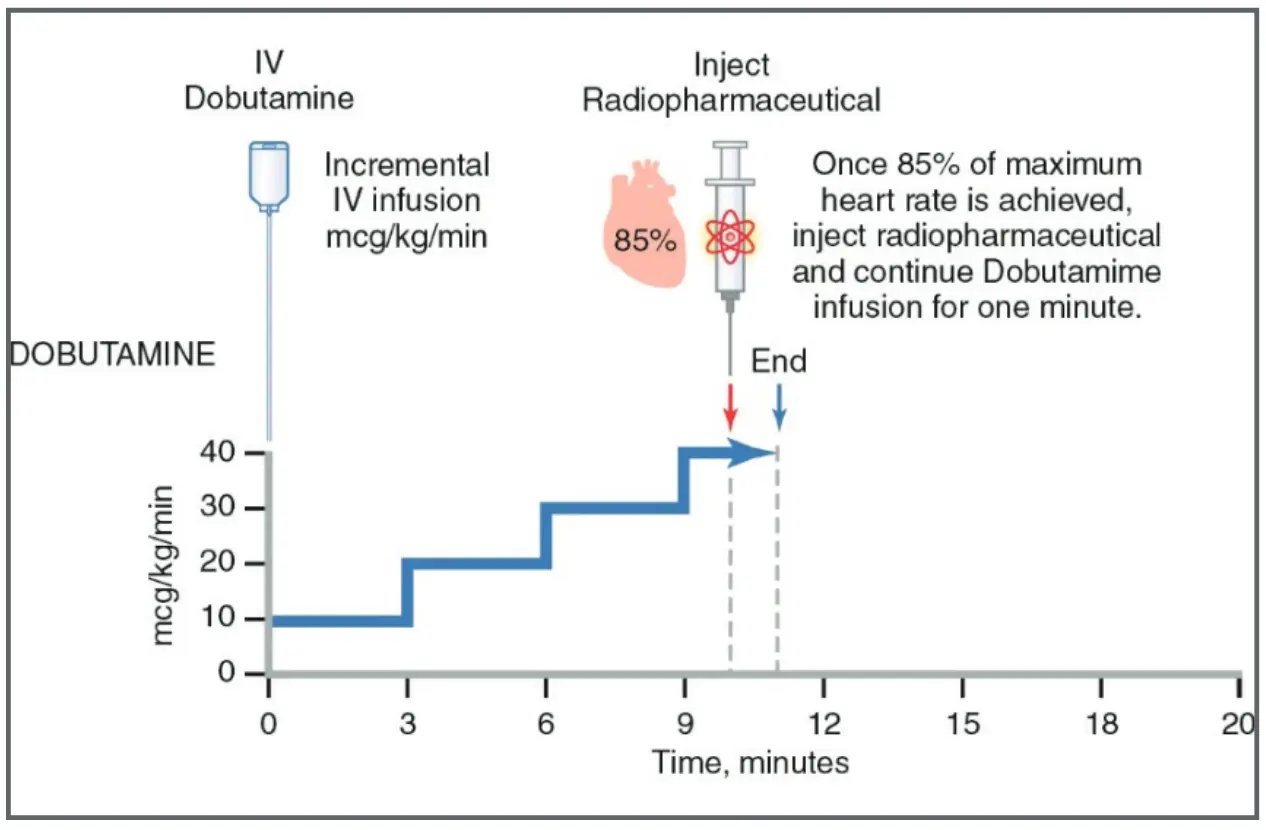
- Atropine administered to increase HR if required
- Use in pts unable to exercise with a contraindication to vasodilator stress
- Side-effects: palpitations, CP, dyspnea, headache, arrhythmia, Bezold-Jarisch reflex
Contraindications to Dobutamine
- Contraindications same as for exercise stress
- Acute left ventricular thrombus, especially mobile, protruding, or pedunculated
- Hypertrophic obstructive cardiomyopathy or other forms of significant left ventricular outflow tract obstruction (ie, aortic membrane)
- Prior history of VT
- Symptomatic or severely enlarged aortic aneurysm
- Uncontrolled or poorly rate controlled atrial fibrillation/flutter
- Known hypersensitivity to dobutamine
- Patients who are on Beta-blockers where the heart rate and inotropic responses to dobutamine will be attenuated
- LBBB, ventricular pacing, and ventricular pre-excitation (WPW syndrome) when perfusion images are being performed should preferentially undergo pharmacologic vasodilator stress.