- With any stress modality, want a double product (adequate stress to draw prognostic information) >20,000 and ideally >25,000.
- See 2019 ASE Guidelines
- Make sure you get a good baseline Echo, e.g. “regional wma, severe AS, aortic enlargement, you sure you want to put him on a treadmill?”
- Bicycle 🚴♀️ is useful for measurement of MR
- Need to interpret with a grain of salt b/c venous return is very high relative to exercise and LV cavity will be large d/t this preload w/ bike.
- Prognostic information is comparable to SPECT
- Dobutamine: start at 5-10, increase every 3 minutes (20 → 30 → 40)
- If still not achieved, can give atropine
- Hypertensive response
- SBP >182 or DBP > 96 for DSE
- SBP > 220 for ESE
- Incidence of AFib with DSE is 1%
- <1 hr (61%) and <24h (96%)
- Rivas: will give some metoprolol and monitor in the lab. If still rapid AFib, will monitor and they typically go back into sinus overnight.
- False negatives
- suboptimal workload
- single vessel disease
- especially LCx disease
- concentric LVH, HCM
- severe AI or MR because you have a hyperdynamic LV
- False positives
- Hyperrtensive response to stress
- LVH/HCM, DM → low MPR
- exercise-induced coronary spasm
- cardiomyopathy
- LBBB (pharmacologic MPI is test of choice)
- High risk features - see Table 3 from the ASE guideline paper
- Contraindications
- Poor windows
- Unable to reach target HR
- Uncontrolled HF
- High-risk unstable angina, active ACS or AMI (<2 d)
- Serious ventricular arrhythmia or high risk for arrhythmias attributable to QT prolongation
- Respiratory failure
- Severe COPD, acute PE, severe pulmonary hypertension
- Contraindications to dobutamine (if pharmacologic stress test needed)
- Severe systemic arterial hypertension (e.g., ≥200/110 mm Hg)
- Useful if patient can exercise and ECG uninterpretable
- Widely available & easy to perform
- Inexpensive
- No ionizing radiation
- Body habitus and echo window
- Qualitative interpretation
- Limited sensitivity (~70%) but better specificity (~80%)
- For detection of CAD, stress echocardiography has similar sensitivity to tomographic nuclear perfusion imaging.
- However, stress echocardiography has higher specificity (89% vs. 77%).
- For detection of left main or multivessel CAD, stress echocardiography has greater sensitivity.
- 📄 Pellikka, P. A., Arruda-Olson, A., Chaudhry, F. A., Chen, M. H., Marshall, J. E., Porter, T. R., & Sawada, S. G. (2020). Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography. Journal of the American Society of Echocardiography, 33(1), 1-41.e8. https://doi.org/10.1016/j.echo.2019.07.001
- Indications
- Known or suspected coronary artery disease
- Myocardial viability
- Dyspnea of possible cardiac origin
- Pulmonary hypertension
- Mitral valve disease
- Aortic stenosis (low-flow)
- Hypertrophic cardiomyopathy
- e.g. don’t have 30 mmHg threshold at rest echo
- Interpretation
- At least two adjacent segments are required for test positivity.
- The wall motion score index (WMSI) is derived by dividing the sum of the scores of individual segments by the number of segments visualized (severely abnormal > 1.7).
- 1.2 - 1.7 is moderate
- 📄 Sicari, R., Nihoyannopoulos, P., Evangelista, A., Kasprzak, J., Lancellotti, P., Poldermans, D., Voigt, J.-U., & Zamorano, J. L. (2008). Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). European Journal of Echocardiography, 9(4), 415–437. https://doi.org/10.1093/ejechocard/jen175
 Image source: 📄 Pellikka, P. A., Arruda-Olson, A., Chaudhry, F. A., Chen, M. H., Marshall, J. E., Porter, T. R., & Sawada, S. G. (2020). Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography. Journal of the American Society of Echocardiography, 33(1), 1-41.e8. https://doi.org/10.1016/j.echo.2019.07.001
Image source: 📄 Pellikka, P. A., Arruda-Olson, A., Chaudhry, F. A., Chen, M. H., Marshall, J. E., Porter, T. R., & Sawada, S. G. (2020). Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography. Journal of the American Society of Echocardiography, 33(1), 1-41.e8. https://doi.org/10.1016/j.echo.2019.07.001
| Stress method | Normal response Regional | Ischemic response Regional | Normal response Global | Ischemic response Global |
|---|---|---|---|---|
| Treadmill | Hyperkinesis post-exercise compared to rest | Hypokinesis compared to rest | Increase in EDV Decrease in ESV Increase in EF | Increase in EDV Increase in ESV Decrease in EF in left main, multivessel disease |
| Supine Bicycle | Hyperkinesis with exercise but less than with treadmill, dobutamine | Hypokinesis compared to rest | Small increase in EDV Decrease in ESV Modest increase in EF | Increase in EDV Increase in ESV Decrease in EF in left main, multivessel disease |
| Dobutamine | Marked hyperkinesis Increased velocity of contraction compared to rest and low dose | Hypokinesis and decreased velocity of contraction compared to low dose, and usually compared to rest | Decrease in EDV Marked decrease in ESV Marked increase in EF | Decrease in EF, cavity dilatation are infrequent with left main, multivessel disease |
| Vasodilator | Hyperkinesis with stress compared to rest | Hypokinesis compared to rest | Decrease in EDV Decrease in ESV Increase in EF | Decrease in EF, cavity dilatation are infrequent with left main, multivessel disease |
| Atrial Pacing | Mild hyperkinesis or no change in function compared to rest | Hypokinesis compared to rest | Decrease in EDV Decrease in ESV No change in EF | Decrease in EDV No change or increase in ESV Decrease in EF with left main, multivessel disease |
Table Source: Table 3 from 📄 Pellikka, P. A., Arruda-Olson, A., Chaudhry, F. A., Chen, M. H., Marshall, J. E., Porter, T. R., & Sawada, S. G. (2020). Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography. Journal of the American Society of Echocardiography, 33(1), 1-41.e8. https://doi.org/10.1016/j.echo.2019.07.001
Prognostic value of Stress Echo
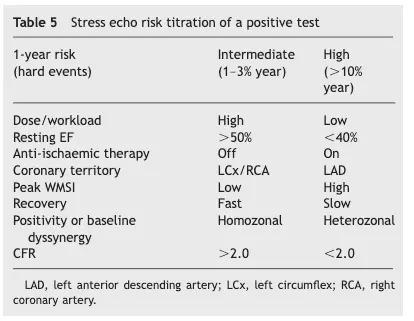 Table source: 📄 Sicari, R., Nihoyannopoulos, P., Evangelista, A., Kasprzak, J., Lancellotti, P., Poldermans, D., Voigt, J.-U., & Zamorano, J. L. (2008). Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). European Journal of Echocardiography, 9(4), 415–437. https://doi.org/10.1093/ejechocard/jen175
Table source: 📄 Sicari, R., Nihoyannopoulos, P., Evangelista, A., Kasprzak, J., Lancellotti, P., Poldermans, D., Voigt, J.-U., & Zamorano, J. L. (2008). Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE) (a registered branch of the ESC). European Journal of Echocardiography, 9(4), 415–437. https://doi.org/10.1093/ejechocard/jen175
Abnormal Stress Echo, but Normal Cors
Focus on the apex
Talal recommends focus on the apex when assessing stress echo. LAD ischemia?
- Wall motion abnormalities in the absence of significant angiographic coronary stenosis should have you thinking of the following:
- Microvascular abnormalities
- Endothelial dysfunction
- Vasospasm
- Small vessel CAD
- Apical ballooning syndrome
- Amyloidosis