-
Related
-
Patients with variant ATTR amyloidosis may experience OH due to autonomic dysfunction
-
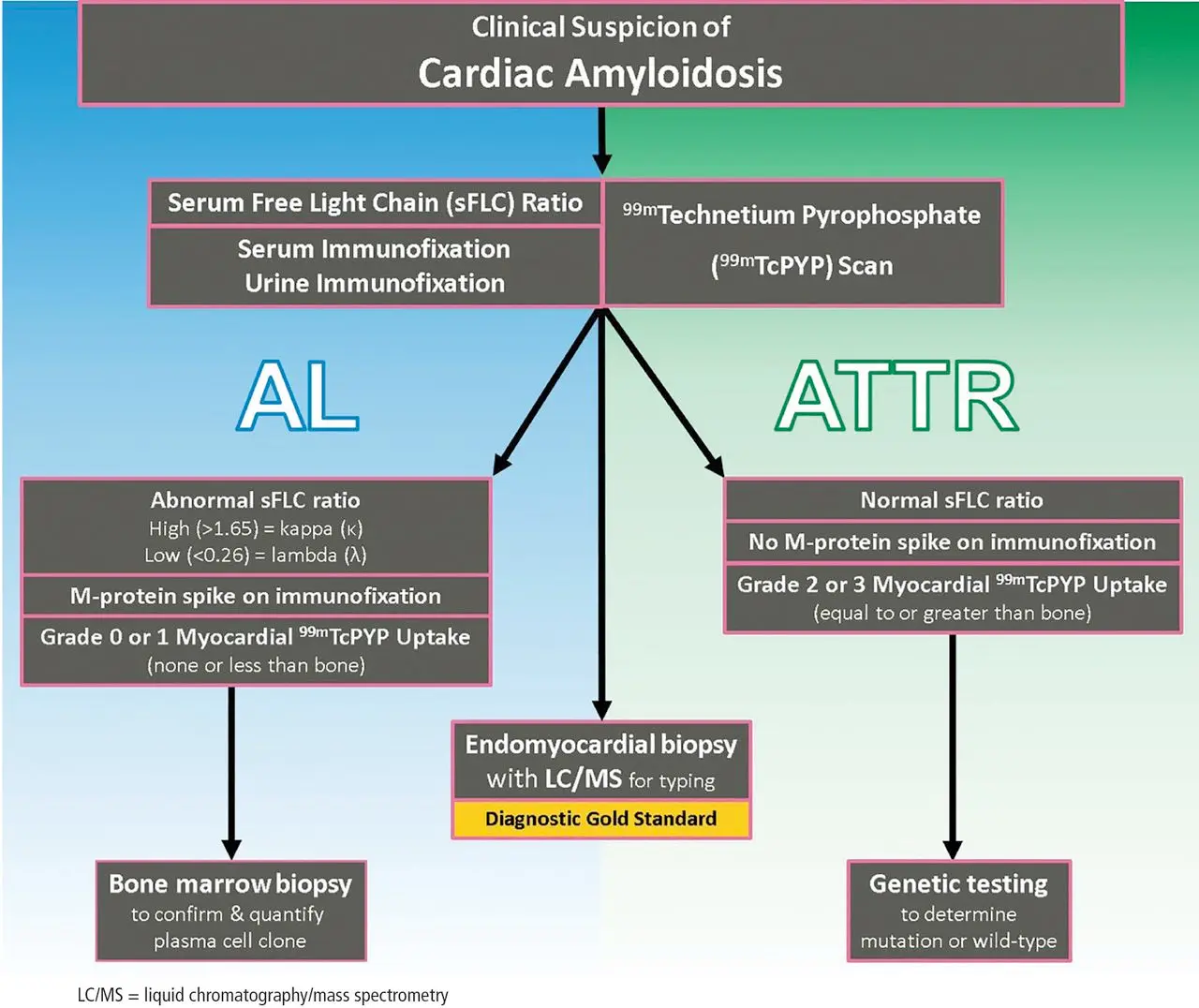
Exclude AL amyloidosis with work-up that includes serum FLCs, serum (SIFE), and urine immunofixation
-
Labs may reveal a chronic troponin elevation that remains flat
- d/t amyloid invasion into the vasculature causing microvascular ischemia
-
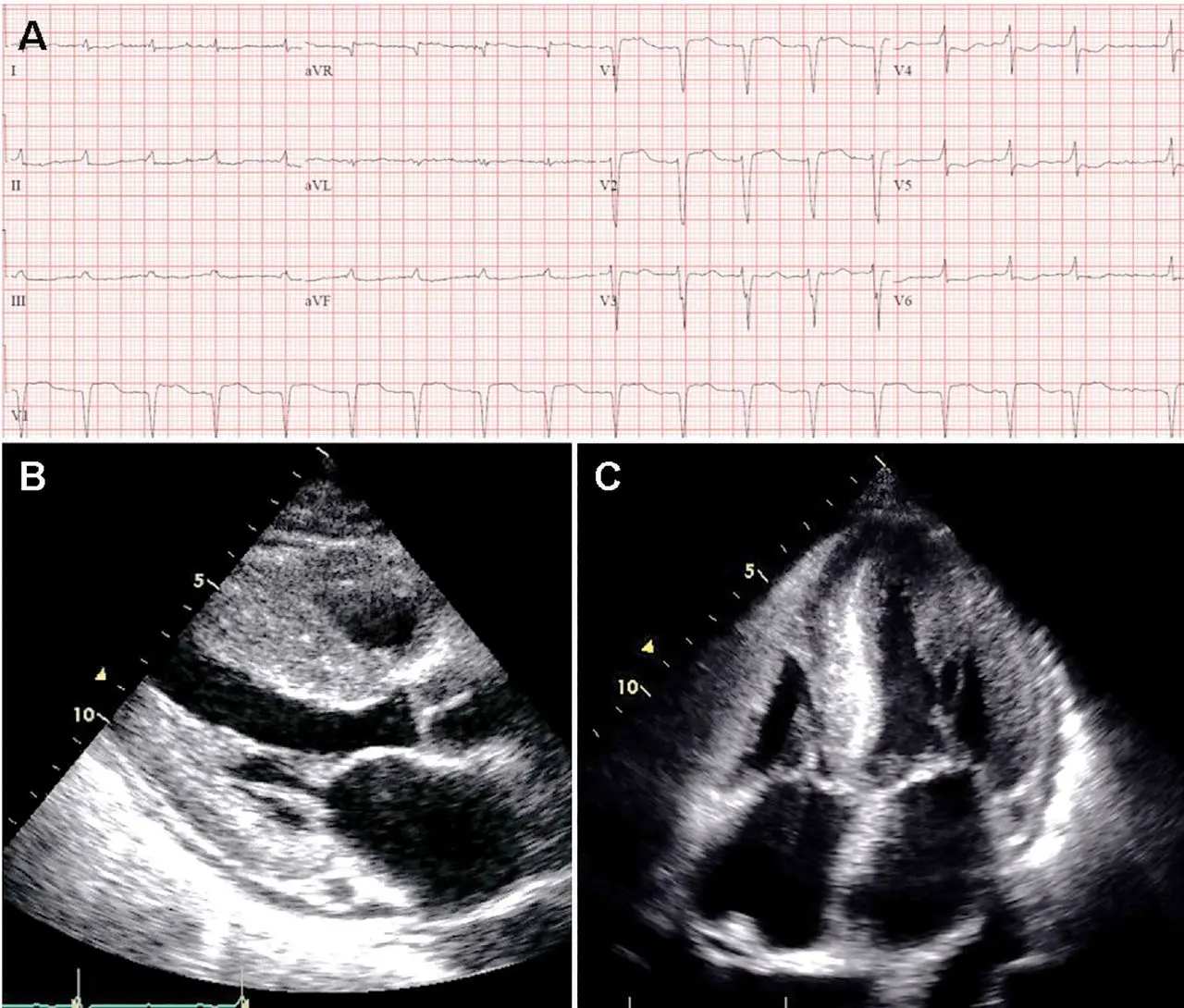
Echo:
- LV wall thickness >1.2 cm (0.6 cm to 1.0 cm is normal) in the absence of hypertension should prompt suspicion for CA. 1
- LVH is most commonly symmetric, but you may see asymmetric septal hypertrophy, particularly in ATTRwt-CA 1
- Strain Imaging with “apical sparing,” in which the apical LV segments have normal or near-normal strain compared with the mid and basal segments. 1
- LV wall thickness >1.2 cm (0.6 cm to 1.0 cm is normal) in the absence of hypertension should prompt suspicion for CA. 1
Discordance: LVH on Echo and Low-voltage on ECG
If you see LVH on echo but low-voltage on ECG, you should definitely suspect cardiac amyloidosis.
- ECG may show low-voltage and pseudo-infarct pattern (Q waves in early precordial leads, V1-V2) mimicking prior anteroseptal MI. 1
- 📝 only about 50% of patients with AL-CA and about 30% of patients with ATTR-CA meet true low-voltage criteria (QRS amplitude <5 mm in limb leads or <10 mm in precordial leads)
- Wide QRS complexes are more frequent in ATTR-CA and lower limb voltages are more frequent in AL-CA
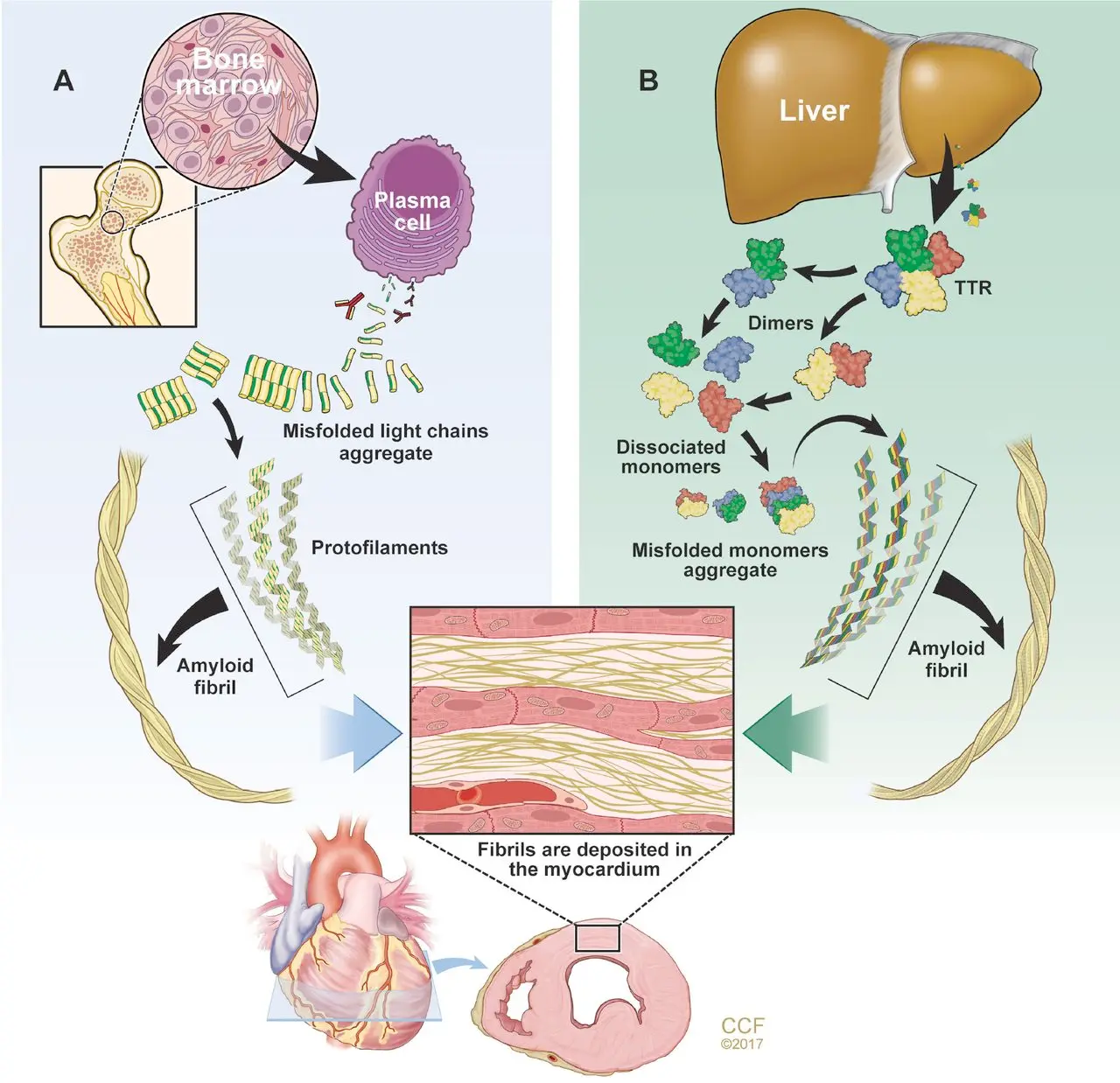
Pathophysiology
Diagnosis
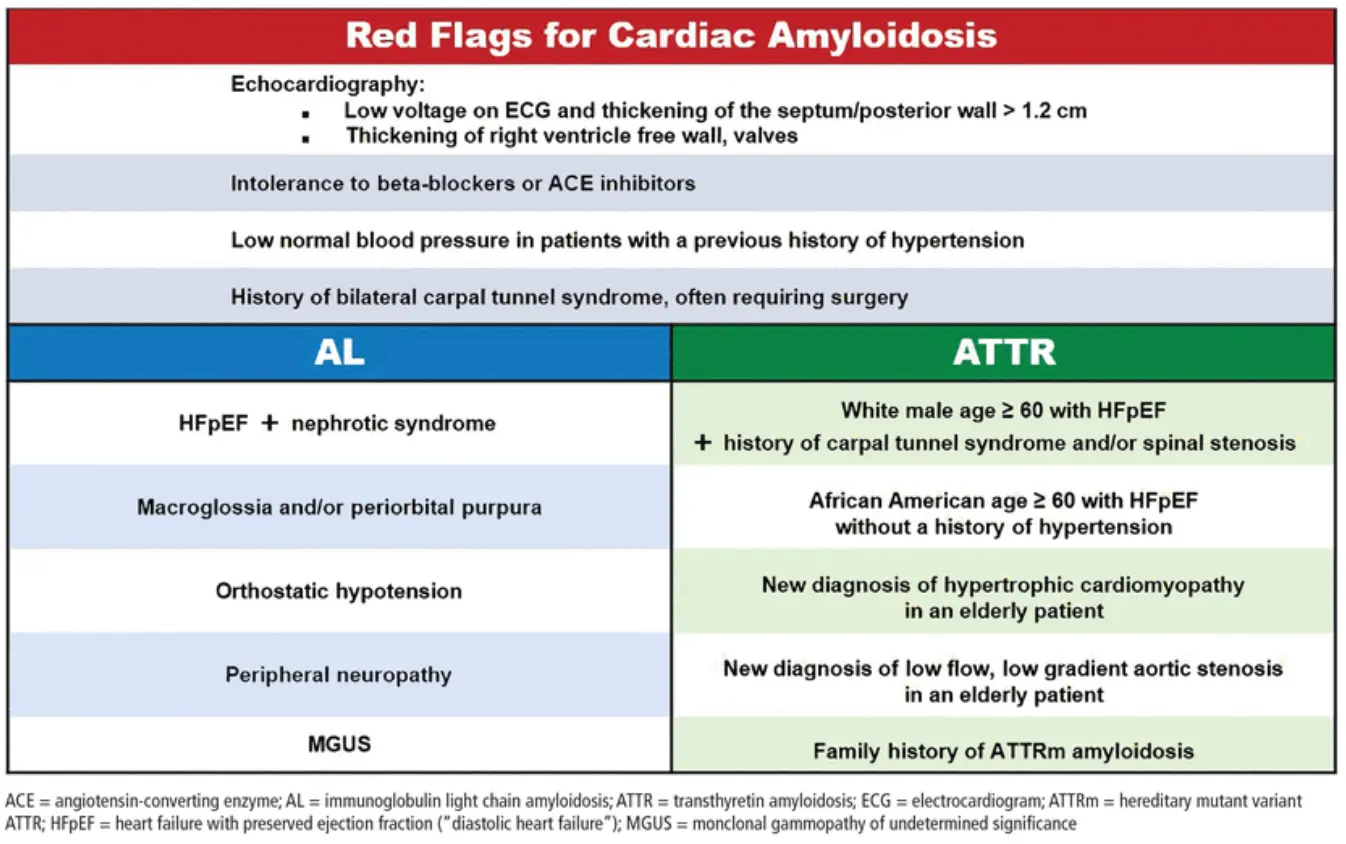
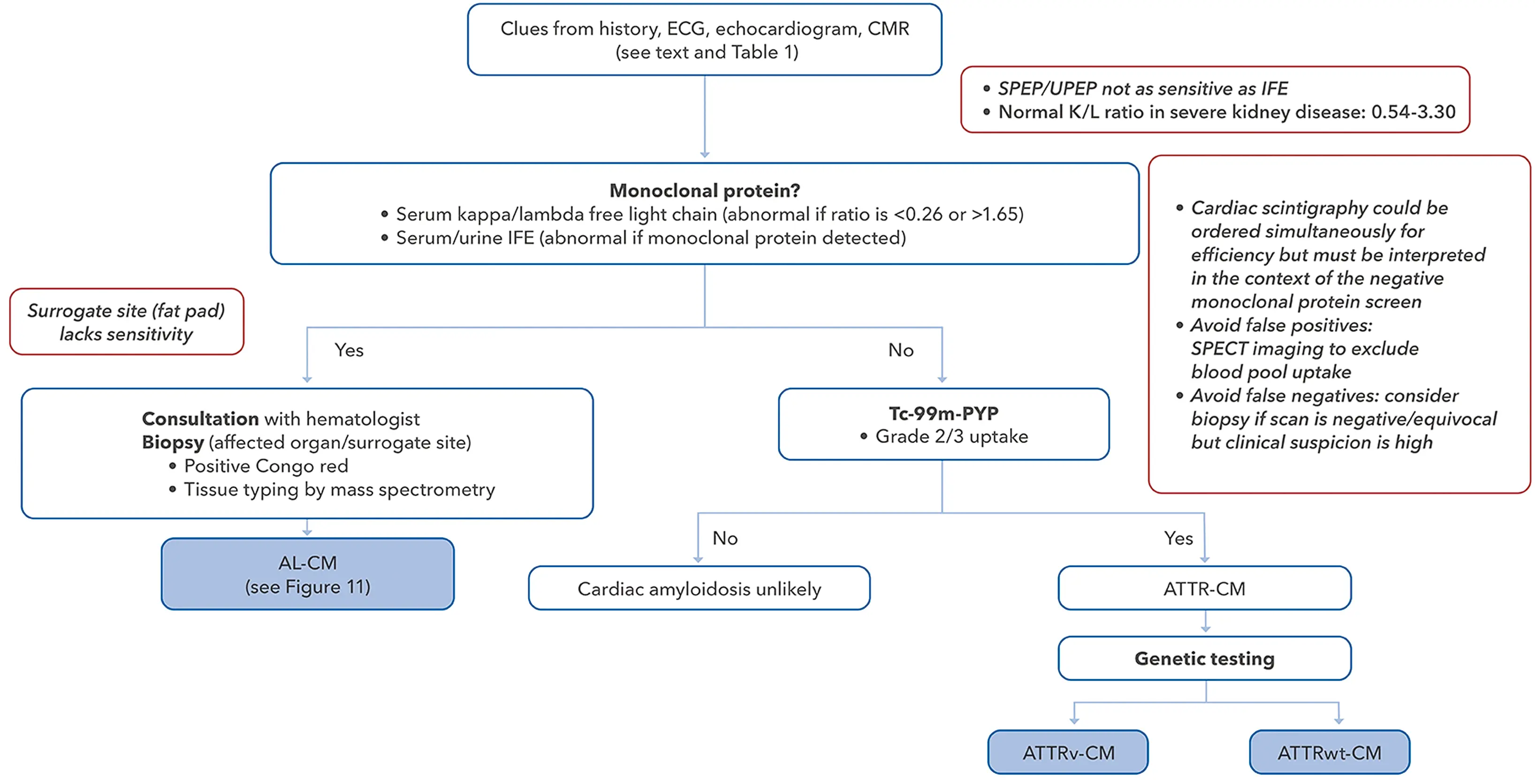 Figure source: 2
Figure source: 2
Concomitant Aortic Stenosis
- ~15% of TAVR patients have ATTR cardiac amyloid
- ~15% of ATTR cardiac amyloid patients have moderate to severe AS
- When both aortic stenosis and ATTR cardiac amyloid occur together, patients will often have low-flow, low-gradient AS because of the stiff heart’s restrictive physiology (→ low stroke volume index)
- recall, paradoxical low-flow, low-gradient AS occurs with an AVA ≤ 1.0 cm2 with ∆P < 4 m/s and MG < 40 mmHg with preserved ejection fraction (≥ 50%) and SVI < 35 mm/m2
Burnt-out Amyloid
Severe HTN is unlikely to be advanced amyloid
- If there is enough accumulation of amyloid fibrils, systolic dysfunction can occur → LV unable to adequately perfuse the brain and other organs. These patients may present with bad congestion, but also poor forward flow that is manifested in normal blood pressures despite a history of hypertension and intolerance to neurohomonal blockade, such as BBs, RAASi, etc.
- From the LVs perspective, you have poor inflow and poor outflow. ∴, ↓ SVR in such patients is not going to translate into improved flow, but rather hypOtension, AKI, and altered mentation.
- Often very challenging diuresing these patients.
Footnotes
-
Donnelly JP, Hanna M. Cardiac amyloidosis: An update on diagnosis and treatment. Cleve Clin J Med. 2017 Dec;84(12 Suppl 3):12-26. doi: 10.3949/ccjm.84.s3.02. PMID: 29257735. ↩ ↩2 ↩3 ↩4
-
Writing Committee; Kittleson MM, Ruberg FL, Ambardekar AV, Brannagan TH, Cheng RK, Clarke JO, Dember LM, Frantz JG, Hershberger RE, Maurer MS, Nativi-Nicolau J, Sanchorawala V, Sheikh FH. 2023 ACC Expert Consensus Decision Pathway on Comprehensive Multidisciplinary Care for the Patient With Cardiac Amyloidosis: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023 Mar 21;81(11):1076-1126. doi: 10.1016/j.jacc.2022.11.022. Epub 2023 Jan 23. Erratum in: J Am Coll Cardiol. 2023 Mar 21;81(11):1135. doi: 10.1016/j.jacc.2023.02.013. PMID: 36697326. ↩