- Categories:
- The term ‘incessant’ has been adopted for cases with persistent symptoms without a clear-cut remission after the acute episode.
- The term ‘chronic’ generally refers—especially for pericardial effusions—to disease processes lasting >3 months
- Recurrent pericarditis is diagnosed with a documented first episode of acute pericarditis, a symptom-free interval of 4–6 weeks or longer and evidence of subsequent recurrence of pericarditis
- recurrence rate after an initial episode of pericarditis ranges from 15 to 30%, and may increase to 50% after a first recurrence in patients not treated with colchicine, esp if Tx w/ steroids.

| Therapy | Dosing | Duration | Tapering | Monitoring | LOE |
|---|---|---|---|---|---|
| Aspirin | 500-1,000 mg 3 times daily | wks (acute) to mo (recurrent) | Weekly | Needed | A |
| Ibuprofen | 600-800 mg 3 times daily | wks (acute) to mo (recurrent) | Weekly | Needed | A |
| Indomethacin | 25-50 mg 3 times daily | wks (acute) to mo (recurrent) | Weekly | Needed | B |
| Colchicine | 0.6 mg twice daily or 0.6 mg once daily (<70 kg, severe renal/hepatic impairment) | 3 mo (acute), 6-12 mo (recurrent) | May be considered | Needed | A |
| Prednisone | 0.2-0.5 mg/kg/d | wks to mo | Several mo | Needed | B |
| Anti–IL-1 agents | |||||
| Anakinra | 1-2 mg/kg/d up to 100 mg/d in adults | >12 mo | Needed | Needed | A |
| Rilonacept | 320 mg once followed by 160 mg weekly | >12 mo | Stopping vs tapering under investigation | Needed | A |
| Goflikicept (Not yet available in United States) | 80 mg every 2 wks | >12 mo (under investigation) | Unknown | Needed | B |
| Azathioprine | Starting with 1 mg/kg per d then gradually increased to 2-3 mg/kg/d | Several mo | Several mo | Needed | C |
| IVIG | 400 to 500 mg/kg IV daily for 5 d | 5 d | Not required | Needed | C |
| Radical pericardiectomy | High-volume pericardial surgical centers | Not applicable | Not applicable | Needed | C |
| Table source: 1 |
Acute Pericarditis
# Acute pericarditis
- Work-up: CBC, ESR, CRP (abnormal if > 3 mg/L), CK, troponin (assess for epicardial inflammation; if significantly elevated consider myopericarditis), 12-lead ECG, CXR
- Consider TB testing in the appropriate context
- Echo
- If acute pericarditis and LV dysfunction, most (85%) will have recovery after 12 months
- Empiric therapy
- Aspirin 750-1,000 mg q8h for 1-2 weeks. If response, plan to taper by decreasing dose by 250-500 mg every 1-2 weeks
- Ibuprofen 600 mg q8h for 1-2 weeks. If response, plan to taper by decreasing dose by 200-400 mg every 1-2 weeks.
- 3 month course of Colchicine 0.5 mg BID (if weight > 70 kg) or 0.5 mg daily (if weight < 70 kg) (based on 2013 ICAP study)
- PPI for gastroprotection (if prescribed ASA or NSAIDs)
- Activity limitations
- If not involved in athletic sports, recommend restrict physical activity beyond ordinary sedentary life until resolution of symptoms and normalization of CRP
- If athlete, recommended to return to competitive sports only after symptoms have resolved and diagnostic tests (i.e. CRP, ECG and echocardiogram) have normalized
- Duration: Expert consensus recommends activity restriction for a minimum of 3 months for athletes, whereas a shorter period (until remission) may be suitable for non-athletes.
- Dispo: close follow-up in 1 week to assess therapeutic response
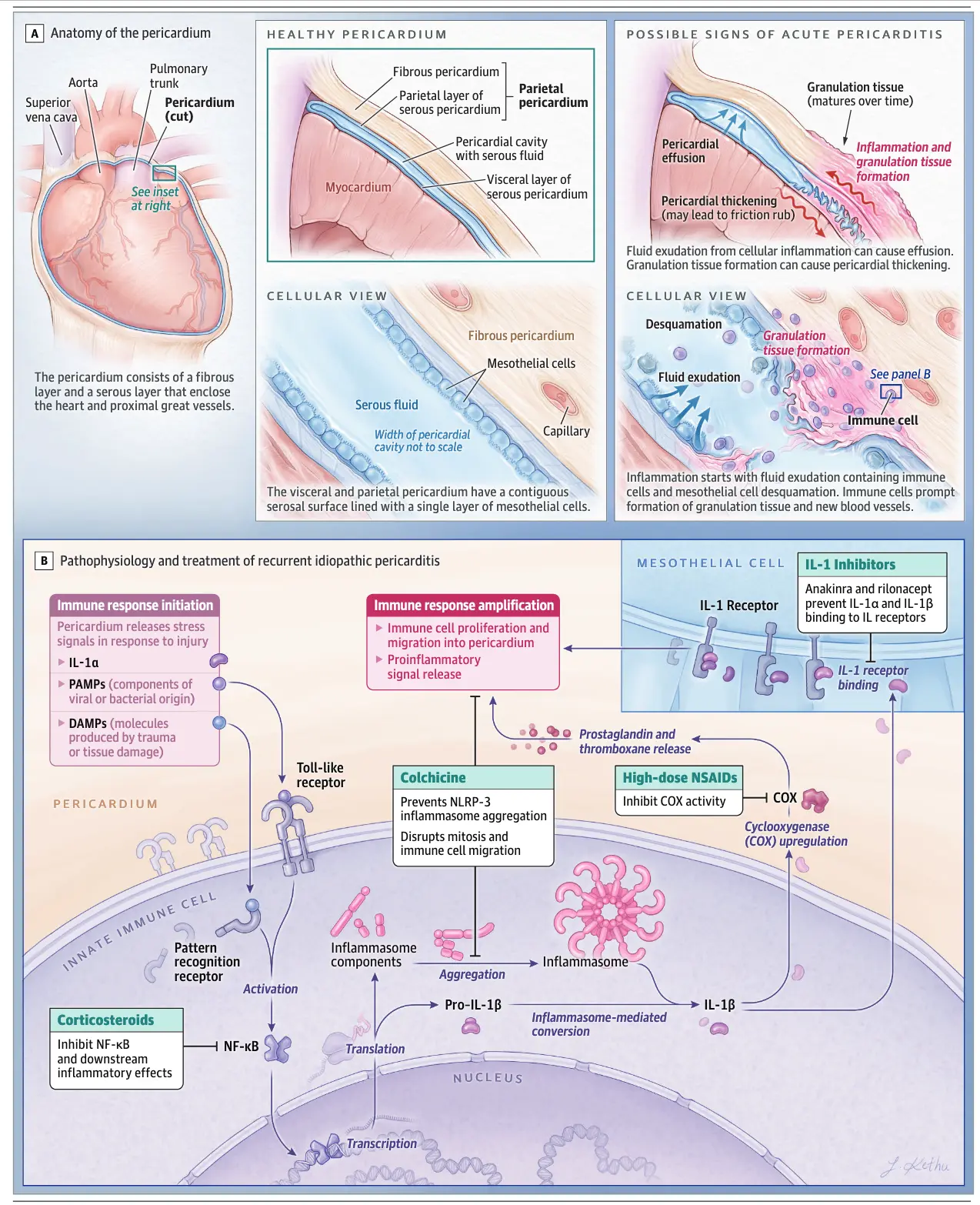
- Acute pericarditis is an inflammatory pericardial syndrome with or without pericardial effusion.
- With appropriate treatment, 70% to 85% of these patients have a benign course.2
- In acute pericarditis, the development of constrictive pericarditis (<0.5%) and pericardial tamponade (<3%) can be life-threatening.2
- Causes
- In North America and Western Europe, the most common causes of acute pericarditis are idiopathic or viral, followed by pericarditis after cardiac procedures or operations.
- Tuberculosis is the most common cause in endemic areas and is treated with antituberculosis therapy, with corticosteroids considered for associated constrictive pericarditis.
- Among patients with a malignant pericardial effusion, the most common causes are lung (≈40%), breast (≈25%), and hematologic (≈20%) malignancies.2
- Poor prognostic markers – if present, may warrant hospital admission
- Fever
- Subacute course, i.e. Sx over several days w/o a clear-cut onset
- Large pericardial effusion, i.e. diastolic echo-free space >2 cm
- Cardiac tamponade
- Failure to respond w/in 7 days to NSAIDs
Diagnosis of Acute Pericarditis
- Clinical diagnosis can be made with ≥2 of the following criteria:
- chest pain (>85–90% of cases)—typically sharp and pleuritic, improved by sitting up and leaning forward; worsens when supine
- pericardial friction rub (≤33% of cases)—a superficial scratchy or squeaking sound best heard with the diaphragm of the stethoscope 🩺 over the left sternal border
- ECG changes (up to 60% of cases)—with new widespread ST elevation or PR depression in the acute phase
- NOTE: ECG changes imply inflammation of the epicardium, since the parietal pericardium itself is electrically inert
- pericardial effusion (up to 60% of cases, generally mild)
- CRP, ESR, WBC elevation is common and may be helpful to monitor disease activity and therapeutic efficacy
- Increased markers of myocardial injury (e.g. CK, troponin) may suggest concomitant myocarditis
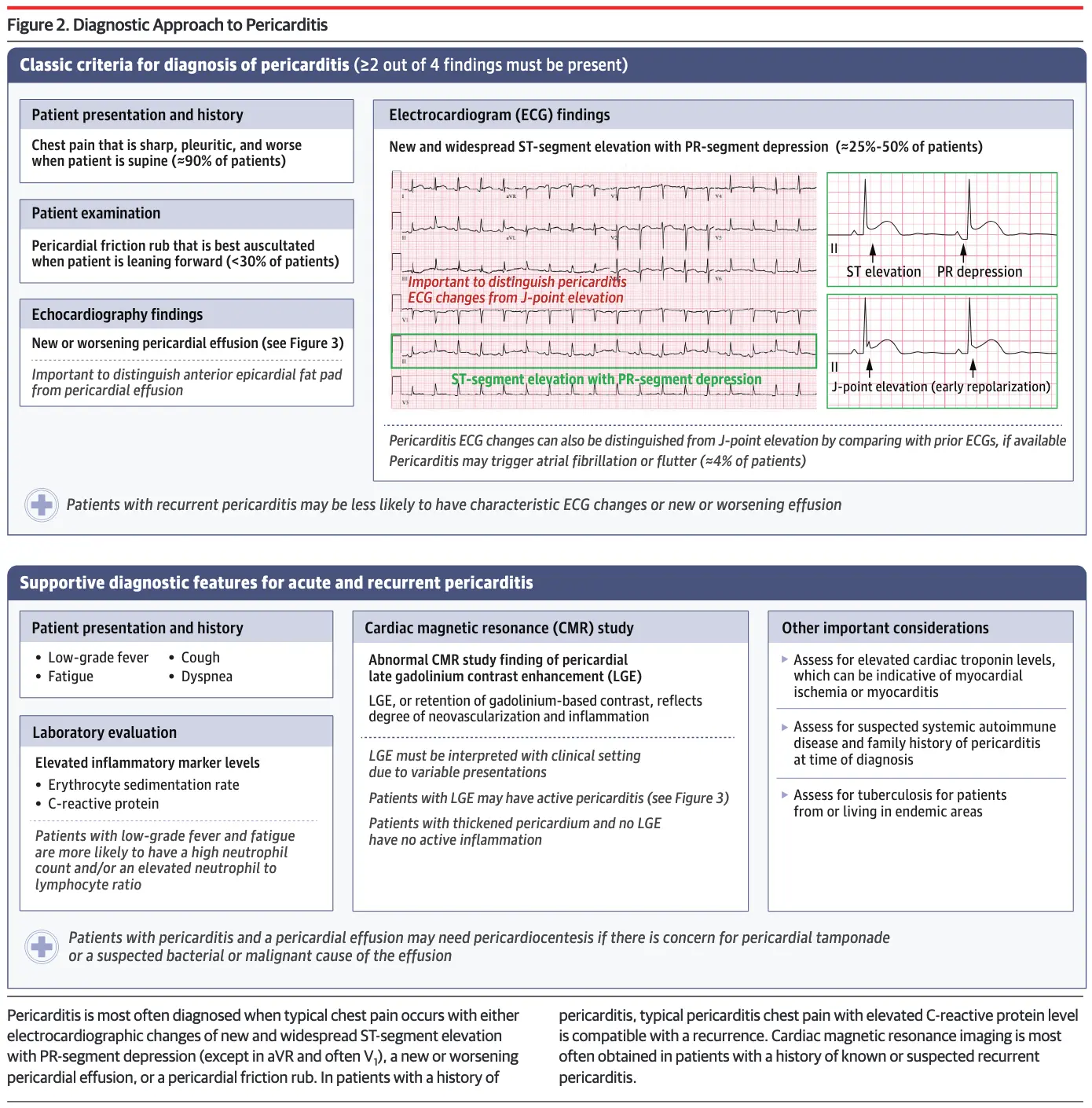
ECG in Pericarditis
You may not always seen diffuse ST-segment elevation, so absence should not exclude Dx of pericarditis.
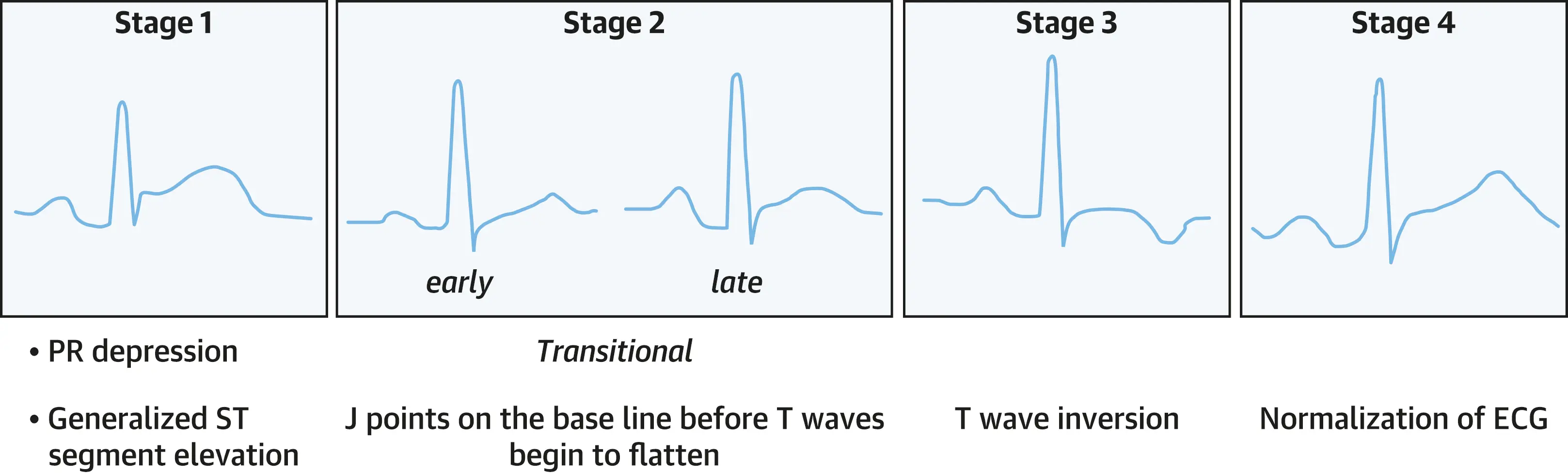 Source: 3
Source: 3
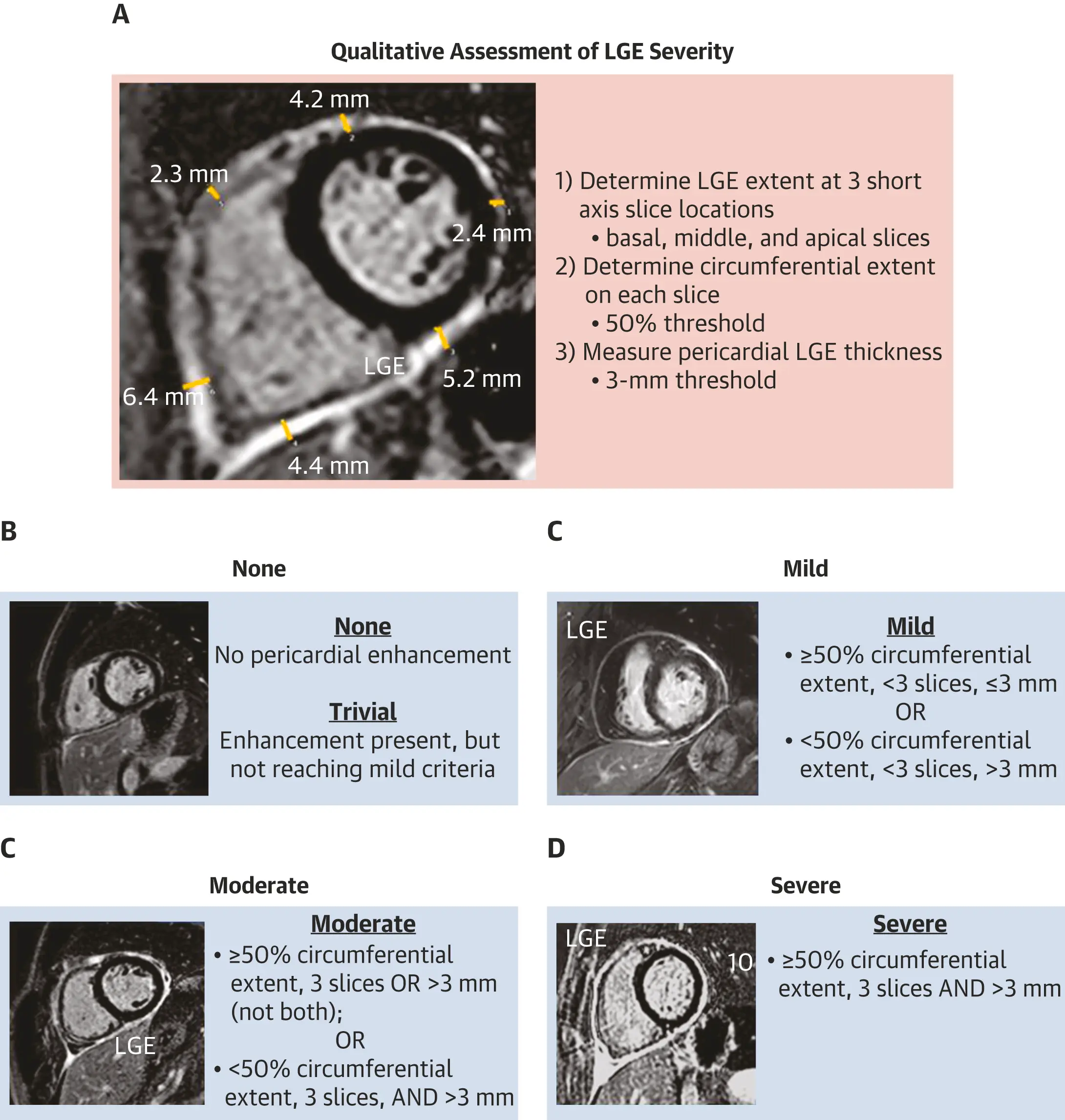
Imaging in Pericarditis
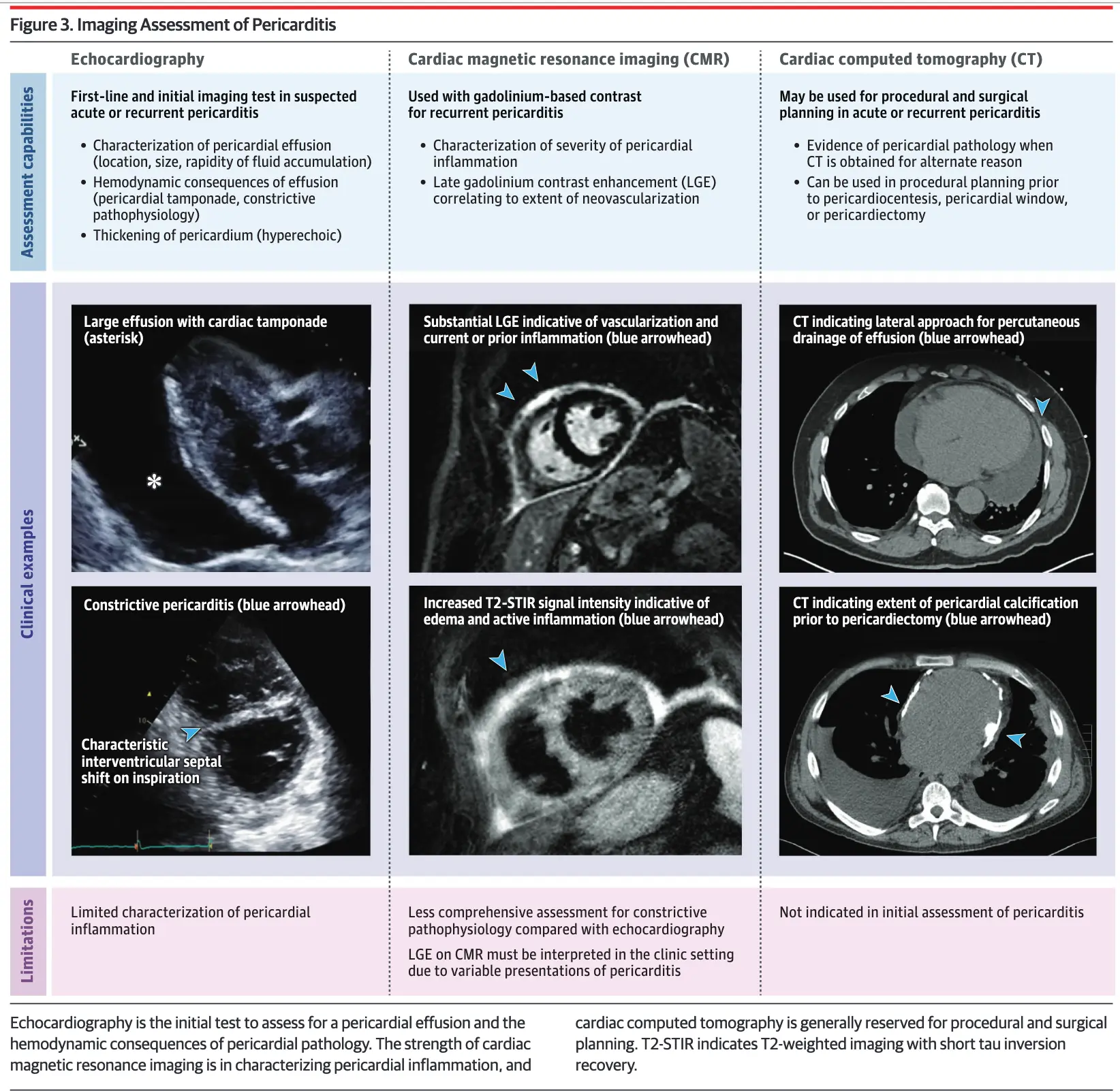
| TTE | CCT | CMR |
|---|---|---|
| ▪ Normal findings in some patients. Pericardial thickening | ▪ Noncalcified pericardial thickening (>3 mm) | ▪ Thickening of pericardium at T1-weighted BB images (>3 mm) |
| ▪ Segmental wall motion abnormalities or pathological myocardial strain values (in case of myocarditis) | ▪ Enhancement of the thickened visceral and parietal surfaces of the pericardial sac at late postcontrast CT scan | ▪ Enhancement of pericardium on LGE sequence (inflammation) and T2-STIR sequence (edema) consistent with active inflammation and neovascularization (of prognostic importance) ▪ LGE+/T2-STIR+: acute/subacute phase or recurrent flares ▪ LGE+/T2-STIR-: subacute or chronic phase ▪ LGE-/T2-STIR-: resolution or end-stage/calcific phase |
| ▪ PEff with or without Tamponade (present in 40%-50% of cases) | ▪ PEff presence. CT attenuation values of the PEff may help distinguish between exudative and transudative fluid (on noncontrast CT) | ▪ PEff presence. High signal intensity on T1-weighted BB images is suggestive of exudative PEffs |
| ▪ Sign of CP (often transient) | ▪ Loss of the normal sliding between pericardial layers during the cardiac cycle is one feature consistent with pericarditis | |
| Table source: 1 |
Figure source: 1
Management of Acute Pericarditis
Table source: 4
| Drug | Usual Dosing | Tx Duration | Tapering |
|---|---|---|---|
| Aspirin | 750-1,000 mg q8h | 1-2 wks | ↓ dose by 250-500 mg every 1-2 wks |
| Ibuprofen | 600 mg q8h | 1-2 wks | ↓ dose by 200-400 mg every 1-2 wks |
| Colchicine | 0.5 mg daily (< 70 kg) or 0.5 mg BID (≥ 70 kg) | 3 months | Not mandatory, alternatively 0.5 mg every other day (< 70 kg) or 0.5 mg once (270 kg) in the last weeks |
- Treatment of acute idiopathic and pericarditis after cardiac procedures or operations involves use of high-dose nonsteroidal anti-inflammatory drugs (NSAIDs), with doses tapered once chest pain has resolved and CRP level has normalized, typically over several weeks. These patients should receive a 3-month course of colchicine to relieve symptoms and reduce the risk of recurrence (37.5% vs 16.7%; absolute risk reduction, 20.8%).2
- Empiric therapy
- Aspirin 750-1,000 mg q8h for 1-2 weeks. If response, plan to taper by decreasing dose by 250-500 mg every 1-2 weeks
- Ibuprofen 600 mg q8h for 1-2 weeks. If response, plan to taper by decreasing dose by 200-400 mg every 1-2 weeks.
- Colchicine 0.6 mg BID (if weight > 70 kg) or 0.5 mg daily (if weight < 70 kg). Often prescribed as adjunct to Aspirin/NSAID. Tapering is not mandatory.
- Contraindicated if severe renal impairment, pregnant/lactating women
- 📝 Steroids only used if contraindications and failure to ASA/NSAIDs. If used, low to moderate doses (i.e. prednisone 0.2-0.5 mg/kg/day or equivalent) should be recommended instead of high doses (i.e. prednisone 1.0 mg/kg/day or equivalent). initial dose should be maintained until resolution of symptoms and normalization of CRP, then tapering should be considered.
- ⚠️ In observational studies, corticosteroids, especially at higher doses (eg, prednisone [1.0 mg/kg daily]), have been associated with an increased risk of recurrence of pericarditis. ∴, corticosteroids should only be prescribed at low to moderate doses (prednisone [0.25-0.5 mg/kg daily]) in patients who do not improve with NSAIDS and colchicine or have adverse outcomes with or contraindications to NSAIDs and colchicine. 2
- PPI for gastroprotection (if prescribed ASA or NSAIDs)
- Activity limitations
- If not involved in athletic sports, recommend restrict physical activity beyond ordinary sedentary life until resolution of symptoms and normalization of CRP
- If athlete 🏃, recommended to return to competitive sports only after symptoms have resolved and diagnostic tests (i.e. CRP, ECG and echocardiogram) have normalized
- Duration: Expert consensus recommends activity restriction for a minimum of 3 months for athletes, whereas a shorter period (until remission) may be suitable for non-athletes.
- Dispo: close follow-up in 1 week to assess therapeutic response
Incessant Pericarditis
- Incessant pericarditis is defined by symptoms lasting at least 4 to 6 weeks but less than 3 months without remission.2
- 20% of patients with incessant pericarditis develop constrictive pericarditis 2
Recurrent Pericarditis
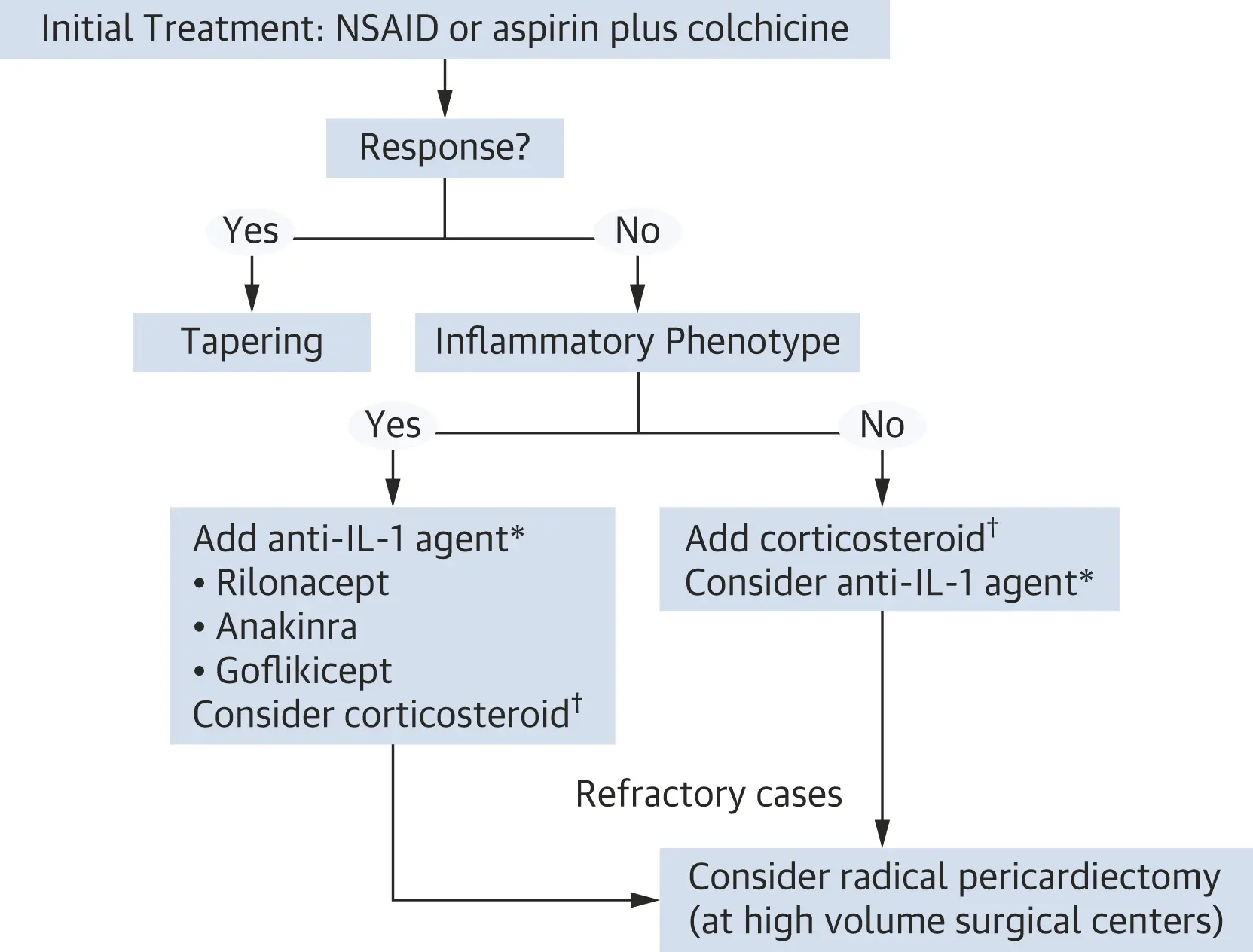 Algorithm source: 1
Algorithm source: 1

- Try to target underlying etiology (if identifiable cause present)
- Aspirin or NSAIDs remain the mainstay of therapy + Colchicine as adjunct
- If incomplete response to ASA/NSAID + colchicine combo, then can consider steroids as an add-on to low-/moderate-dose ASA/NSAID + colchicine, i.e. ‘triple therapy’
- See ESC 2015 guidelines for recommendations on tapering steroid therapy

- Drugs such as IVIG, anakinra and azathioprine may be considered in cases of proven infection-negative, corticosteroid-dependent, recurrent pericarditis not responsive to colchicine after careful assessment of the costs, risks and eventually consultation by multidisciplinary experts, including immunologists and/or rheumatologists, in the absence of a specific expertise. It is also mandatory to educate the patient and his/her caregivers about the clinical risks related to immunomodulatory/immunosuppressive drugs and the safety measures to adopt during the treatment.
- As a last resort, pericardiectomy may be considered, but only after a thorough trial of unsuccessful medical therapy, and with referral of the patient to a centre with specific expertise in this surgery.
Chronic Pericarditis
Footnotes
-
Wang TKM, Klein AL, Cremer PC, Imazio M, Kohnstamm S, Luis SA, Mardigyan V, Mukherjee M, Ordovas K, Vakamudi S, Wohlford GF. 2025 Concise Clinical Guidance: An ACC Expert Consensus Statement on the Diagnosis and Management of Pericarditis: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2025 Jul 31:S0735-1097(25)06503-9. doi: 10.1016/j.jacc.2025.05.023. Epub ahead of print. PMID: 40767817. ↩ ↩2 ↩3 ↩4
-
Cremer PC, Klein AL, Imazio M. Diagnosis, Risk Stratification, and Treatment of Pericarditis: A Review. JAMA. 2024;332(13):1090–1100. doi:10.1001/jama.2024.12935 ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7
-
Chiabrando JG, Bonaventura A, Vecchié A, Wohlford GF, Mauro AG, Jordan JH, Grizzard JD, Montecucco F, Berrocal DH, Brucato A, Imazio M, Abbate A. Management of Acute and Recurrent Pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jan 7;75(1):76-92. doi: 10.1016/j.jacc.2019.11.021. PMID: 31918837. ↩
-
Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. European Heart Journal. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318 ↩