History
- Living Situation
- Independent living: 5% prevalence
- Nursing Home: 70% prevalence
- Food ingestion
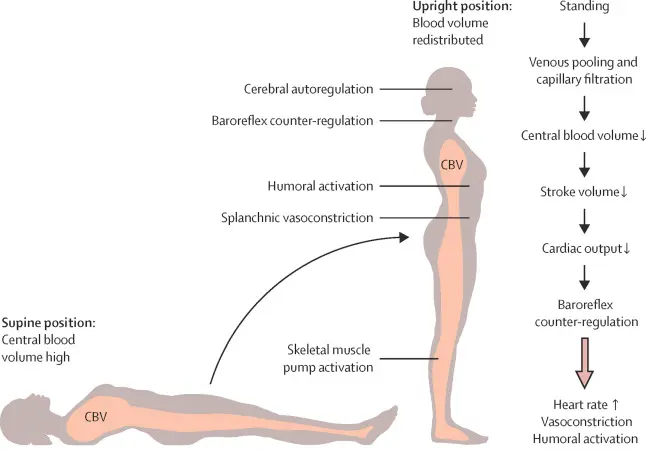
- Orthostatic hypotension worsens with large meals (high carbs) and EtOH
- Pooling of blood in the splanchnic circulation
- Vasodilatation from insulin and vasoactive peptides
- Orthostatic hypotension worsens with large meals (high carbs) and EtOH
- Hydration status
- Usually worse with dehydration or in the morning
Diagnosis
📝 the diagnosis is hemodynamic and NOT based on symptoms
- Symptomatic postural decrease in BP
- SBP ≥ 20 mmHg or DBP ≥ 10 mmHg (usually within 3 minutes)
- Diagnosis made whether symptomatic or asymptomatic
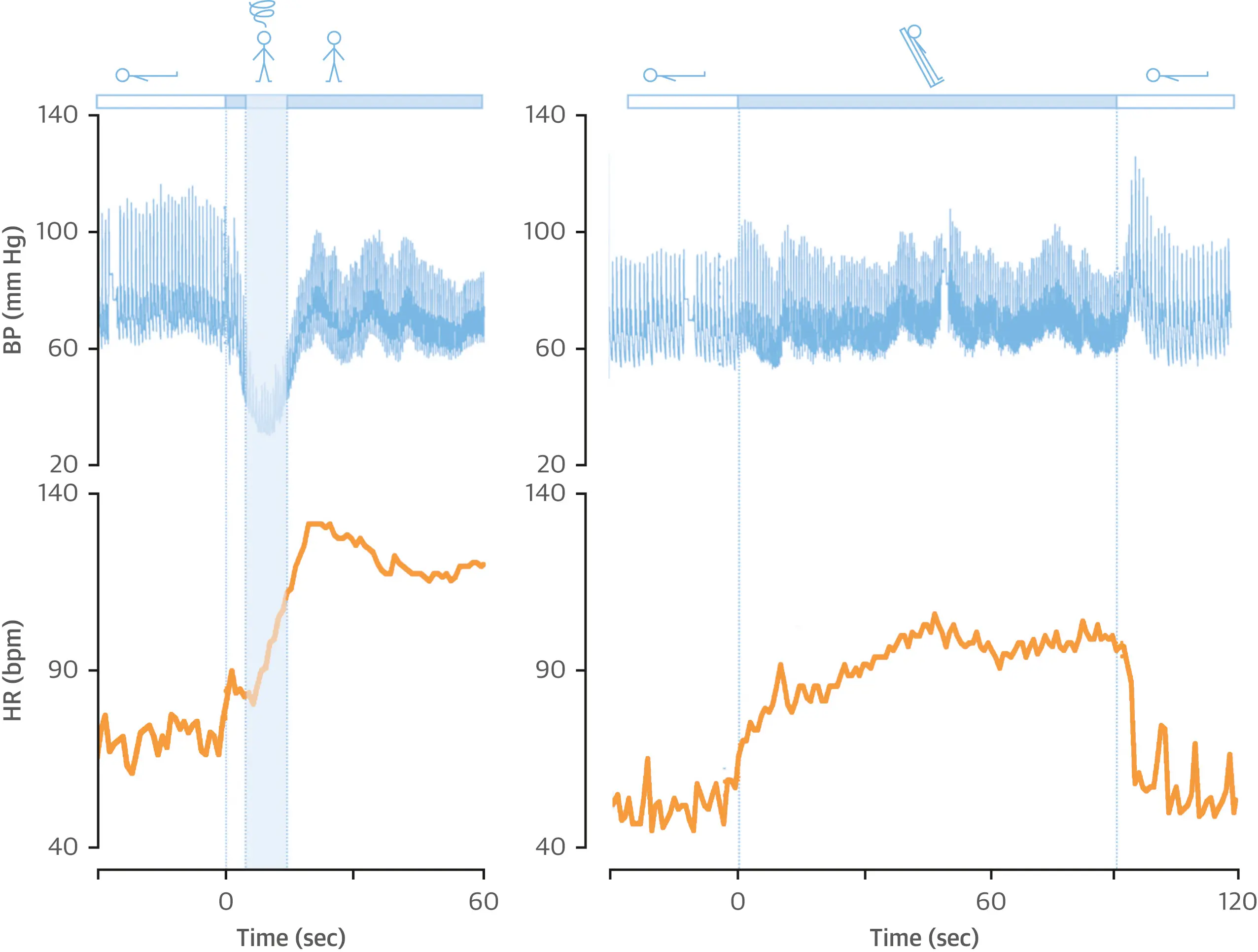
- Closely related to changes in position
- Lying → Sitting
- Sitting → Standing
- Time Frame of Symptom onset
- 📝 Typically the HR increment is minimal 2
Etiologies
Non-Reversible
- Secondary Autonomic Failure / Peripheral neuropathy
- Diabetes
- Severity and duration of diabetes does not correlate to severity of OH
- Alcoholism
- Chemotherapy
- HIV
- Paraneoplastic syndromes (small cell lung CA most commonly)
- Amyloidosis
- B12 deficiency (reversible)
- Guillain Barre (recovers over time)
- Vasculitis
- Diabetes
- Primary Autonomic Failure / Neurodegenerative disorders
- ~27% of moderate-severe OH have primary autonomic failure
- Parkinson disease (20 - 60% prevalence of OH)?
- Rigidity, resting tremor, shuffling gait
- Responds to levodopa
- Lewy body dementia
- Parkinsonism with dementia, cognitive impairments, usually more severe OH
- Multiple system atrophy
- CNS: Parkinsonian and cerebellar variants, with urinary incontinence and constipation, ED
- Does not respond to levodopa (usually)
- Pure autonomic failure (Bradbury-Eggleston)
- PNS: Diffuse autonomic issues with slow heart rate, urinary incontinence, ED, difficulty sweating
Management
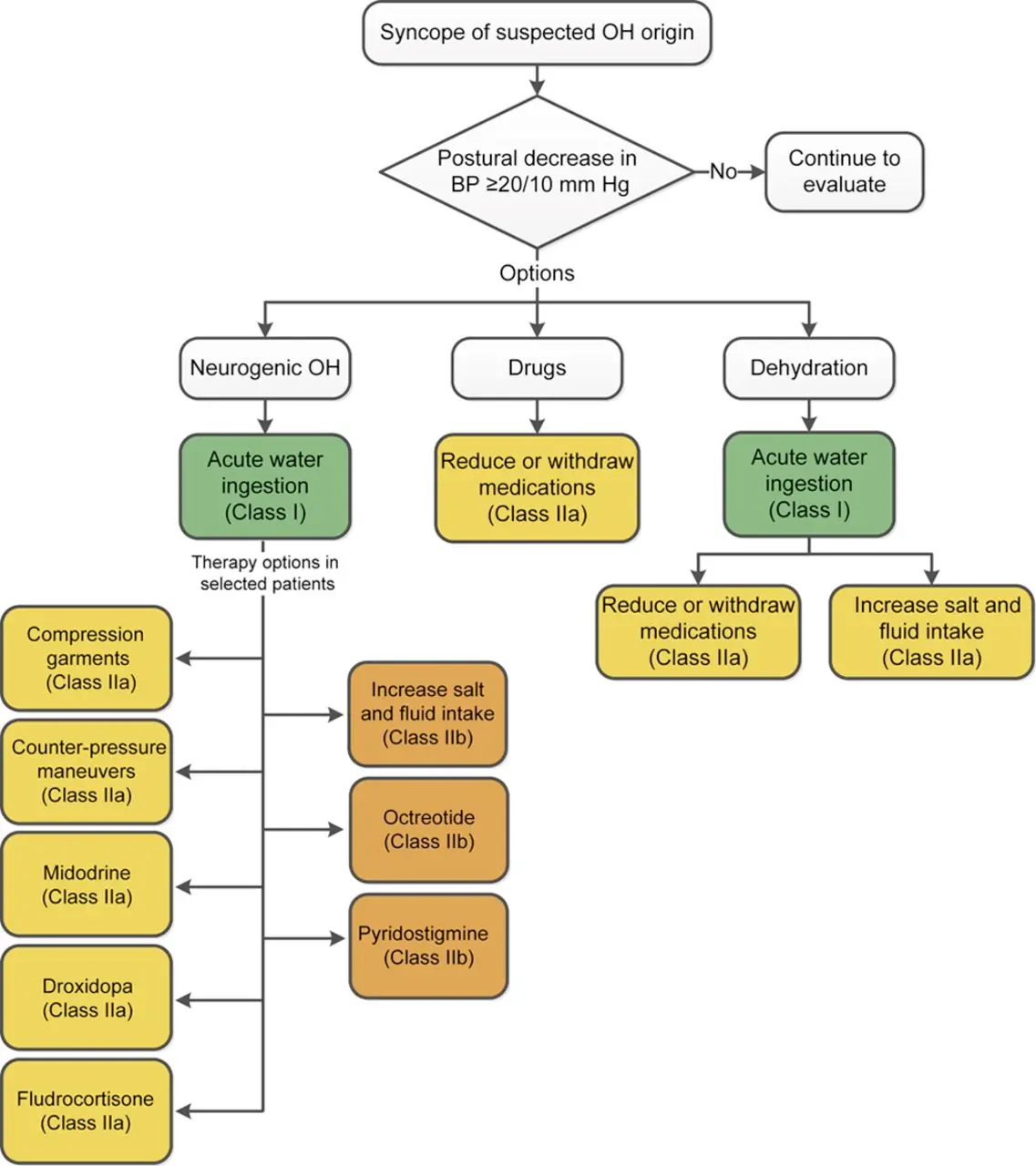
- Liberalize salt and fluid
- Consider fluid bolus
- Compression hose (higher is better)
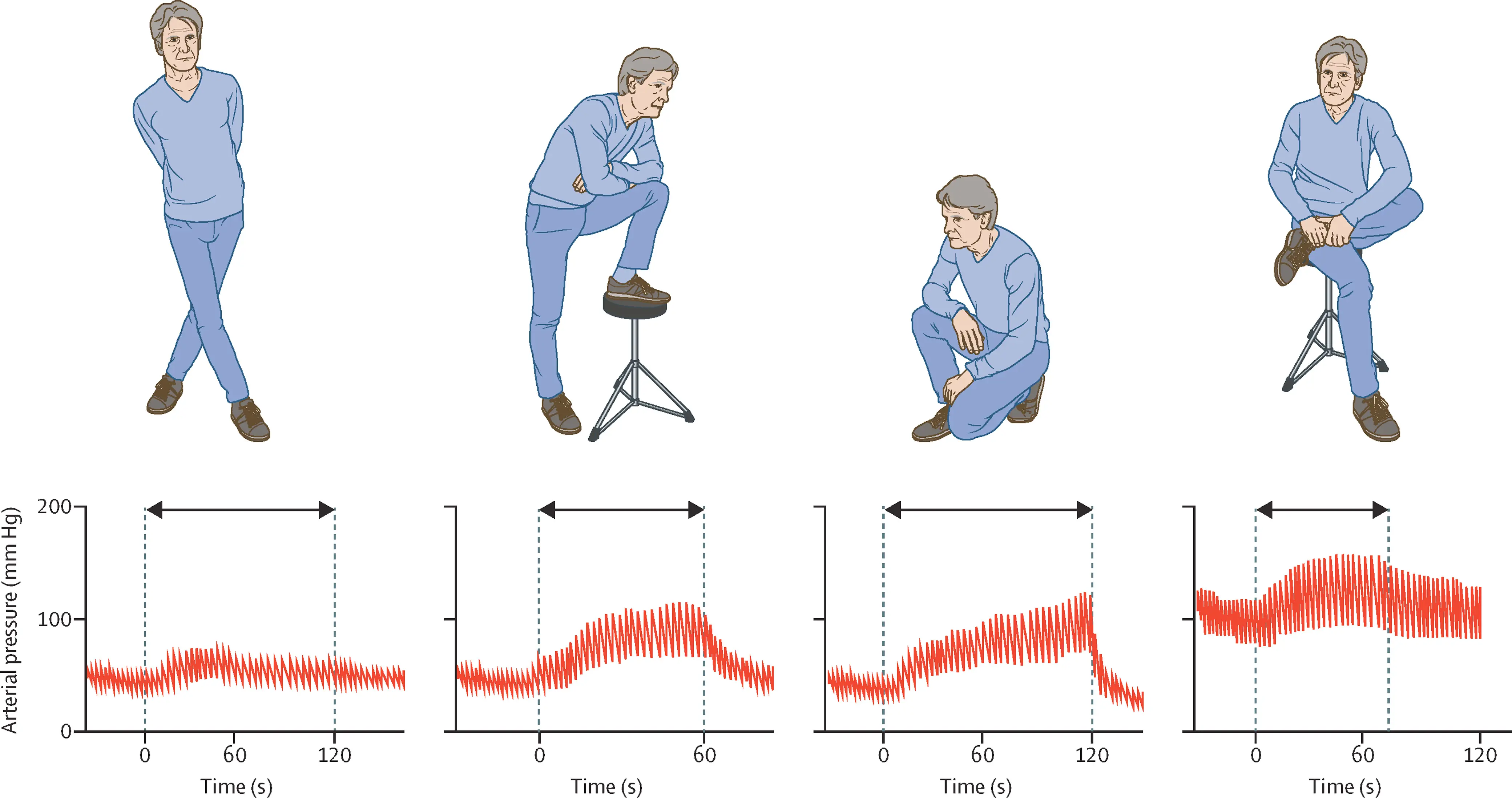
- Counterpressure maneuvers, e.g. leg crossing, limb and/or abdominal contraction, squatting
- Stop offending medication(s)
- Commonly used medications (hidden sympatholytics) can worsen orthostatic hypotension (e.g. tizanidine, trazodone, tamsulosin).
- Consider fludrocortisone (0.1 mg daily)
- Consider midodrine (5 mg TID)
- Consider droxidopa (100 mg TID)
- refer to EP or Autonomic Neurology
- To read:
Footnotes
-
Freeman, Roy, et al. “Orthostatic Hypotension.” Journal of the American College of Cardiology, vol. 72, no. 11, Sept. 2018, pp. 1294–309. DOI.org (Crossref), https://doi.org/10.1016/j.jacc.2018.05.079. ↩ ↩2
-
Bryarly M, Phillips LT, Fu Q, Vernino S, Levine BD. Postural Orthostatic Tachycardia Syndrome: JACC Focus Seminar. J Am Coll Cardiol. 2019 Mar 19;73(10):1207-1228. doi: 10.1016/j.jacc.2018.11.059. PMID: 30871704. ↩
-
Park JW, Okamoto LE, Shibao CA, Biaggioni I. Pharmacologic treatment of orthostatic hypotension. Auton Neurosci 2020;229:doi: 10.1016/j.autneu.2020.102721. ↩
-
Gibbons CH, Schmidt P, Biaggioni I, et al. The recommendations of a consensus panel for the screening, diagnosis, and treatment of neurogenic orthostatic hypotension and associated supine hypertension. J Neurol 2017;264:1567-82. ↩