- ExECG has a positive likelihood ratio of 2.18 and a negative likelihood ratio of 0.32 for CAD1
- Involves graded exercise until physical fatigue, limiting chest pain (or discomfort), marked ischemia, or a drop in blood pressure occurs.2
- Goal is at least 4-6 minutes of exercise to allow for maximal metabolic demand
- METS needs to be ≥5 for stress study to be interpretable (ask Talal for citation)
- Adequate workload in a patient undergoing stress ECG testing is defined as ≥5 METS
- Ideally, tests should be symptom limited (i.e. not “done” when patient reaches 85% of max-predicted HR)
- Candidates for exercise ECG are those:2
- without disabling comorbidity (e.g., frailty, marked obesity (BMI >40 kg/m2), PAD, COPD, or orthopedic limitations) and capable of performing ADLs or able to achieve ≥5 METs and
- without resting ST-T abnormalities (e.g., >0.5-mm ST depression, LVH, paced rhythm, LBBB, WPW pattern, or digoxin use).
- Confounders such as resting ST-segment depression, digoxin usage, and LVH with repolarization changes decrease specificity. Despite these confounders, ExECG is still considered diagnostic in most patients able to reach 85% of their maximum age-predicted heart rate.1
- Indications
- ischemic evaluation
- chronotropic incompetence
- exercise induced arrhythmias
- valve disease, e.g. severe aortic stenosis
- Options:
- Treadmill
- Recumbent bicycle
- Protocols (Bruce, modified Bruce, Naughton)
- Contraindications
- Abnormal ST changes on resting ECG, digoxin, LBBB, WPW pattern, ventricular paced rhythm (unless test is performed to establish exercise capacity and not for diagnosis of ischemia)
- LVH, LBBB, digoxin effect, V-paced rhythm, pre-excitation/WPW pattern, resting ST abnormalities, ?RBBB (V1-V3, the rest of the leads are interpretable though) as these would be uninterpretable based on ECG assessment alone
- Unable to achieve ≥5 METs or unsafe to exercise
- High-risk unstable angina or AMI (<2 d) i.e., active ACS
- Uncontrolled HF
- Significant cardiac arrhythmias (e.g., VT, complete atrioventricular block) or high risk for arrhythmias caused by QT prolongation
- Severe symptomatic aortic stenosis
- Severe systemic arterial hypertension (e.g., ≥200/110 mm Hg)
- Acute illness (e.g., acute PE, acute myocarditis/pericarditis, acute aortic dissection)
- Abnormal ST changes on resting ECG, digoxin, LBBB, WPW pattern, ventricular paced rhythm (unless test is performed to establish exercise capacity and not for diagnosis of ischemia)
- Widely available and inexpensive
- Interpretable ECG
- Requires ability to exercise to an adequate level
- Who should you test?
- Intermediate-risk ASx adults (including considering starting a vigorous exercise program), particularly when attention is paid to exercise capacity
- Limited diagnostic accuracy
- sensitivity ~60% & specificity ~70%
- Avoid if pre-existing ECG abnormalities
- What are you looking for?
- See slide
- Prognostic importance of functional capacity
- Once > 10 METS your prognosis, regardless of whether you have CAD or not, is quite good)

- Figure source: 📄 Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise Capacity and Mortality among Men Referred for Exercise Testing. New England Journal of Medicine. 2002;346(11):793-801. doi:10.1056/nejmoa011858
- Value add of Coronary Artery Calcium (CAC) Score
- See 📄 Chang SM, Nabi F, Xu J, et al. Value of CACS Compared With ETT and Myocardial Perfusion Imaging for Predicting Long-Term Cardiac Outcome in Asymptomatic and Symptomatic Patients at Low Risk for Coronary Disease. JACC: Cardiovascular Imaging. 2015;8(2):134-144. doi:10.1016/j.jcmg.2014.11.008

Baseline ECG abnormalities
- Resting STD ≥1 mm
- digoxin usage
- LBBB
- require vasodilator MPI imaging due to a high false-positive rate
- WPW pattern
- Ventricular paced rhythm (unless test is performed to establish exercise capacity and not for diagnosis of ischemia)
Stress ECG Interpretation
- Abnormal responses to exercise on stress include:
- Heart rate fails to rise above 120 bpm or unable to attain 85% of MPHR
- Drop in systolic BP
- Physically unable to complete test
- Marked hypertension, >220/110
- Chest Pain and/or unusual shortness of breath
ST segments
- Review of ST segment - “positive” response is indicated by:
- ST segment depression (horizontal or downsloping) of > 1mm
- 80 msec from the J-point
- ST segment elevation in leads lacking Q-waves
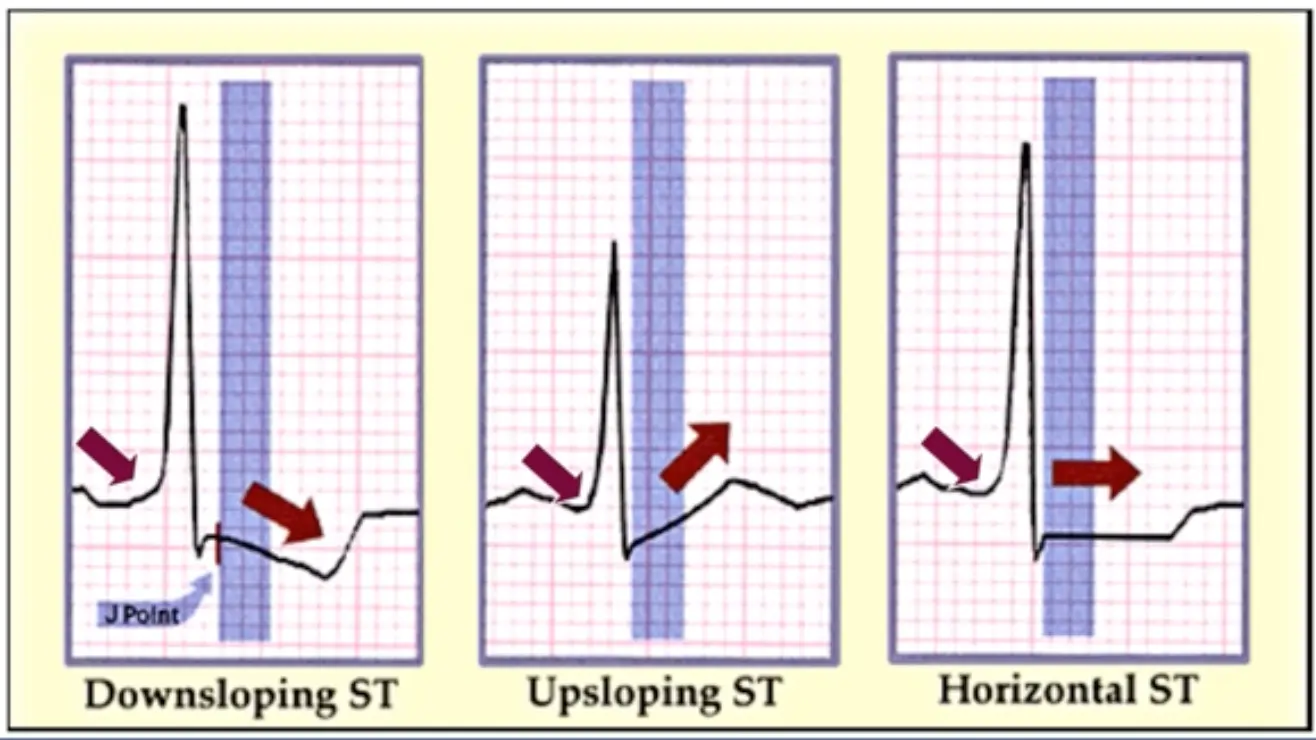
- ST segment depression (horizontal or downsloping) of > 1mm
- ST-segment elevation in lead aVR1
- Lead aVR is often neglected in ExECG interpretation but has unique vector positioning. This allows it to function as a “pseudo-intracavitary” lead that may identify anterior wall transmural ischemia.
- Uthamalingam et al. found a ≥1 mm aVR elevation during ExECG to be the strongest predictor of an obstructive LM or ostial LAD artery stenosis with a diagnostic accuracy of 80% and a 2.6-fold increase in post-test probability.
- Presence of arrhythmias
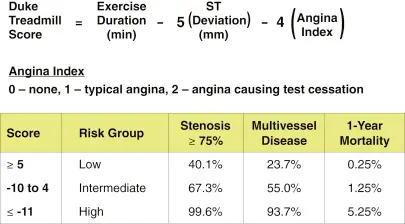
Duke Treadmill Score
Chronotropic Response
- If HR <80-ish%, cannot say completely negative test
- Heller et al. found that reaching only 70% compared with ≥85% of maximum age-predicted heart rate leads to a reduction in the incidence of stress defects from 100% to 47% and a reduction in angina from 84% to 26%.
- Exercise ECG is considered diagnostic if able to achieve ≥85% MPHR
- If unable to achieve 80% of MPHR, can call is “chronotropic incompetence”
Prognostic Features
Failure to achieve target HR
Exercise capacity
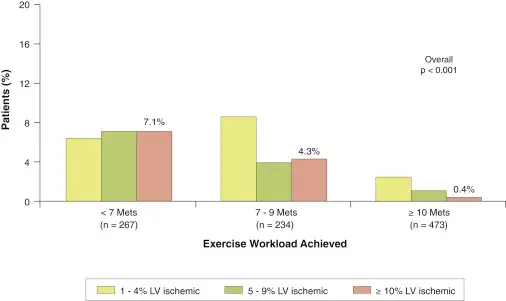
- Patients achieving ≥10 METs on ExECG have a very low prevalence of inducible ischemia and an excellent prognosis1
- High exercise workload is also a marker of a decreased risk of cardiac events, including cardiac death, nonfatal MI, and coronary revascularization. These associations remain even in the setting of ischemic ST-segment depression.1
- Bourque et al. found that patients attaining <7 metabolic equivalents (METs) had an 18-fold higher prevalence of substantial (≥10%) LV ischemia compared with those reaching ≥10 METs. The latter group with good exercise tolerance had a very low (0.4%) prevalence of ≥10% LV ischemia.1
Post-exercise
Abnormal heart rate recovery
- <12 bpm HR drop 1 min post-exercise (1 min into recovery)
- Cole et al. found a relative risk of death of 2.0 (95% confidence interval: 1.5 to 2.7; p < 0.001) for those with a <12-beats/min heart rate drop 1 min post-exercise after risk factor adjustment in 2,428 patients1
- <22 bpm HR drop 1 min post-exercise
- A retrospective analysis of 2,193 men found a heart rate recovery <22 beats/min at 2 min to be predictive of mortality and the presence of CAD1
- 📝 O’Keefe mentioned that this is a reflection of vagal tone (i.e., healthy hearts will have healthy vagal tone), and he will often use ≥ 20 bpm reduction at 2 minutes b/c practically 1 minute is not always captured well.
Abnormal blood pressure recovery
- SBP ≥15% by 3 min post-exercise
- An abnormal SBP recovery ratio of >0.9 (SBP at 3 min/SBP at peak exercise) has been found to have comparable diagnostic accuracy to ST-segment depression and incremental value for the identification of CAD1
- correlates with the extent and severity of thallium-201 perfusion defects
- An abnormal SBP recovery ratio of >0.9 (SBP at 3 min/SBP at peak exercise) has been found to have comparable diagnostic accuracy to ST-segment depression and incremental value for the identification of CAD1
-
10-mm Hg SBP drop during exercise and a delayed decline in SBP after exercise have been associated with high-risk multivessel or left main disease in men with less specificity in women
Indications for Early Termination of Exercise
- Moderate to severe angina pectoris
- Excessive STD (horizontal or downsloping) >2 mm from baseline in a patient with suspected ischemia
- STE (>1.0 mm) in leads without diagnostic Q-waves (except for leads V1 or aVR).
- Sustained SVT or VT
- Development of symptomatic second- or third-degree AV block without functioning pacemaker
- Development of LBBB or IVCD that cannot be distinguished from VT
- Signs of poor perfusion (cyanosis and pallor)
- Hypertensive response (SBP >230 mmHg and/or DBP >115 mmHg)
- Severe hypotension (SBP <80 mmHg)
- Drop in SBP of >10 mmHg from baseline, despite an increase in workload, when accompanied by other evidence of ischemia
- Inability to monitor the ECG or BP
- In patients with ICDs, when the heart rate attained is within 20 bpm of the lowest heart rate at which therapy (antitachycardia pacing or shock) is programmed to be delivered
- Patient’s request to stop
Footnotes
-
Bourque JM, Beller GA. Value of Exercise ECG for Risk Stratification in Suspected or Known CAD in the Era of Advanced Imaging Technologies. JACC Cardiovasc Imaging. 2015 Nov;8(11):1309-21. doi: 10.1016/j.jcmg.2015.09.006. PMID: 26563861; PMCID: PMC4646721. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9
-
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain. Journal of the American College of Cardiology. 2021;78(22):e187-e285. doi:10.1016/j.jacc.2021.07.053 ↩ ↩2