Chest pain
- Initial troponin ***
- Continue to trend troponins to peak every 1-3 hrs for hsTn (3-6 hrs if conventional troponin assays)
- ECG: ***
- If nondiagnostic, consider serial ECGs to detect potential ischemic changes including if CP recurs or clinical deterioration
- CXR to r/o other potential cardiac, pulmonary, and thoracic causes
- Optimize GDMT/anti-anginal therapy (if known CAD)
- Work-up to exclude other causes of CPChest Pain
-20240923102638720.webp) Schema source
Schema source
- Description of chest pain can be helpful1
- Anginal symptoms gradually build in intensity over a few minutes.
- Triggers
- physical exercise
- emotional stress
- Associated symptoms include dyspnea, palpitations, diaphoresis, lightheadedness, presyncope or syncope, upper abdominal pain, or heartburn unrelated to meals and nausea or vomiting 1
- ⚠️ Relief with nitroglycerin is not necessarily diagnostic of myocardial ischemia and should not be used as a diagnostic criterion.
-20240923100504827.webp)
- Differential diagnosis
- Sharp chest pain that increases with inspiration and lying supine is unlikely related to ischemic heart disease (e.g., these symptoms usually occur with acute pericarditis) 1
- Sudden onset of ripping chest pain (with radiation to the upper or lower back) is unlikely to be anginal and is suspicious of an acute aortic syndrome (e.g., aortic dissection).1
- Ripping chest pain (“worse chest pain of my life”), especially when sudden in onset and occurring in a hypertensive patient, or with a known bicuspid aortic valve or aortic dilation, is suspicious of an acute aortic syndrome (e.g., aortic dissection).
- Pain that can be localized to a very limited area and pain radiating to below the umbilicus or hip are unlikely related to myocardial ischemia.1
- Positional chest pain is usually nonischemic (e.g., musculoskeletal)1
- Pain, pressure, tightness, or discomfort in the chest, shoulders, arms, neck, back, upper abdomen, or jaw, as well as shortness of breath and fatigue should all be considered anginal equivalents.1
- ⚠️ Avoid the term ‘atypical chest pain’. Instead, use “cardiac,” “possible cardiac,” and “noncardiac” to describe the suspected cause of chest pain1
- Anginal equivalents (e.g., new-onset/↑ DOE, nausea/vomiting, diaphoresis, unexplained fatigue, or syncope) may occur in those who are…
- older (e.g., ≥75 years of age)
- female
- diabetes mellitus
- renal dysfunction
- dementia
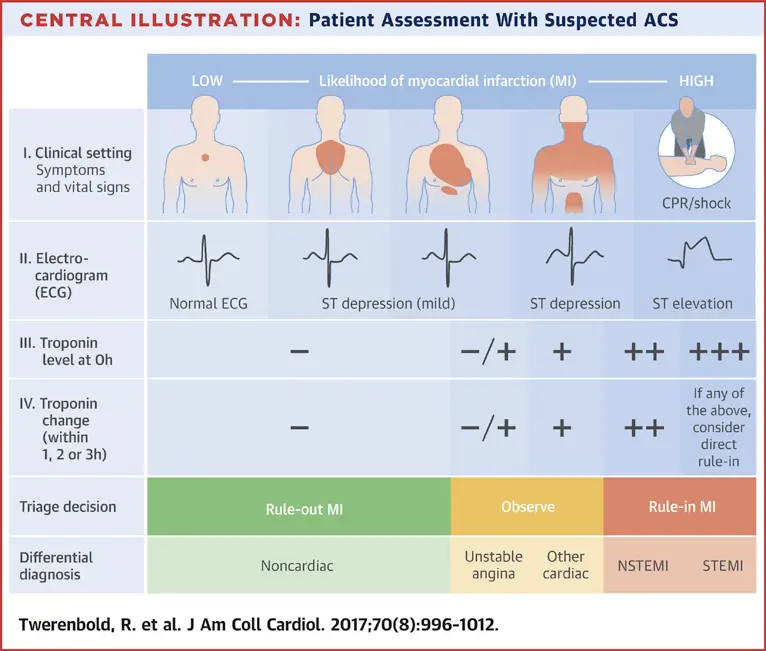 Figure source: 2
Figure source: 2
Non-cardiac causes of chest pain
- Respiratory
- Pulmonary Embolism
- Pneumothorax/hemothorax
- Pneumomediastinum
- Pneumonia
- Bronchitis
- Pleural irritation
- Malignancy
- GI
- Cholecystitis
- Pancreatitis
- Hiatal hernia
- Gastroesophageal reflux disease/gastritis/esophagitis
- Peptic ulcer disease
- Esophageal spasm
- Dyspepsia
- MSK
- Costochondritis
- Chest wall trauma or inflammation
- Herpes zoster (shingles)
- Cervical radiculopathy
- Breast disease
- Rib fracture
- Musculoskeletal injury/spasm
- Pain disorder
- Panic disorder
- Anxiety
- Clinical depression
- Somatization disorder
- Hypochondria
- Other
- Hyperventilation syndrome
- Carbon monoxide poisoning
- Sarcoidosis
- Lead poisoning
- Prolapsed intervertebral disc
- Thoracic outlet syndrome
- Adverse effect of certain medications (e.g., 5-fluorouracil)
- Sickle cell crisis
Unstable angina
| Class | Presentation |
|---|---|
| Rest angina | Angina occuring at rest and prolonged, usually > 20 minutes. |
| New-onset angina | New-onset angina of at least CCS class III severity. |
| Increasing angina | Previously diagnosed angina that has become distinctly more frequent, longer duration, or lower in threshold (i.e., increased by 1 or more CCS class to at least CCS class III severity) |
Risk Scores for Patient Stratification
- Clinical Decision Pathways are useful to identify low risk patients for early discharge
- Serial troponins in HEART Pathway, EDACS, ADAPT, etc
- For example, if HEART score < 3 and normal evaluation patient may be able to be discharged and have outpatient eval.
| HEART Pathway | EDACS | ADAPT (mADAPT) | NOTR | 2020 ESC/hs-cTn | 2016 ESC/GRACE | |
|---|---|---|---|---|---|---|
| Target population | Suspected ACS | Suspected ACS, CP >5 min, planned serial troponin | Suspected ACS, CP >5 min, planned observation | Suspected ACS, ECG, troponin ordered | Suspected ACS, stable | Suspected ACS, planned serial troponin |
| Target outcome | ↑ ED discharge without increasing missed 30-d or 1-y MACE | ↑ ED discharge rate without increasing missed 30-d MACE | ↑ ED discharge rate without increasing missed 30-d MACE | ↑ Low-risk classification without increasing missed 30-d MACE | Early detection of AMI; 30-d MACE | Early detection of AMI |
| Patients with primary outcome in study population, % | 6–22 | 12 | 15 | 5–8 | 9.8 | 10–17 |
| Troponin | cTn, hs-cTn | hs-cTn | cTn, hs-cTn | cTn, hs-cTn | hs-cTn | cTn, hs-cTn |
| Variables used | History ECG Age Risk factors Troponin (0, 3 h) | Age Sex Risk factors History Troponin (0, 2 h) | TIMI score 0-1 No ischemic ECG changes Troponin (0, 2 h) | Age Risk factors Previous AMI or CAD Troponin (0, 2 h) | History ECG hs-cTn (0, 1 or 2 h) | Age HR, SBP Serum Cr Cardiac arrest ECG Cardiac biomarker Killip class |
| ![[Acute Coronary Syndromes (ACS)-20240923121531173.webp | 758]] |
HEART Score
- Helps determine who will benefit from hospital 🏥 admission
- Low (0-3), Medium (4-6), or High (7-10) Risk for 30-Day MACE
-20250112123911174.webp)
Cardiac Testing
Test selection should be based on patient risk and pre-test likelihood of CAD and may be influenced by site expertise and availability1
1 recommends using clinical decision pathways (CDPs) to categorize patients into low-, intermediate-, and high-risk.
-20240923103358028.webp)
Intermediate-risk Patients
Intermediate Risk and no known CAD
-20240923121936870.webp) Figure source: Figure 9 of 1
Figure source: Figure 9 of 1
Intermediate Risk with known CAD
- High-risk CAD features include:
- left main disease
- proximal LAD disease
- multivessel CAD
- Class 1 indication for invasive coronary angiography for a patient with intermediate-risk p/w acute chest pain with high-risk CAD.
-20240923122835996.webp) Figure source: Figure 10 of 1
Figure source: Figure 10 of 1
Selection of Stress Imaging versus CCTA
- Related:
- Cardiac Stress Testing
- Coronary Computed Tomography Angiography (CCTA)
- Stress Imaging
- Stress Echocardiography
- Stress Cardiac MRI
- Nuclear Stress: PET, SPECT
-20240923103654377.webp)
Footnotes
-
Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain. Journal of the American College of Cardiology. 2021;78(22):e187-e285. doi:10.1016/j.jacc.2021.07.053 ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9 ↩10 ↩11 ↩12
-
Twerenbold R, Boeddinghaus J, Nestelberger T, Wildi K, Rubini Gimenez M, Badertscher P, Mueller C. Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction. J Am Coll Cardiol. 2017 Aug 22;70(8):996-1012. doi: 10.1016/j.jacc.2017.07.718. PMID: 28818210. ↩