| Emergent (Immediate followup) | Urgent (may need workup/followup) | Non-urgent – may or may not need followup |
|---|---|---|
| Aortic Dissection | Possible new malignancy | Granulomatous disease (e.g. sarcoid) |
| Pneumothorax, Pneumomediastinum | Lymphadenopathy | Cystic lung disease |
| Pulmonary Embolism | Esophageal thickening | Fibrotic lung disease |
| Infection (TB, empyema, abscess) | Pulmonary edema | Known malignancy (has prior studies) |
| Hemorrhage | Large pleural effusion | Other chronic lung disease |
| Fracture | Pulmonary nodules |
- Review the scout images!
- Lower neck
- Thyroid
- Chest wall
- Breast
- Musculoskeletal
- Bone: compression fx? rib fx?
- Lungs
- Parenchyma
- Pleura
- Vessels
- Pulmonary arteries - filling defect suggestive of PE? You may not always have adequate contrast in the pulmonary arterial system; should be ≥200 HU to make a confident diagnosis. If you see a filling defect, trace it back to make sure it’s not in a pulmonary vein segment.
- Aorta
- Type A or B dissection - not type of dissection, extent of flap, and potential complications
- Aortic size - use double oblique technique to get a true measure
- Mediastinum
- Anterior - normally will just be composed of fat, small ≤1.5 cm lymph nodes, and vessels
- tl;dr: any mass in the anterior mediastinum requires further w/u
- Middle
- Trachea
- Esophagus, GE junction
- Lymph nodes (also 👀 in axillae and hila)
- Posterior
- Anterior - normally will just be composed of fat, small ≤1.5 cm lymph nodes, and vessels
- Upper abdomen
- Adrenal
- Kidney
- Liver
- Pancreas
- Hernias?
Nice resource: 1
CHEST:
The thyroid gland is unremarkable. The chest wall is unremarkable. There is no significant adenopathy noted in the axillae, mediastinum, and hila. Lung windows reveal no acute abnormalities. Patent airways. There is no pleural effusion.
The pericardium and pulmonary arteries appear normal. There is no central or lobar pulmonary artery thrombus. Assessment of the distal branches is limited.
The cardiac chambers demonstrate normal atrioventricular and ventriculoarterial concordance, and systemic and pulmonary venous return. The cardiac chamber sizes are normal. There is no LV myocardial thinning. There is no significant mitral annular calcification. The left atrial appendage is unremarkable. The coronary arteries have normal origins and courses. There are no distinct coronary calcifications, though this study was not optimized for coronary artery evaluation.
UPPER ABDOMEN:
The limited images of the upper abdomen reveal no abnormalities of the visualized organs.
BONES:
No destructive osseous lesions.Simpler:
CHEST:
The chest wall, mediastinum, and pericardium are unremarkable. The pulmonary arteries appear normal. No significant adenopathy is identified in the axilla, mediastinum, and hila.
Lung windows reveal no acute abnormalities. There is no pulmonary parenchymal mass, infiltrate, or pleural effusion.
The cardiac chambers demonstrate normal atrioventricular and ventriculoarterial concordance, and systemic and pulmonary venous return. The cardiac chamber sizes appear normal. There is no LV myocardial thinning.. There is no significant mitral annular calcification.Lower neck
Thyroid Gland
Normal CT appearance of the thyroid gland: (Source)
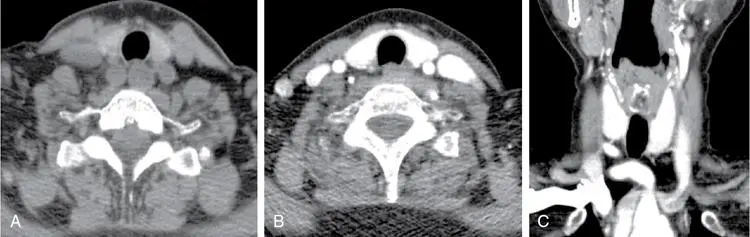 Non-contrast axial CT images (A) shows a normal hyperdense thyroid gland relative to the adjacent skeletal muscles. Contrast axial (B) and coronal (C) images shows intense enhancement of the thyroid gland.
Non-contrast axial CT images (A) shows a normal hyperdense thyroid gland relative to the adjacent skeletal muscles. Contrast axial (B) and coronal (C) images shows intense enhancement of the thyroid gland.
Example of thyroid lesion that underwent further work-up. 1

Lungs
Use lung windows and mediastinal windows
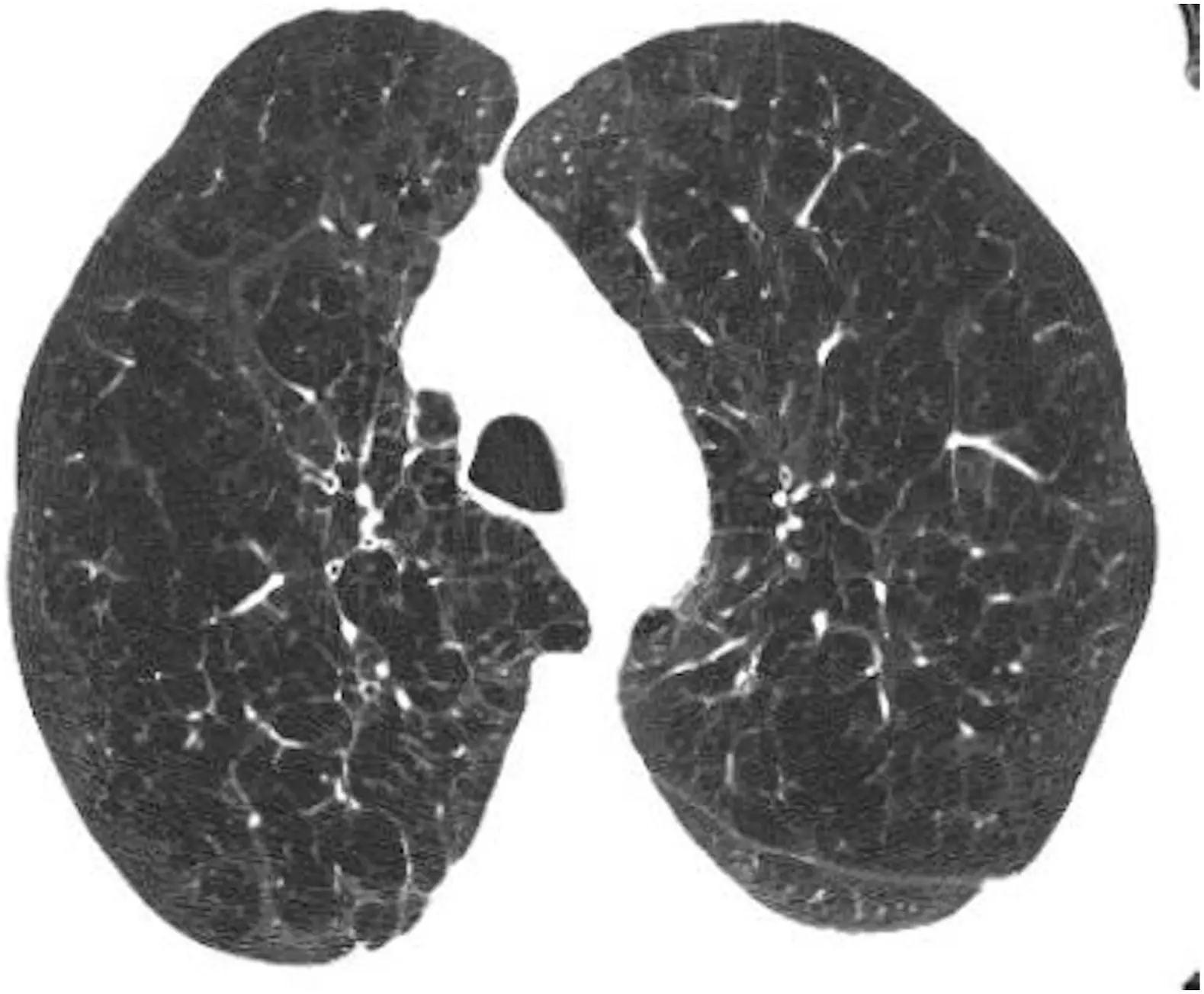
- Emphysema
- Bronchiectasis
- Interstitial lung disease (other than pulmonary fibrosis)
- Ground-glass opacification
- Pulmonary fibrosis
- Pulmonary nodules
Pulmonary Nodules
- Updated 2017 Fleischner society guidelines raised the size threshold for incidental lung nodule followup resulting in substantially less future testing (MacMahon 2017)
- Applies to:
- Incidental nodules
- Solid nodules ≤6 mm in low-risk adults generally need no further follow-up. In higher-risk patients, a follow-up CT scan should be considered optional.
- ⚠️ Does NOT apply to age < 35, immunocompromised or known malignancy.
Lung examples
Emphysema
Breast
- Coarse calcifications - OK.
- Cyst with no associated solid component - OK.
- ⚠️ Any other nodule/mass or asymmetric density
- Recommend w/u, e.g. diagnostic mammogram +/- US.
Musculoskeletal
- Degenerative disc disease
-
130 HU at L1 - OK.
- ⚠️ 100-130 HU at L1 (Osteopenia) → consider PCP evaluation.
- ⚠️ < 100 HU at L1 (Osteoporosis) → PCP evaluation and consider DEXA.
Mediastinum
Esophagus, GE junction
- Normal esophageal wall is thin.
- CT is a poor method to evaluate the esophagus secondary to underdistention.
- If thickening if present, consider nonemergent barium esophagram or endoscopy.
Example: 75 y/o with asymmetric thickening of esophagus prompting endoscopy → Dx: Carcinoma.
Example: 67 year old male with diffuse symmetric thickening of esophagus → Dx: Carcinoma
Upper Abdomen
Adrenals
- Adrenal calcification - OK.
- Nodule < 10 HU (fat density), likely adenoma - OK.
- Soft tissue density nodule < 1 cm - OK.
- Adrenal nodule stable ≥ 1 year - OK.
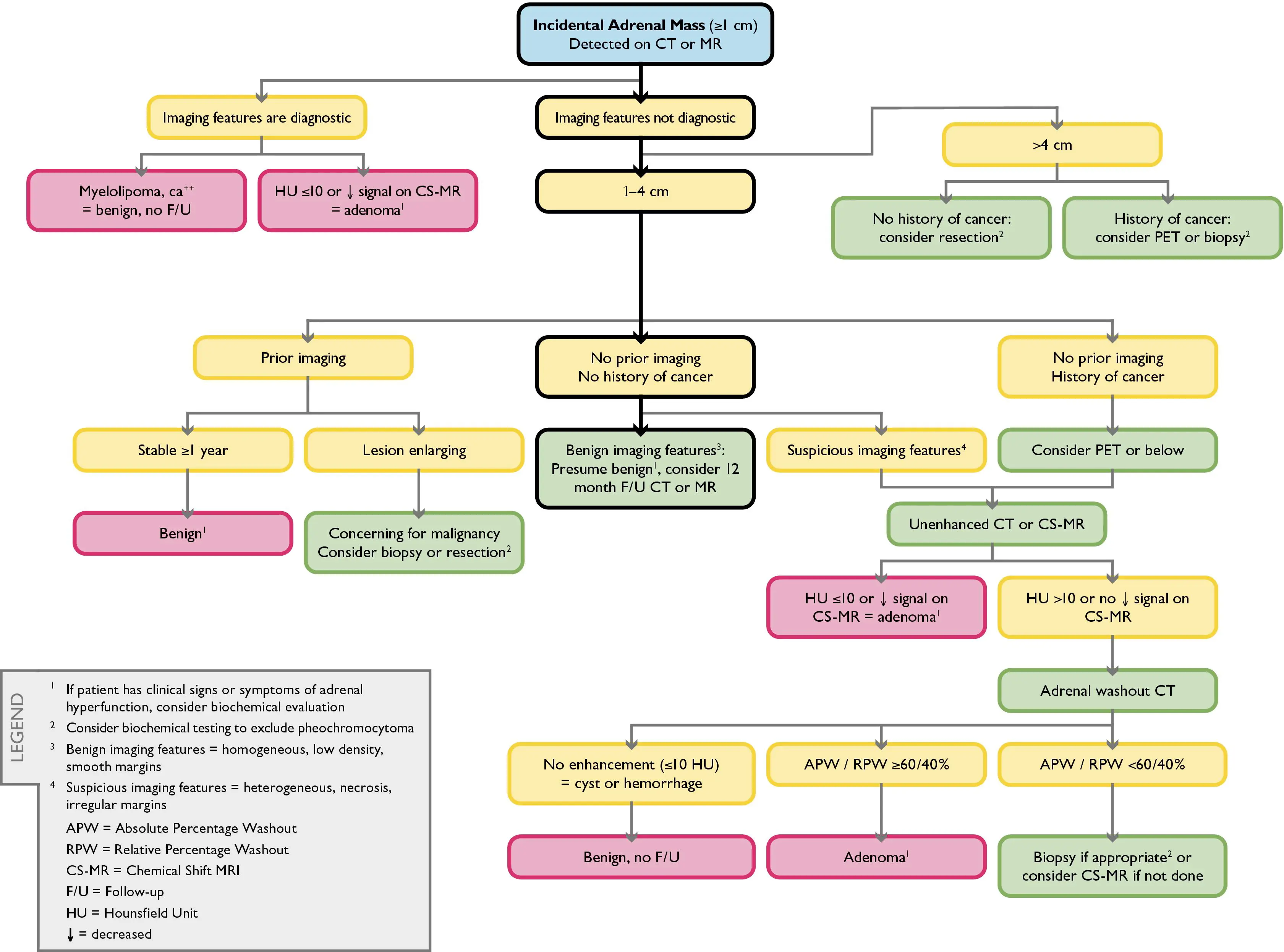 Algorithm source: 2
Algorithm source: 2
Kidneys
- Non-obstructing renal calculi - OK.
- Simple or hyperdense/hemorrhagic cyst (“Bosniak 1 or 2”) < 4 cm - OK.
- ⚠️ Soft tissue density (or mixed density) renal mass
- Recommend further work-up with CT or MRI of the kidneys without and with IV contrast.
Renal cyst
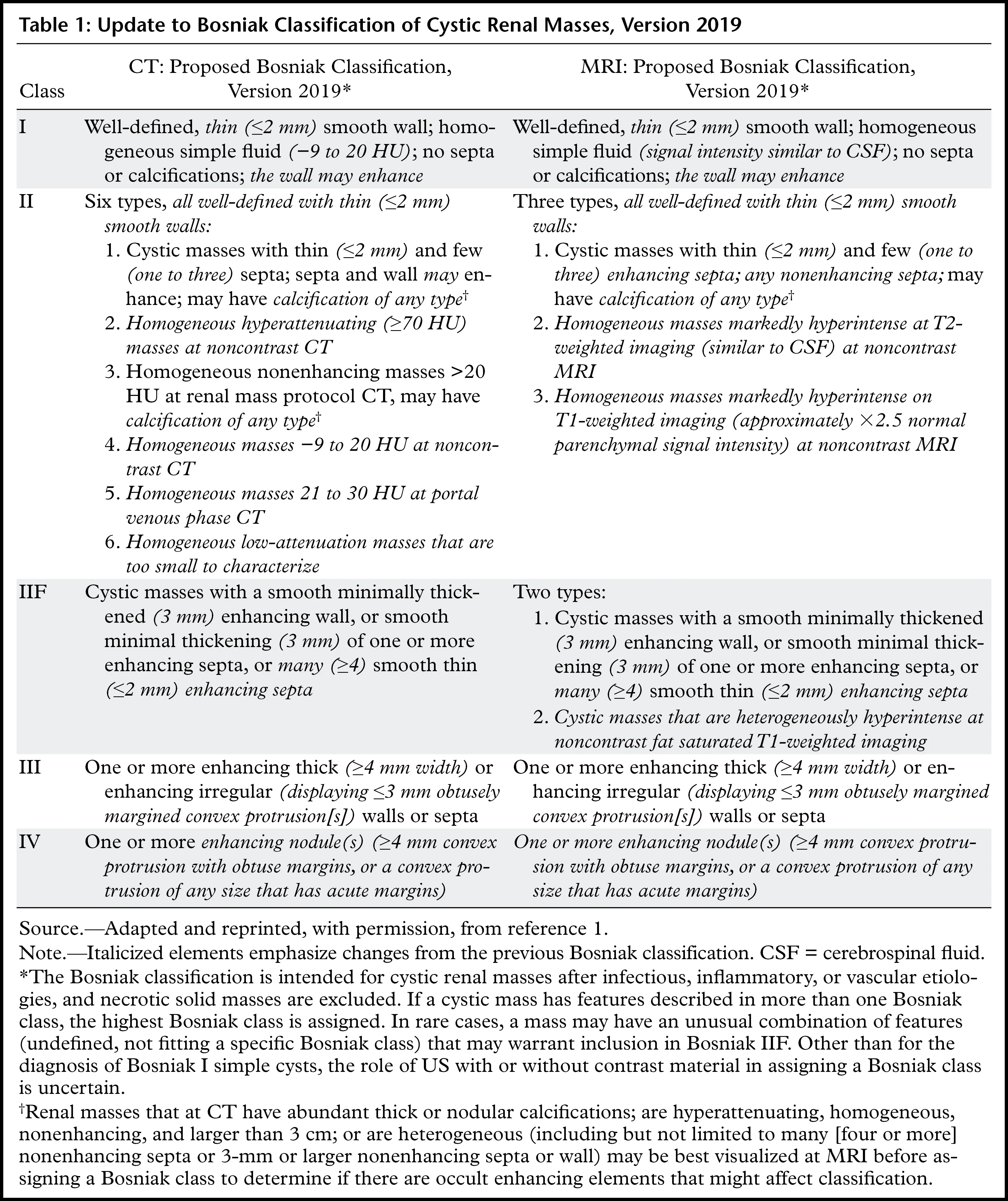 Table source: 3
Table source: 3
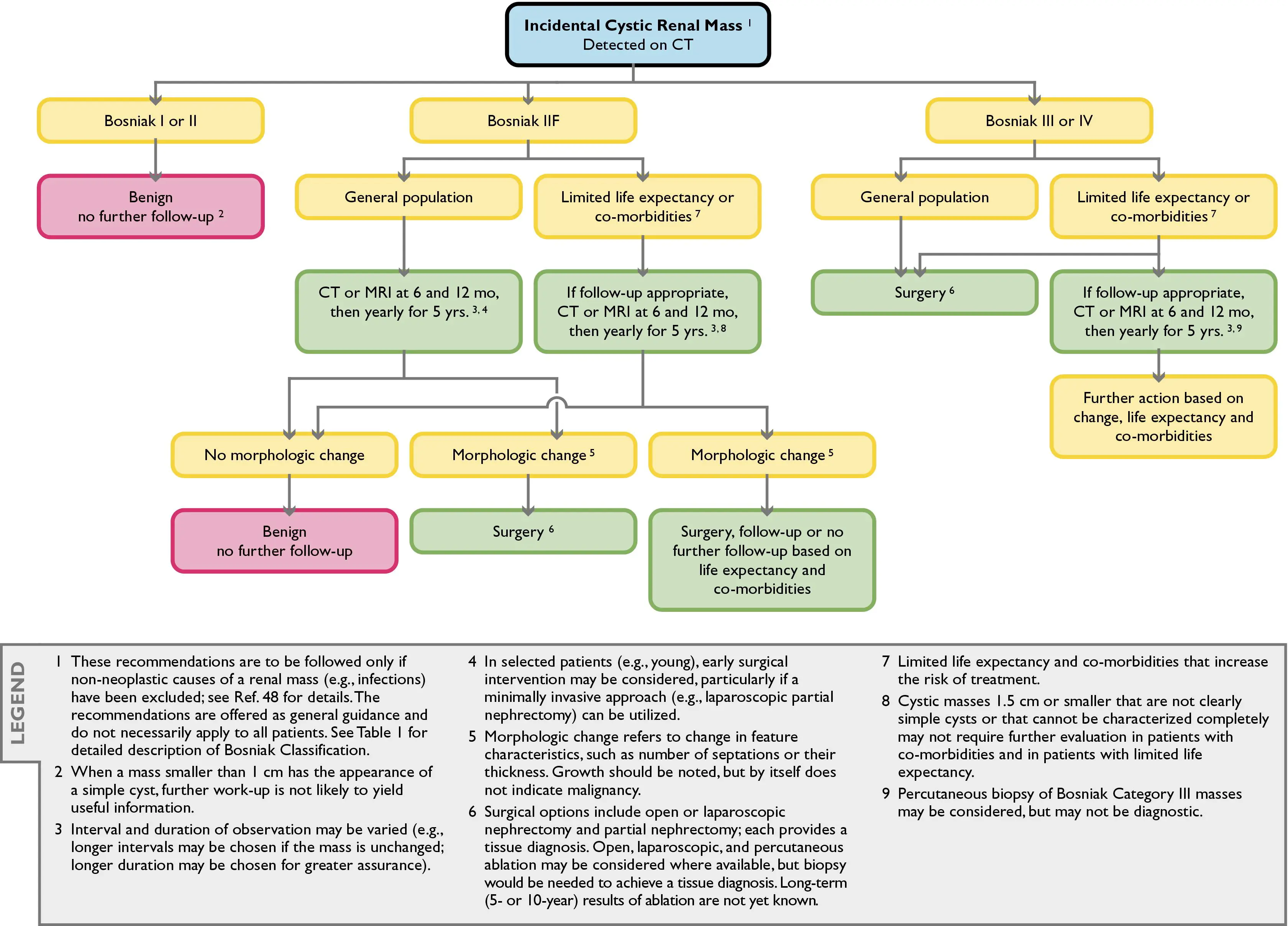 Algorithm source: 2
Algorithm source: 2
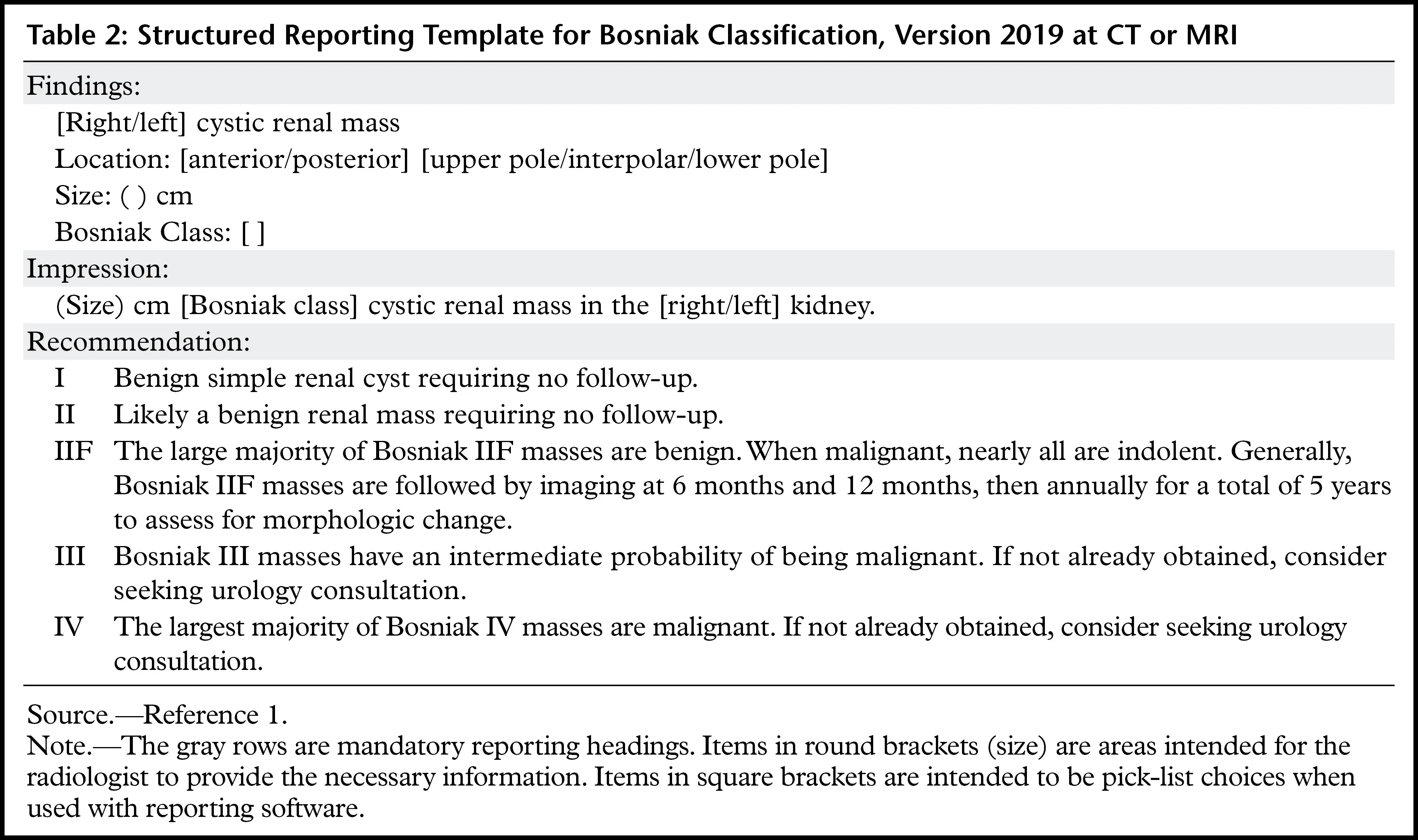 Table source: 3
Table source: 3
Renal mass
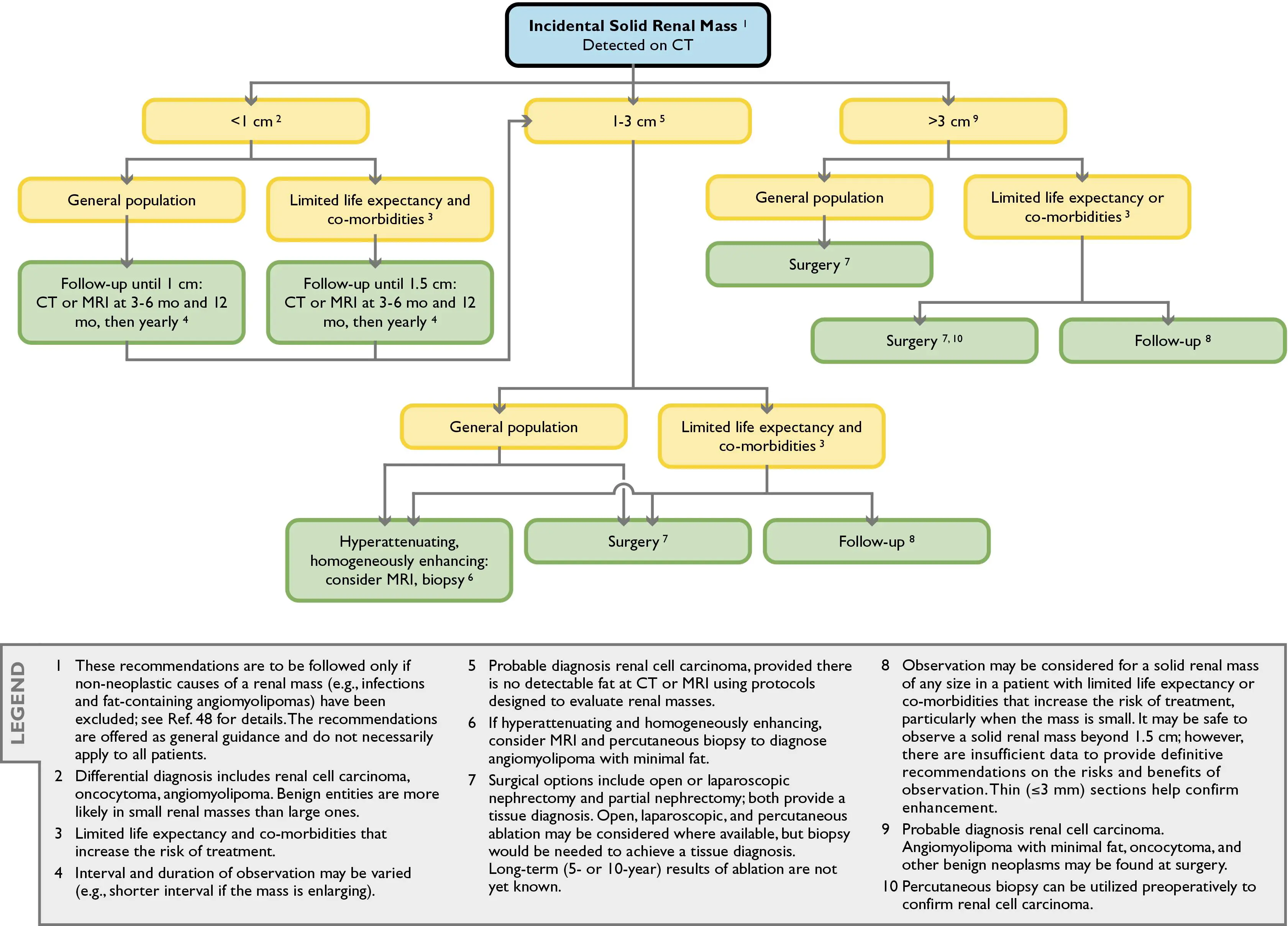 Algorithm source: 2
Algorithm source: 2
Liver
- Simple cyst - OK.
- Nodule < 1 cm - OK, likely benign.
- ⚠️ Soft tissue nodule/mass ≥ 1cm
- Recommend w/u with contrast-enhanced Abdomen CT or MRI.
- ⚠️Fatty liver/hepatic steatosis or cirrhosis
- Recommend PCP evaluation.
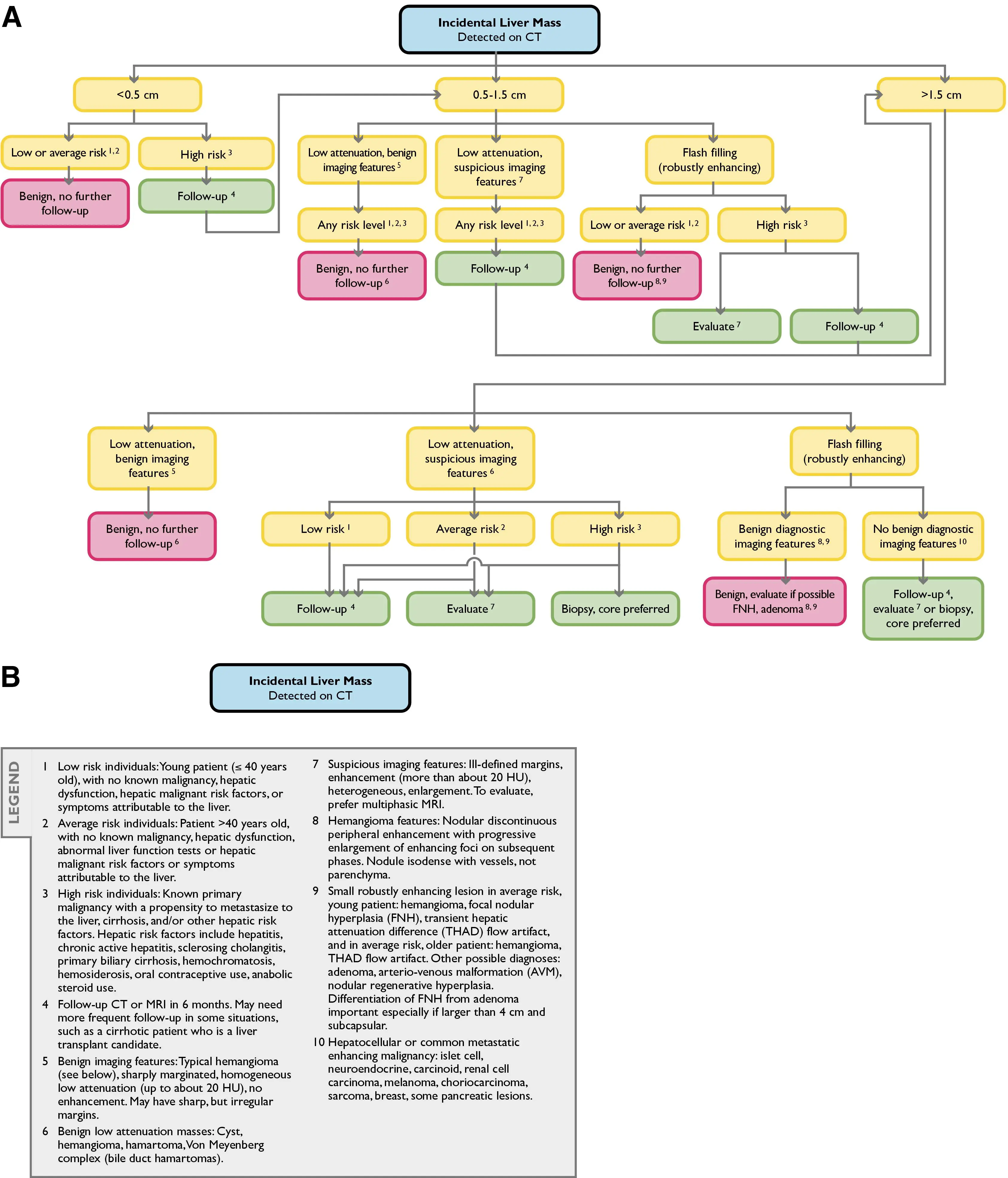 Algorithm source: 2
Algorithm source: 2
Pancreas
- Coarse calcifications - OK.
- ⚠️ Cyst/mass
- Recommend work-up with contrast-enhanced Abdomen CT or MRI.
Fluid Collections
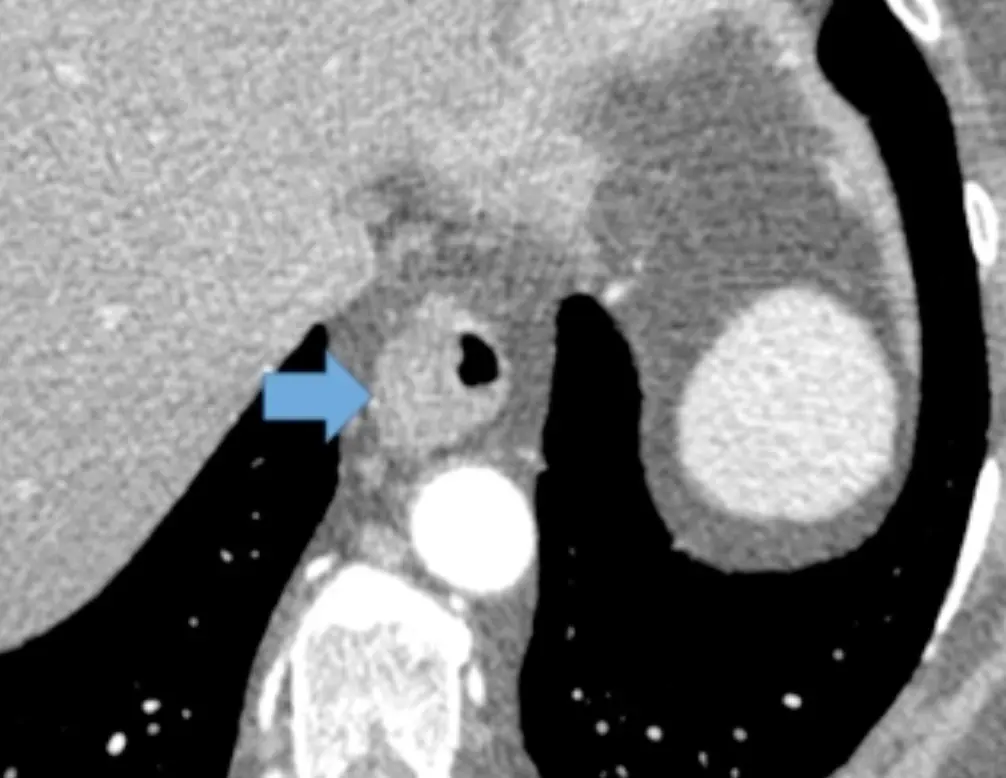
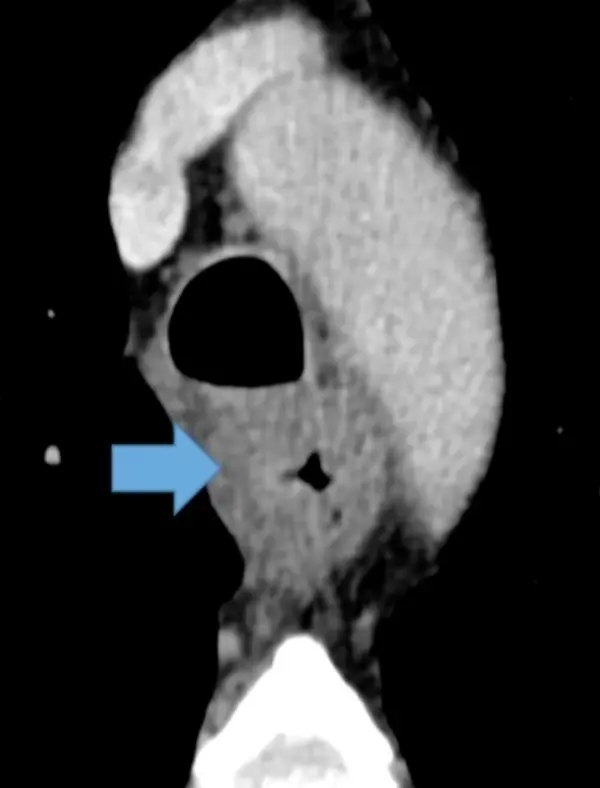
Abscesses
- Clues to calling a fluid collection an abscess include:
- rim-enhancement
- presence of air bubbles
Footnotes
-
Dyer DS, White C, Conley Thomson C, Gieske MR, Kanne JP, Chiles C, Parker MS, Menchaca M, Wu CC, Kazerooni EA. A Quick Reference Guide for Incidental Findings on Lung Cancer Screening CT Examinations. J Am Coll Radiol. 2023 Feb;20(2):162-172. doi: 10.1016/j.jacr.2022.08.009. Epub 2022 Dec 9. PMID: 36509659. ↩ ↩2
-
Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD, Francis IR, Herts BR, Israel GM, Krinsky G, Platt JF, Shuman WP, Taylor AJ. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol. 2010 Oct;7(10):754-73. doi: 10.1016/j.jacr.2010.06.013. PMID: 20889105. ↩ ↩2 ↩3 ↩4
-
Schieda N, Davenport MS, Krishna S, Edney EA, Pedrosa I, Hindman N, Baroni RH, Curci NE, Shinagare A, Silverman SG. Bosniak Classification of Cystic Renal Masses, Version 2019: A Pictorial Guide to Clinical Use. Radiographics. 2021 May-Jun;41(3):814-828. doi: 10.1148/rg.2021200160. Epub 2021 Apr 16. Erratum in: Radiographics. 2022 Jan-Feb;42(1):E33. doi: 10.1148/rg.219016. PMID: 33861647. ↩ ↩2