# Pericardial effusion
- (Acute/subacute/chronic) (mild/moderate/large) (circumferential/loculated) (transudative/exudative)
- Work-up: CBC, ESR, CRP, CK, troponin, 12-lead ECG, CXR
- Imaging
- Echo
- CT/MR (if loculated effusion, pericardial thickening and masses, or other chest abnormalities)
- Empiric therapy for pericarditis if inflammatory signs present- The normal pericardial sac contains 10—50 ml of pericardial fluid as a plasma ultrafiltrate that acts as a lubricant between the pericardial layers.
- Etiology can be broken down into one of 2 issues:
- Increased production or accumulation
- Decreased reabsorption
flowchart TD A[Pericardial Effusion] --> B(↑ production or accumulation) A --> C(↓ reabsorption)
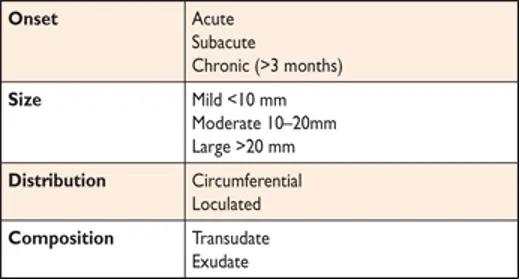
- Classification
-
Onset
- acute or subacute vs. chronic when lasting >3 months
-
Distribution
- circumferential or loculated
-
Hemodynamic impact
- none, cardiac tamponade, effusive-constrictive
-
Composition
- exudate, transudate, blood, rarely air, or gas from bacterial infections
-
Size
- Mild: < 1.0 cm
- Moderate: 1.0-2.0 cm
- Large: > 2.0 cm
- 📝 Assess end-diastolic distance of the echo-free space between the epicardium and parietal pericardium: small (<1.0 cm), moderate (1.0-2.0 cm), large (>2.0 cm)
-
-
Patient History
- Classic symptoms include DOE progressing to orthopnoea, chest pain and/or fullness.
- Additional occasional symptoms due to local compression may include nausea (diaphragm), dysphagia (esophagus), hoarseness (recurrent laryngeal nerve) and hiccups (phrenic nerve).
- Non-specific symptoms include cough, weakness, fatigue, anorexia and palpitations, and reflect the compressive effect of the pericardial fluid on contiguous anatomic structures or reduced blood pressure and secondary sinus tachycardia.
Management
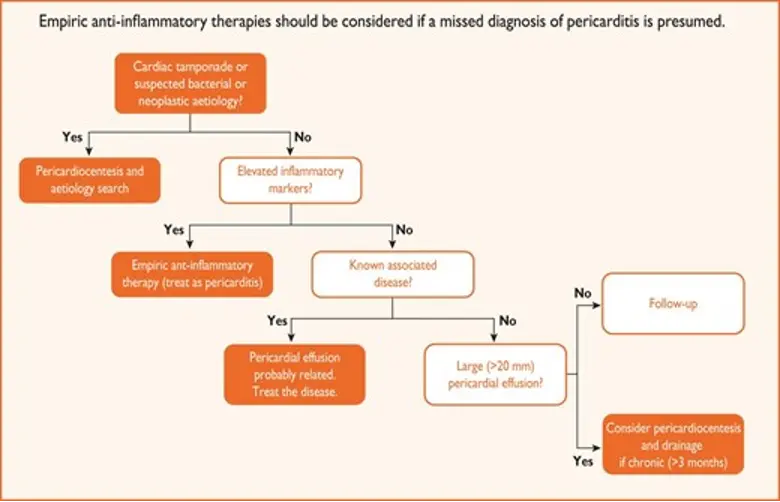
- If inflammatory signs are present, the clinical management should be that of pericarditis.
- Cardiac tamponade without inflammatory signs is associated with a higher risk of a neoplastic etiology (likelihood ratio 2.9), whereas a severe effusion without cardiac tamponade and inflammatory signs is usually associated with a chronic idiopathic etiology (likelihood ratio 20).
- If moderate/large effusion, consider bacterial or neoplastic conditions
- What do I do if chronic effusion without a definite etiology?
- No data on role of NSAIDs, colchicine, steroids
- If inflammatory markers up, consider trial of NSAIDs and/or colchicine and/or low-dose steroids
- In the absence of inflammation, NSAIDs, colchicine and corticosteroids are generally not effective.
Pericardiocentesis
-
Indications
- Cardiac Tamponade present
- Symptomatic moderate/large effusion unresponsive to medical therapy
- Suspicion of unknown bacterial or neoplastic etiology
-
Recurrences are common, and pericardiectomy or less invasive options (i.e. pericardial window) should be considered whenever fluid reaccumulates, becomes loculated or biopsy material is required.
-
Follow-up
-
Symptoms
-
Echocardiographic size of the effusion
-
Additional features such as inflammatory markers (i.e. CRP)