- Diastolic function is a catch-all term referring to several different physiological processes that allow the left ventricle (LV) to fill with sufficient blood for the body’s current needs at a low enough pressure to prevent pulmonary congestion.1
- In broad terms, one can focus on 2 main aspects: 2
- myocardial relaxation
- chamber stiffness
- Normal diastolic function allows adequate filling of the heart without an excessive increase in diastolic filling pressure both in the resting state and with stress or exertion.3
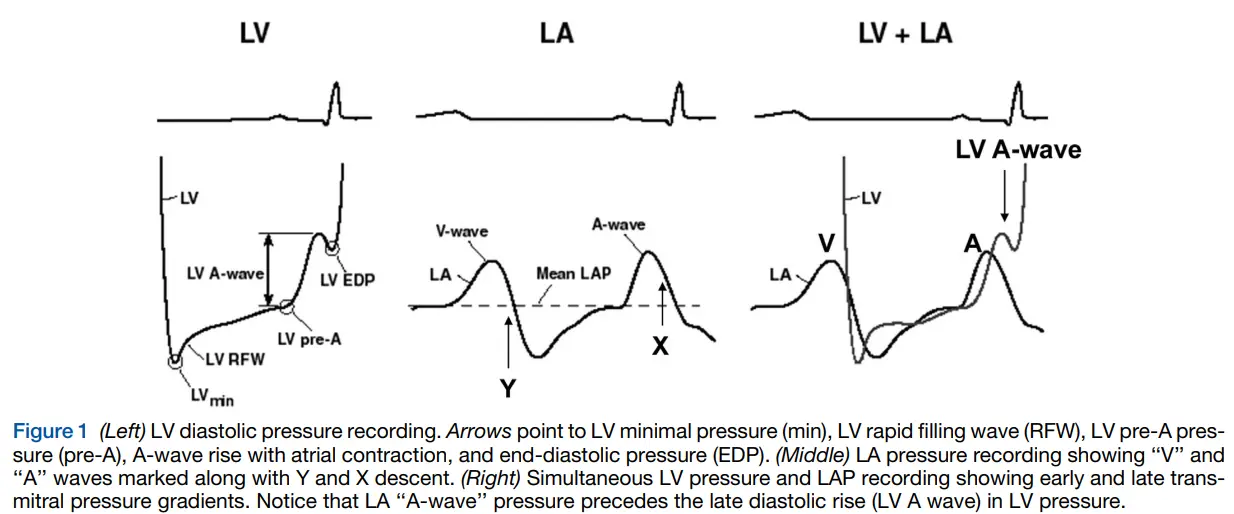
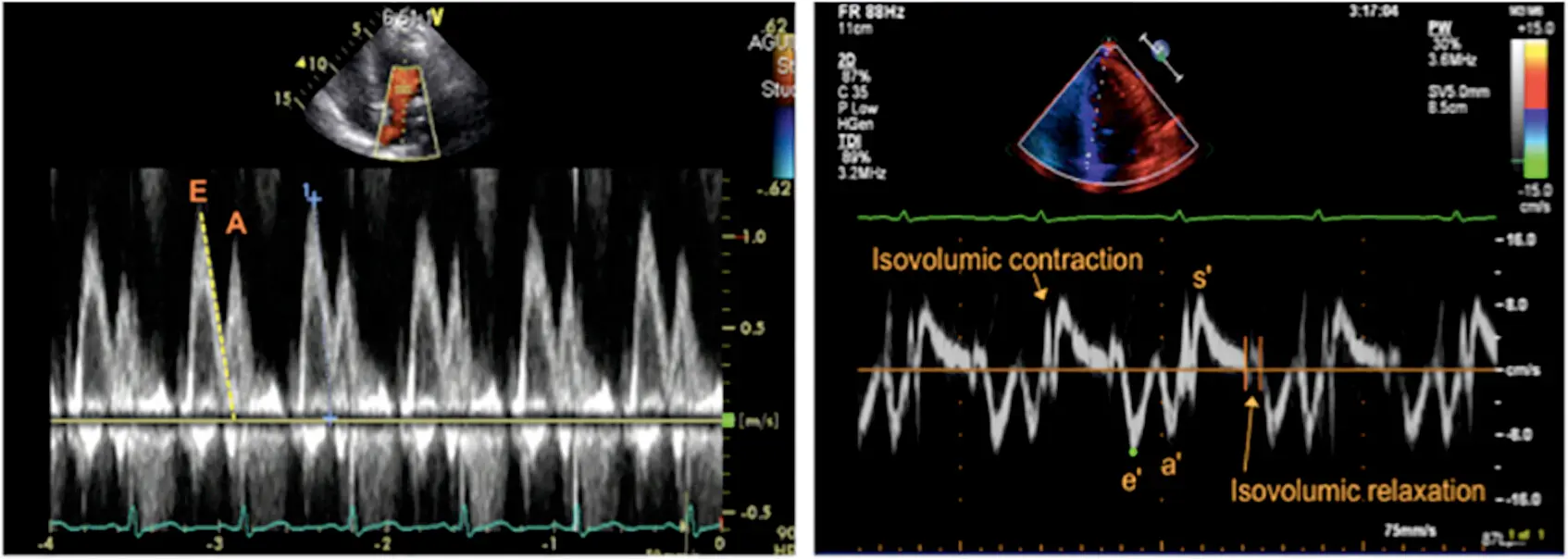
- Basically, at the end of systole, left ventricular (LV) relaxation begins as an initial diastolic process, and LV pressure falls rapidly as the LV expands. This relaxation phase is accompanied by active movement of the mitral annulus away from the apex. The velocity of LV dilatation and mitral annular movement during early diastole correlates well with how fast the LV fills and relaxes, respectively.3
- 3 likens myocardial relaxation in a healthy ♥️ as helping to “suck” or “pull” the blood actively into the LV.
- By contrast, with diastolic dysfunction, you have a more laborious “push” of blood from the LA into the LV.
- ↑ pressure in LA is needed to push blood into the LV
Diagnosis
- Echocardiography is used to assess LV diastolic function, and estimate LV filling pressures.
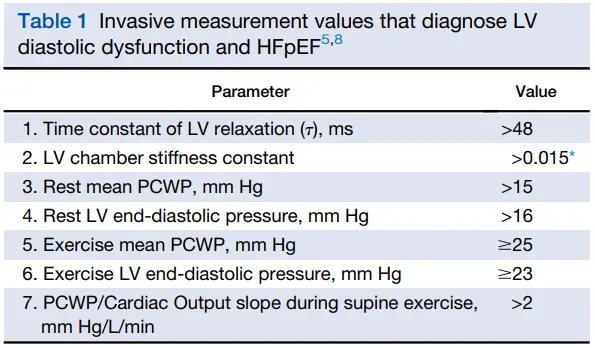
Invasive Hemodynamics
Echocardiography
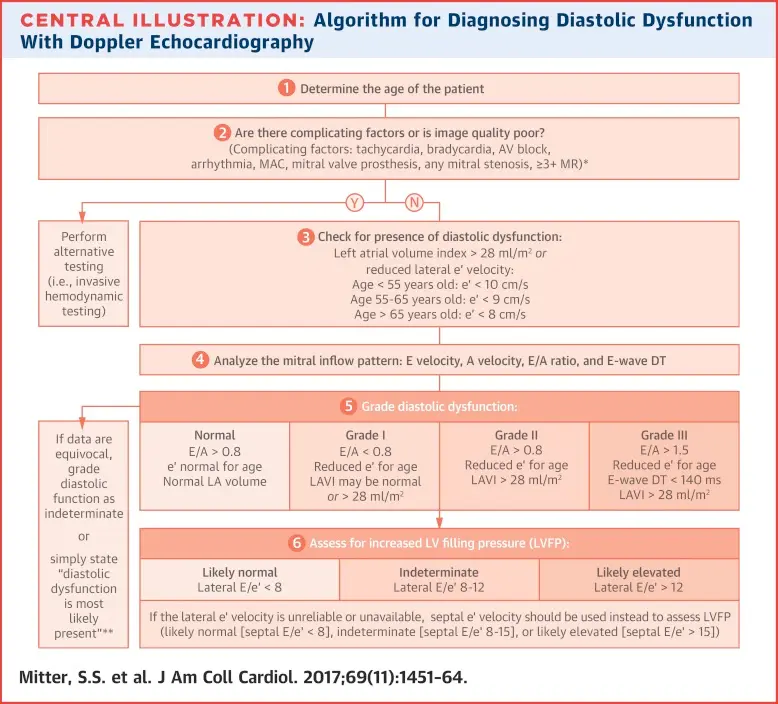
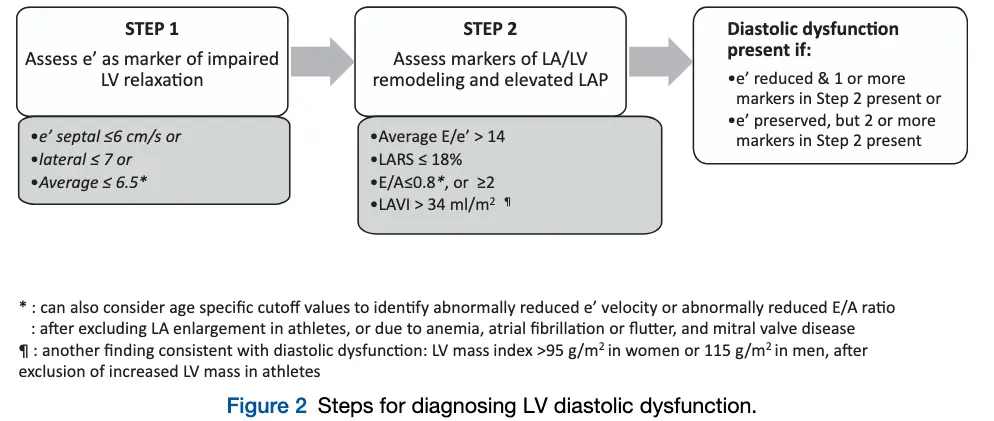
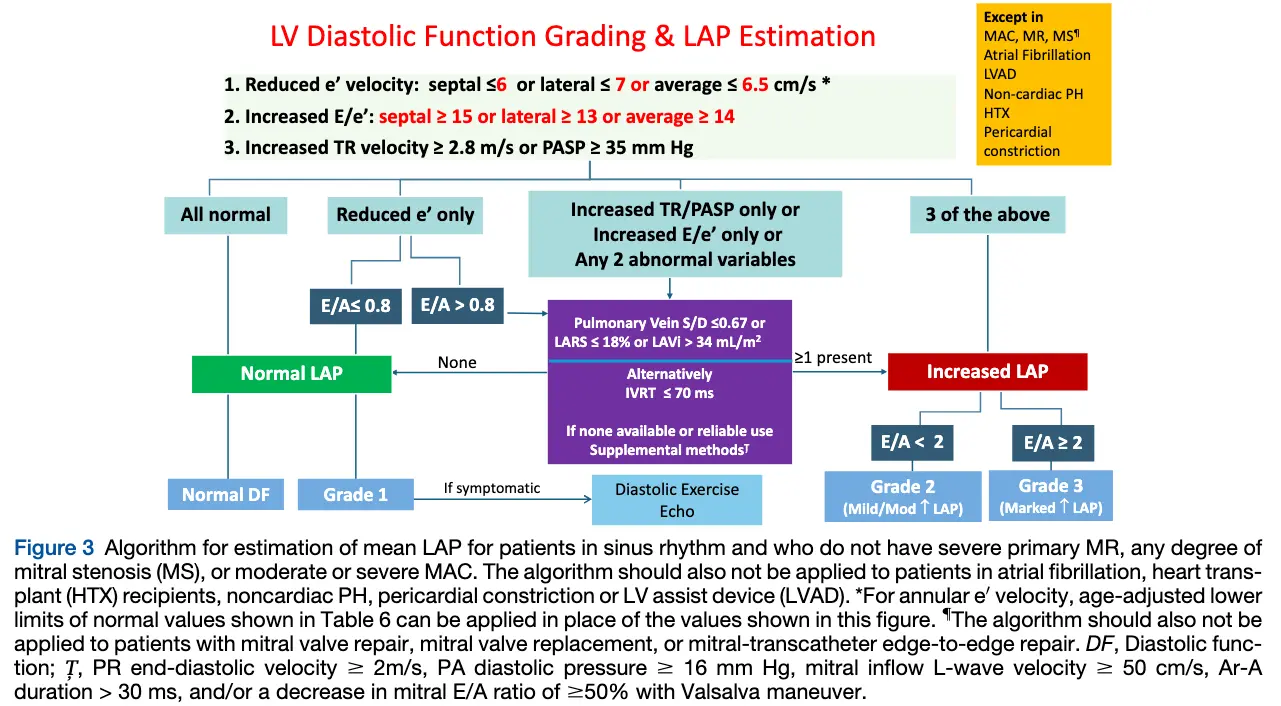
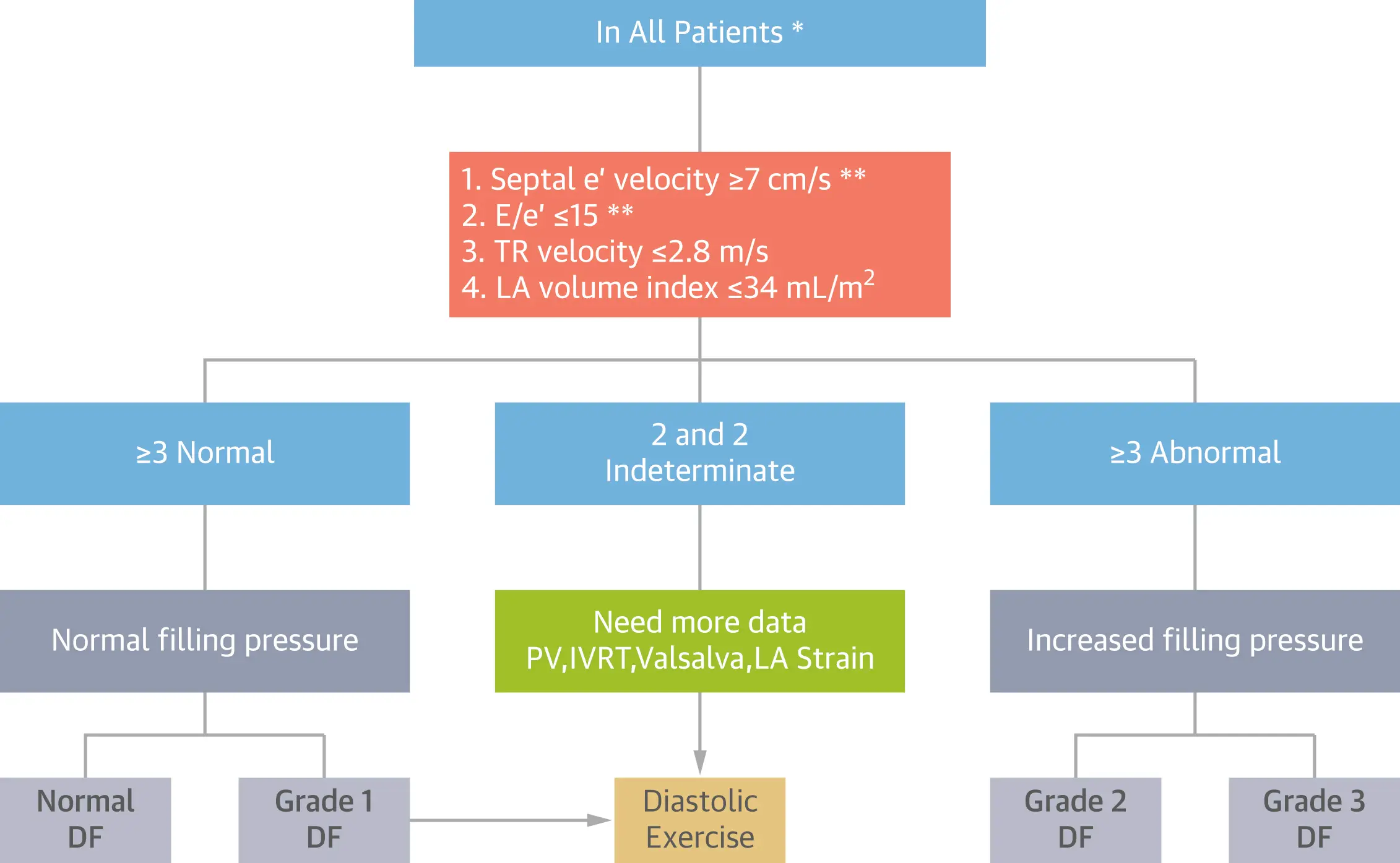
2025 ASE Guideline algorithm 4
2016 ASE Guidelines algorithm 5
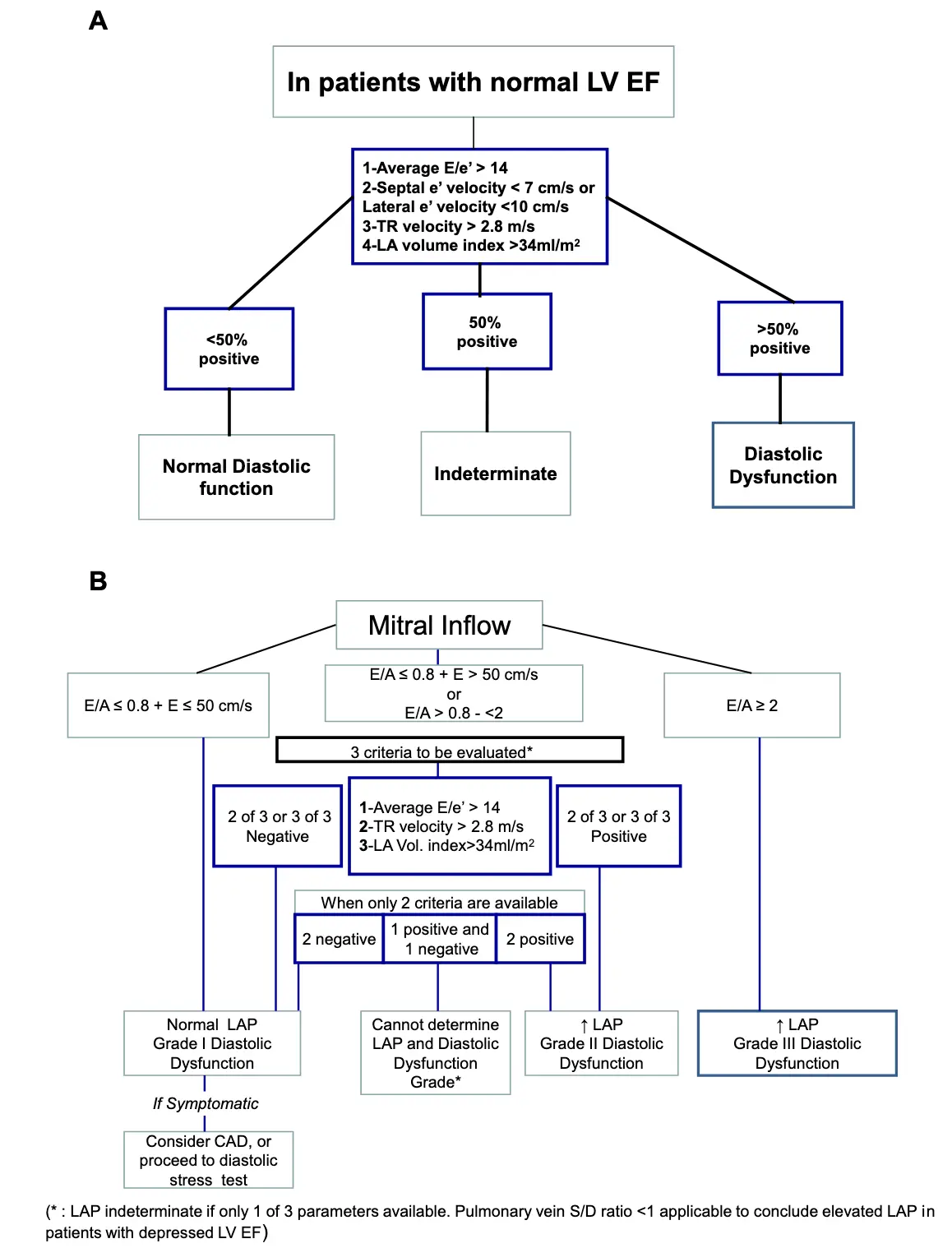
Not everyone with systolic dysfunction has diastolic dysfunction
Dr. Oh said that it is a myth that diastolic dysfunction is always abnormal in patients with systolic dysfunction (as implied by the above algorithm). Rather, he reminds us that “the e’ velocity has to be reduced for there to be diastolic dysfunction”
Revised algorithm from 6
 The 6 algorithm does not apply to patients with at least moderate mitral annulus calcification, left bundle branch block, pacemaker rhythm, or severe primary pulmonary hypertension.
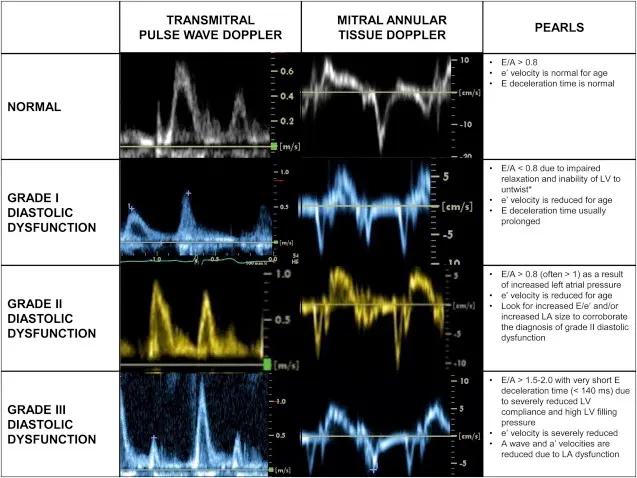
Normal or grade 1 diastolic function is assigned to the subject with normal filling pressure with E/A > 0.8 and ≤ 0.8, respectively, and grade 2 or 3 to the group with increased filling pressure with E/A < 2 and ≥ 2.
The 6 revised algorithm can be also used for patients with atrial fibrillation to assess filling pressure, but not grading, with the different E/e’ cutoff value of 11.
The 6 algorithm does not apply to patients with at least moderate mitral annulus calcification, left bundle branch block, pacemaker rhythm, or severe primary pulmonary hypertension.
Normal or grade 1 diastolic function is assigned to the subject with normal filling pressure with E/A > 0.8 and ≤ 0.8, respectively, and grade 2 or 3 to the group with increased filling pressure with E/A < 2 and ≥ 2.
The 6 revised algorithm can be also used for patients with atrial fibrillation to assess filling pressure, but not grading, with the different E/e’ cutoff value of 11.
-
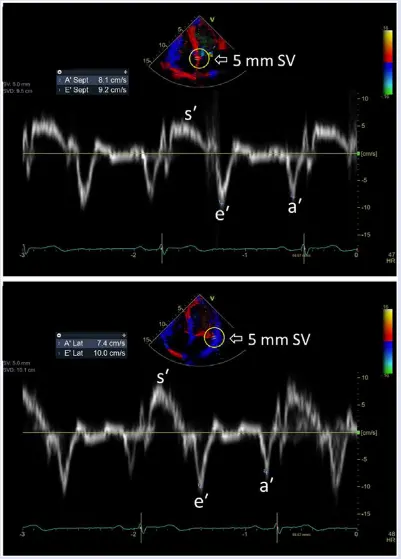
Mitral inflow velocity: Peak E-wave velocity (cm/s) is the peak early diastolic modal velocity after ECG T wave
-
Mitral inflow velocity: Peak A-wave velocity (cm/s): peak late diastolic modal velocity after ECG P wave
-
Mitral annular velocity: e’ velocity (cm/s): peak early diastolic modal velocity after ECG T-wave
-
Mitral annular velocity: a’ velocity (cm/s): peak late diastolic modal velocity after ECG P-wave
-
A and e′ should not be used in isolation in assessing diastolic function and LVEDP, but rather used in conjunction with clinical characteristics, such as age and medical history, and other echocardiographic parameters from the study in its entirety to accurately classify diastolic function.
-
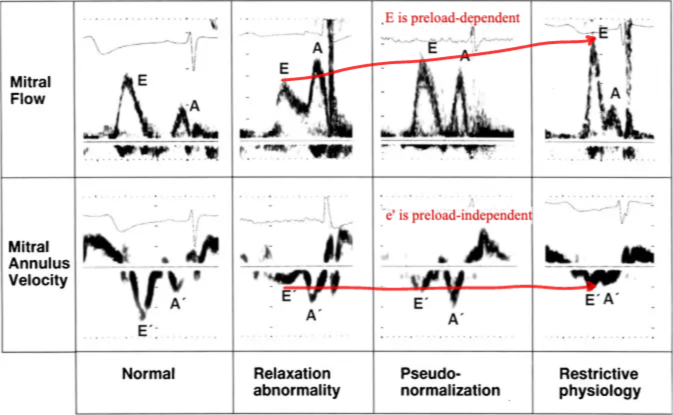
E velocity on mitral inflow is preload-dependent, whereas the mitral annulus e’ velocity as a marker for LV relaxation is preload-independent.
- ==E mitral inflow velocity increases with severity of diastolic dysfunction==
- This characteristics also allows you to distinguish “pseudonormal” vs normal.
Normal Reference Ranges
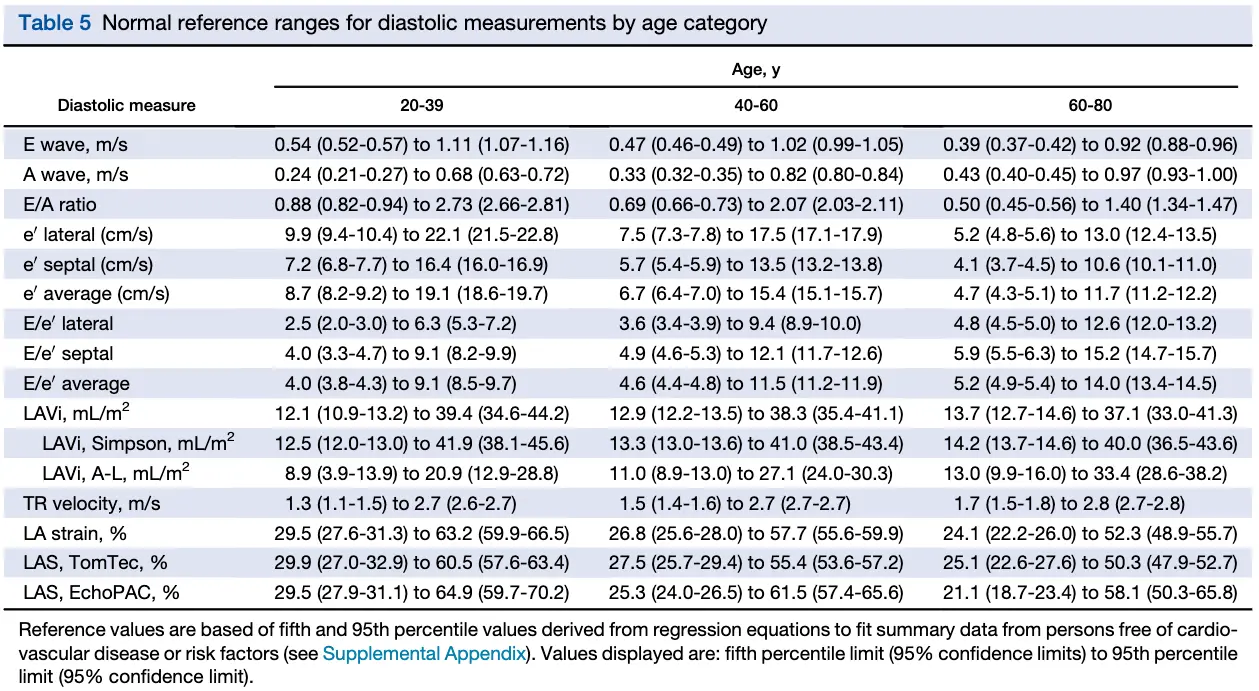
Mitral annular e’ velocity
See Tissue Doppler
Normal e' velocity values
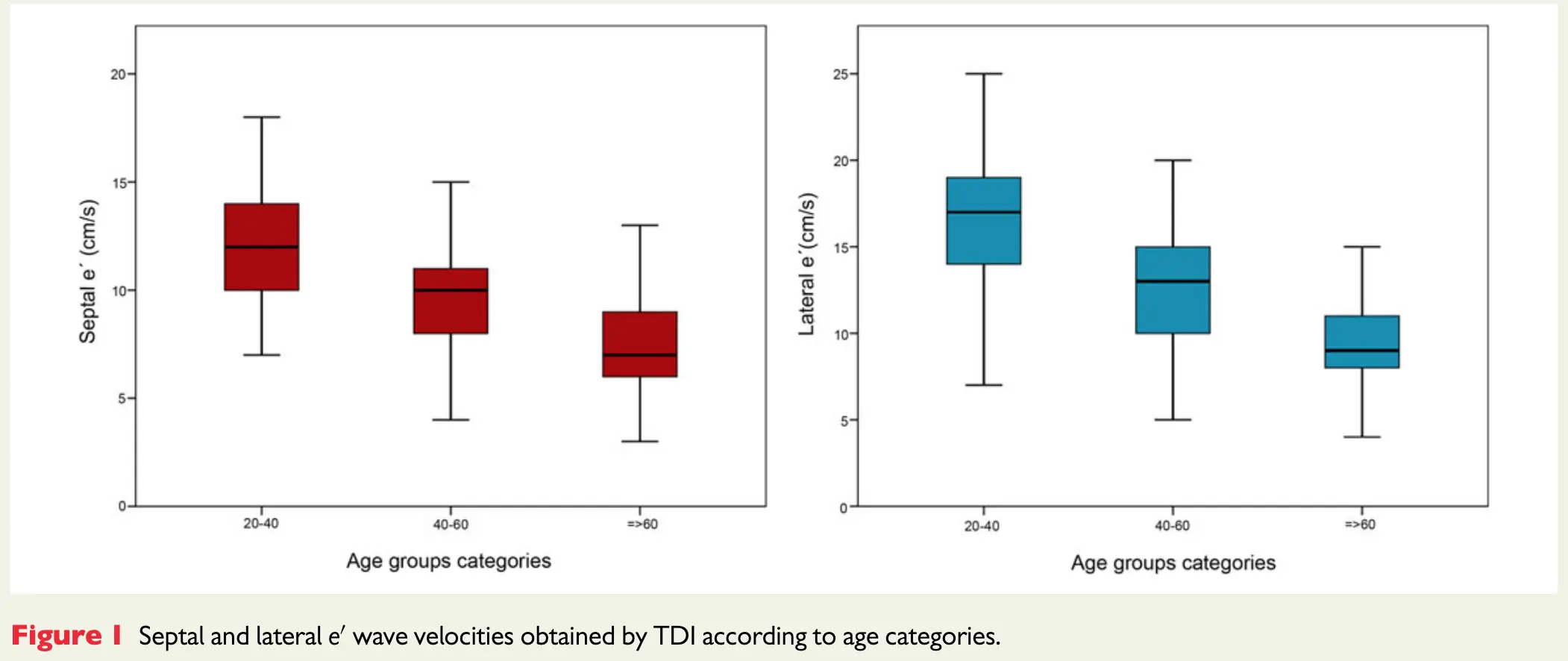
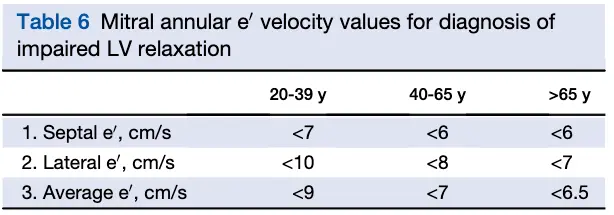
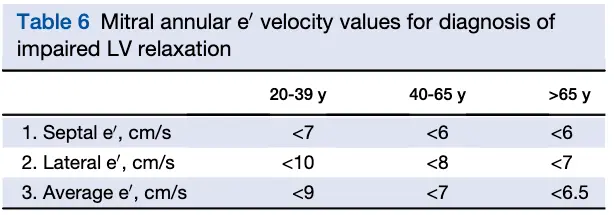
As a general rule of thumb, normal LV relaxation is suggested by medial e’ ≥ 9 cm/s and lateral e’ ≥ 12 cm/s. However, values can vary by age 👇
- According to Dr. Oh, e’ velocity is money 💵 because normal LV relaxation (e’) means you must have normal diastolic function. This is reflected in the Step 1→Step 2 algorithm (Figure 2) proposed in the 2025 guideline update.4
- In other words, you can stop looking for other markers of diastolic dysfunction if you have normal e’ velocities.
- “Once you see that e’ is normal, you don’t need to look at anything else because you cannot have diastolic dysfunction with normal e’ velocities” - Dr. Oh
- “Normal e′ velocity is unusual in patients with diastolic dysfunction related to a myocardial abnormality or disease, which is a main reason that the joint Diastology Working Group recommends that an evaluation of diastolic function begins with e′ in patients with normal LV ejection fraction.” 3
- In healthy hearts, a significant amount of LV ejection and LA filling results from descent of the mitral annulus toward the apex. This longitudinal motion normally precedes filling.1
- A bunch of comorbidities (e.g., HTN, obesity, diabetes) can lead to impaired myocardial relaxation and restoration forces, and ↑ lengthening load (LA pressure) → reduced and delayed longitudinal motion and e′ velocity
- E/e′ showed poor correlation with direct LA pressure measurements in patients with HCM
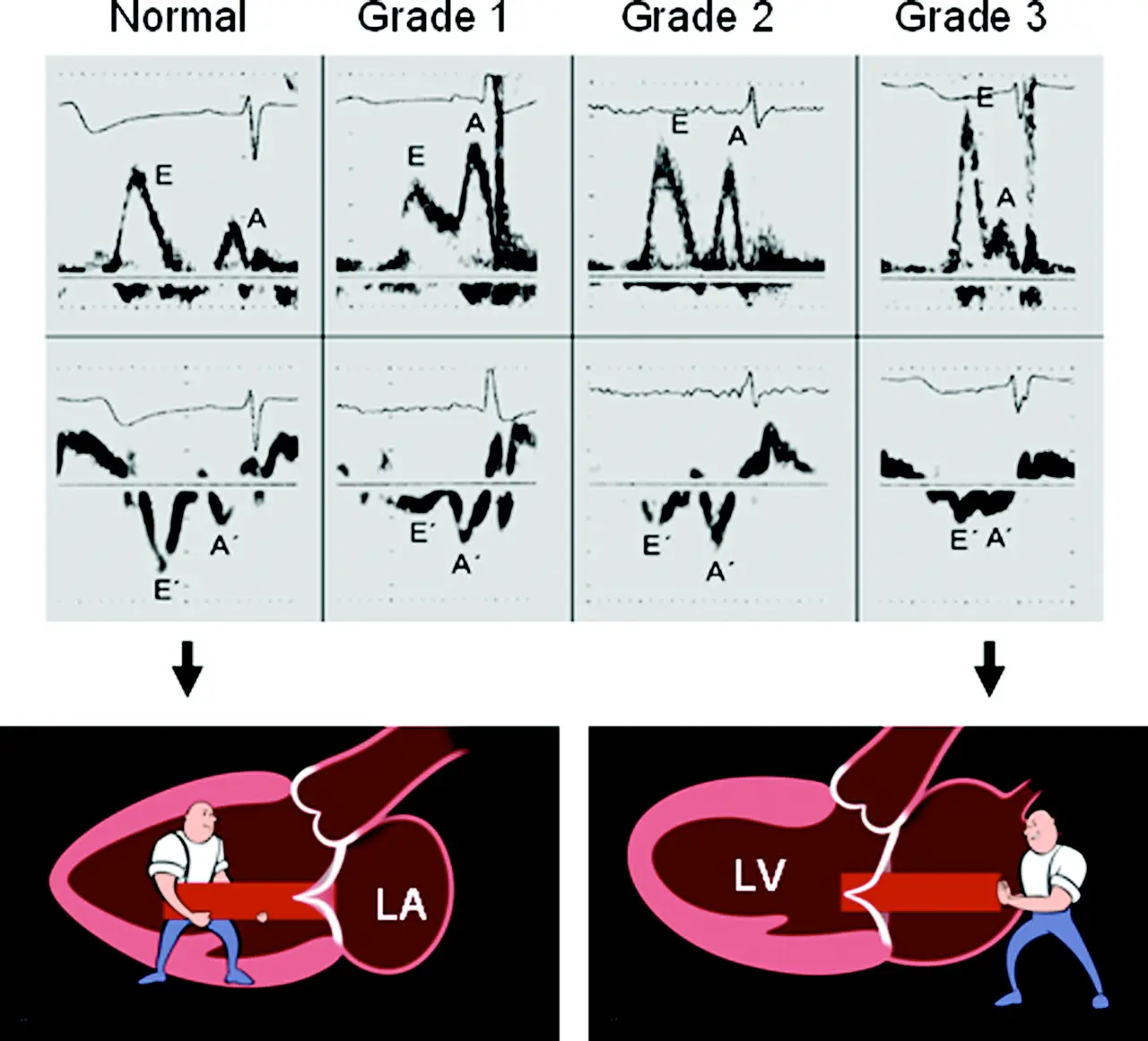 Figure source: 3
Figure source: 3
- The normal range of e’ velocities can vary by age as shown by 7 and reflected in the 2025 guideline update 4
E/A ratio
- The E/A ratio in healthy, euvolemic, recumbent young adults is typically >1.
- Active, late diastolic blood flow into the LV is driven by atrial contraction (A).
- The E/A ratio in healthy, euvolemic, recumbent young adults is typically >1. When τ is prolonged (often seen with aging, HTN, HCM, ischemia, AMI), is lower, and the E-wave is smaller, leading to the grade I diastolic dysfunction filling pattern where E/A <1.
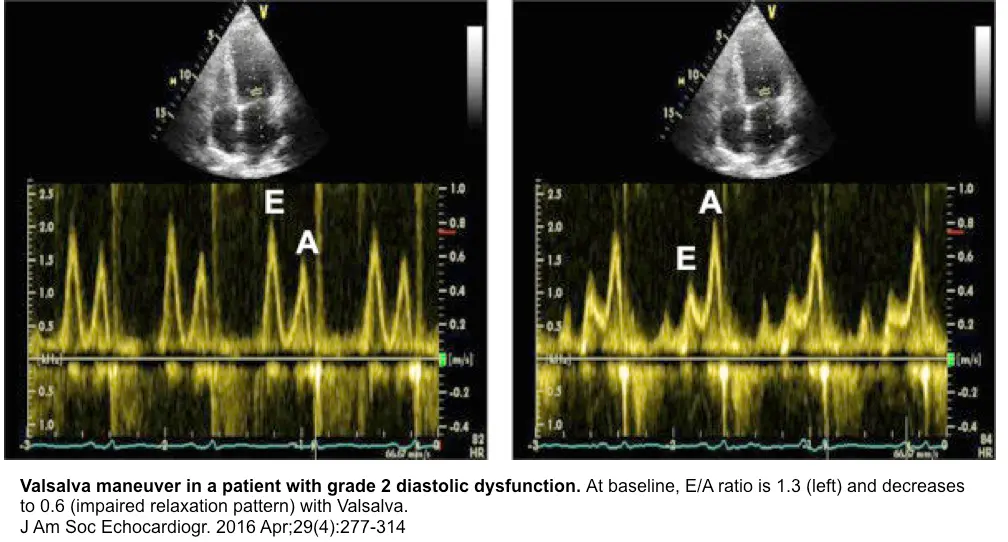
- To compensate for impaired relaxation, LA pressure may rise, increasing and E-wave height, leading to the grade II (“pseudonormal”) or grade III (“restrictive”) diastolic dysfunction filling pattern, with consequent risk for pulmonary congestion
- Valsalva maneuver to tease out normal vs “pseudonormal” (grade II) diastolic dysfunction
- tbh, this is an old school 👵 approach, so you may rarely have a sonographer collect this for you
- normal: Valsalva → ↓ preload → ↓ amplitude of both the E- and A-wave
- grade II diastolic dysfunction: Valsalva → ↓ preload → filling will occur on the flatter portion of the LV diastolic PV relationship; ∴, E-wave amplitude ↓ > A-wave amplitude ↓ less (or may actually ↑) → E/A reversal (i.e., E/A ratio <1)
TR Velocity
- TR velocity > 2.8 m/s is very specific
Left atrial size
TODO
Isovolumic Relaxation Time (IVRT)
- IVRT is a good screening parameter for LA pressure, regardless of underlying LV ejection fraction.3
- IVRT is shortened when LA pressure increases.
- IVRT measures the time between aortic valve closure until mitral valve opening/inflow.
- If IVRT is prolonged (>100 ms), LA pressure is not elevated because the delay in mitral valve opening is related to lower pressure crossover between LV and LA in the setting of delayed relaxation.3
- In other words, a longer duration of IVRT (closure of AV to mitral inflow) on mitral inflow suggests normal filling pressures
- If LA pressure is elevated even with abnormal myocardial relaxation, the mitral valve opens at a high pressure, and IVRT gets shortened. ∴, it is safe to conclude that LA pressure is elevated if the IVRT is short (<60 ms) in the presence of cardiac disease. However, it is difficult to estimate LA pressure when IVRT is relatively normal.3
- In patients with impaired LV relaxation, IVRT <70 ms is usually associated with increased LA pressure.2
Deceleration time (DT) of E velocity
- Influenced by the rate of decline in LA-LV pressure gradient after mitral valve opening, and therefore LV stiffness. When LV relaxation is slow, LV relaxation also affects DT.2
Pulmonary vein (S/D ratio)
- The corresponding value for pulmonary vein systolic velocity–to–diastolic velocity (S/D) ratio of ≤0.67 is equal to ≤40% systolic filling fraction and is therefore recommended. The ratio is most reliable in patients with LV systolic dysfunction and should not be considered in normal subjects with normal echocardiographic results, when the ratio can be ≤ 0.67. 4
L wave
- Although the L wave can occur in healthy, well-conditioned individuals with bradycardia, its peak velocity usually is <20 cm/s in that setting.3
- As diastolic function worsens, LA pressure is elevated and myocardial relaxation is impaired at rest, clinically manifesting as heart failure. In this stage, most of the diastolic filling that occurs during early diastole and LA contraction may not be able to contribute substantially to LV filling because of the increased LV diastolic pressure. In these patients, LA contraction pushes blood back into the pulmonary veins, especially if pulmonary venous diastolic forward flow is already completed at the time of atrial contraction.3
- Related: HFpEF
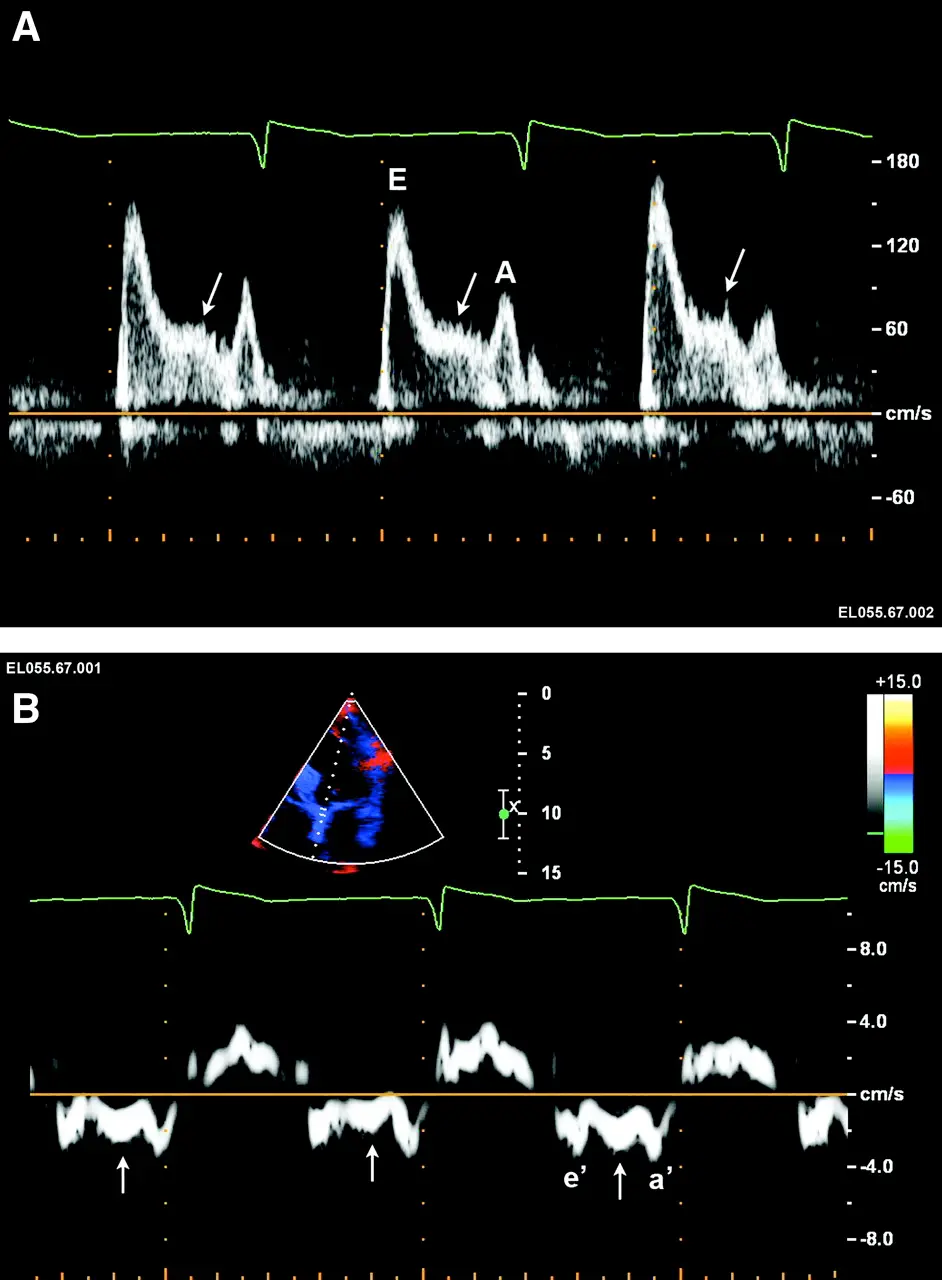 Figure source: 3. The arrow (→) corresponds to the L wave, which is due to elevated filling pressure and delayed myocardial relaxation
Figure source: 3. The arrow (→) corresponds to the L wave, which is due to elevated filling pressure and delayed myocardial relaxation
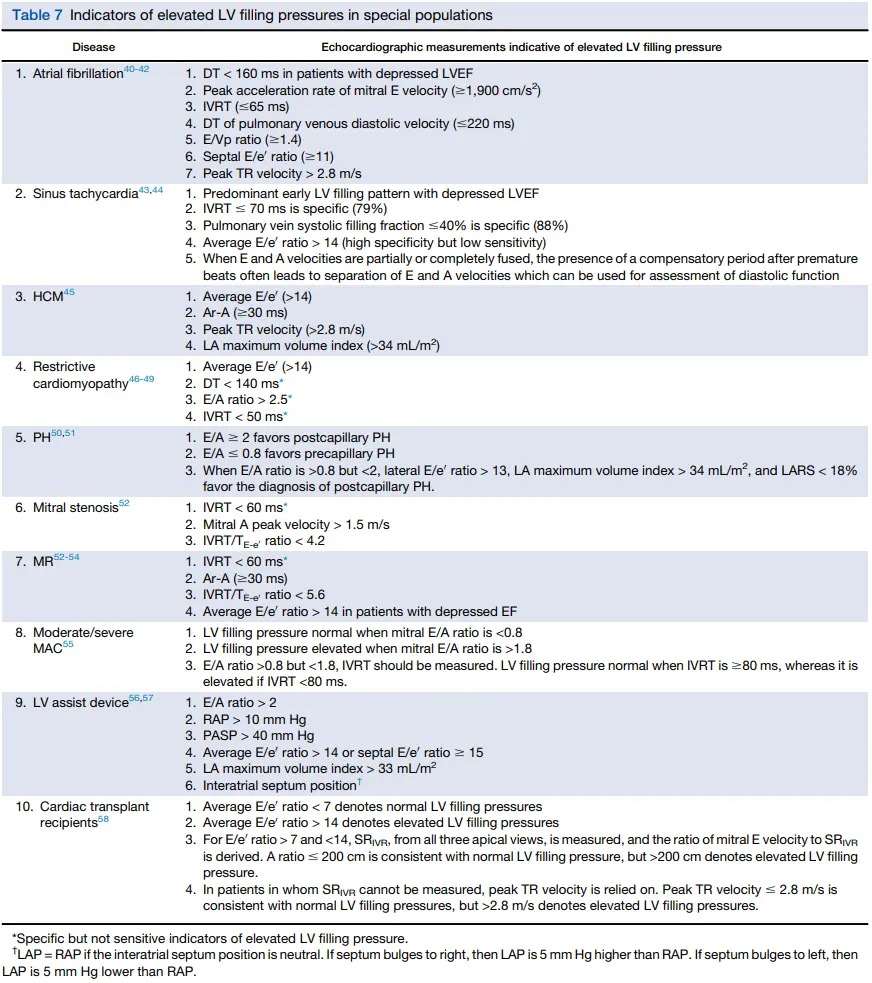
Special Populations
AFib
- In AFib, beat-to-beat variability and the absence of A waves make the assessment of diastolic dysfunction difficult.
- Doppler parameters, such as e′ <8 and E/e′ >11 that are associated with tau >50 ms and LV filling pressures of >15 mm Hg, respectively, are needed to help assess diastolic function and increased LA pressure.1
- 📝 The presence of a second filling wave after the E-wave (L-wave) in patients with AFib is correlated with advanced diastolic dysfunction.1
- ⚠️ Even in the absence of atrial fibrillation, the L-wave and the L′ (its tissue Doppler correlate) are markers of worse diastolic function and filling pressure in a variety of settings, and predict future heart failure events
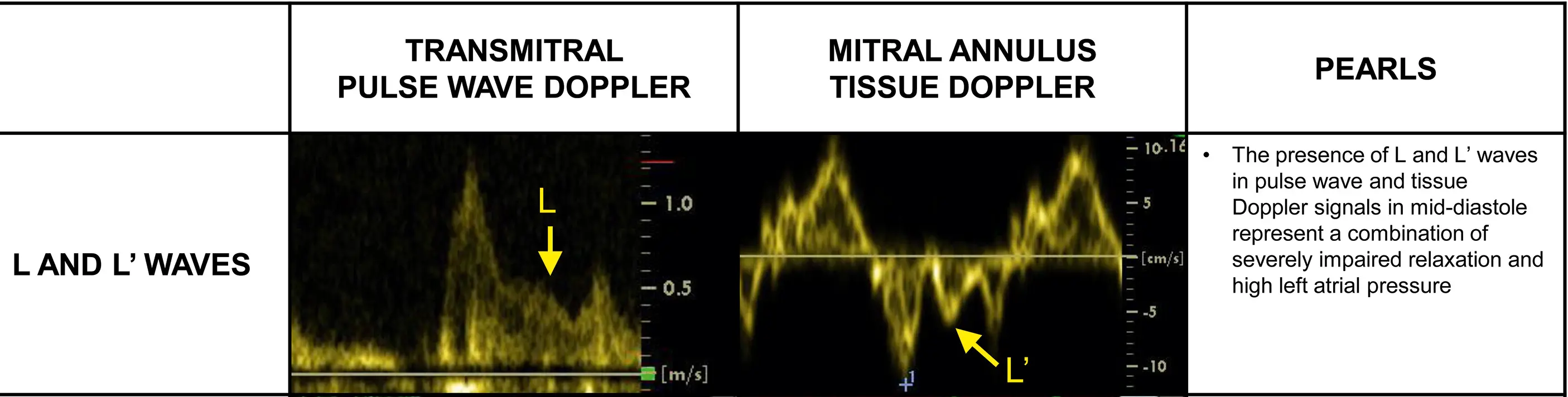
- Other parameters associated with higher LV filling pressures in individuals with atrial fibrillation include shortened diastolic pulmonary vein flow DT (<220 ms), regardless of LV function, and an E-wave DT of <150 ms in the presence of LV systolic dysfunction
Mitral Regurgitation
- Typically, with LV diastolic dysfunction, the increased LV diastolic pressures contribute to the increase in LAP
- Primary MR: - Pathologic sequence: Primary MR → LA and LV enlargement → increase in the compliance of both chambers, which attenuates the increase in LAP. Later, with increased LA stiffness, mean LAP and PA pressures increase, which is related to MR, not LV myocardial disease.
- Secondary MR: - Pathologic sequence: in primary myocardial disease (e.g. dilated cardiomyopathy) → increased LV diastolic pressures initially and later you get functional MR. Therefore, in patients with secondary MR, echocardiographic correlates of increased filling pressures reflect the combination of both myocardial and valvular disorders
- Moderate and severe MR usually lead to an increase in mitral E velocity and a decrease in pulmonary vein systolic velocity, and the S-to-D ratio
Exercise Echo
- Up to 50% of patients with HFpEF have normal LV filling pressure at rest that increases rapidly with exercise or even leg raising
- Effect of e’ velocity with exercise: In normal subjects, mitral e’ increases about 3 to 5 cm/s on average with exercise, but in subjects with diastolic dysfunction, e’ velocity does not increase as much as in a normal subject, or not at all
- Effect of mitral E velocity and E/e’ with exercise: In patients with diastolic dysfunction, mitral inflow E velocity increases with exercise and e’ does not change as much, such that E/e’ ratio increases
- Who should you consider for diastolic exercise testing?
- patients with grade 1 diastolic dysfunction, which indicates the presence of delayed myocardial relaxation and normal mean LAP at rest.
- symptomatic patients with indeterminate diastolic function or filling pressure at rest
- LARS as it has been reported to identify patients who are more likely to develop increased filling pressure with exercise
- Diastolic stress testing can be performed using either supine bicycle or treadmill exercise echocardiography.
- Interpretation of diastolic exercise echo
- Increased LV filling pressures: average E/e’ ratio ≥ 14 or septal E/e’ ratio ≥ 15 and peak TR velocity > 3.2 m/s
- 📝: HFpEF diagnosis is NOT supported by an E/e’ ratio <14, even with an increase in peak TR velocity to >3.2 m/s
- 📝: HFpEF diagnosis is considered likely when E/e’ ratio is >14 and the peak TR velocity is >2.8 but <3.2 m/s
- Normal filling pressure: average (or septal) E/e’ is <10 and peak TR velocity is <2.8 m/s
- Increased LV filling pressures: average E/e’ ratio ≥ 14 or septal E/e’ ratio ≥ 15 and peak TR velocity > 3.2 m/s
Reporting Diastology
Obtained from 4
- All echocardiographic reports should include an assessment of diastolic function grading and filling pressure, indicating whether diastolic function is normal or abnormal with grade 1, 2 (mild to moderate increase in LAP), or 3 (marked increase in LAP).
- If unable to determine the grade of diastolic dysfunction, the status of LV filling pressure should be mentioned in the report (whether LAP is normal or elevated).
- Whenever possible, the report should mention whether a change has occurred in LV diastolic function grade in comparison with previous studies.
- Measurements that should be included in the report are mitral inflow velocities, mitral annular e’ velocity, peak TR velocity, E/A ratio, and average E/e’ ratio (unless only one side is acquired or satisfactory).
- LARS, pulmonary vein S/D ratio or systolic filling fraction, mitral inflow A duration, pulmonary vein Ar duration, and/or IVRT should be included in the report if relied on to arrive at the conclusions pertaining to diastolic function grade and mean LAP.
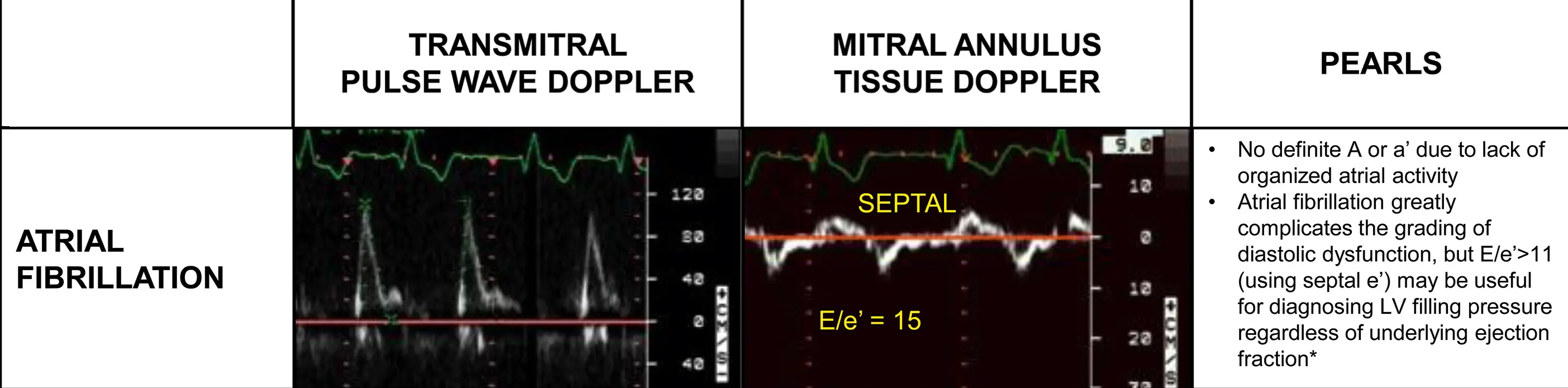
Diastolic Dysfunction ≠ ↑ Left Atrial Pressure
(Left) With normal diastolic function, LAP and LV pressure are normal with predominant early diastolic filling, short isovolumic relaxation time (IVRT), and deceleration time (DT). Mitral annulus early diastolic velocity (e′) exceeds a′. Onset of e′ precedes onset of E. (Middle) With impaired LV relaxation but normal LAP, early diastolic transmitral pressure gradient is reduced, leading to reduced E and prolonged DT and IVRT. Due to increased LA volume before LA contraction, LA contractility increases, leading to increased late diastolic transmitral pressure gradient, increased mitral A velocity, and decreased E/A ratio. e′ is delayed and reduced with increased a′. (Right) With impaired LV relaxation but increased LAP, E increases with short DT and IVRT. Due to increased late diastolic LV pressures and LA afterload, mitral A velocity decreases, leading to an increased E/A ratio. e′ is delayed and reduced with decreased a′. Increased intravascular volume in patients with grade I diastolic dysfunction leads to an increase in LAP and a pattern of predominant early LV filling (shift to right). Diuretics in patients with increased LAP shift mitral inflow pattern to one of predominant late diastolic filling.2
Footnotes
-
Mitter SS, Shah SJ, Thomas JD. A Test in Context: E/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressure. J Am Coll Cardiol. 2017 Mar 21;69(11):1451-1464. doi: 10.1016/j.jacc.2016.12.037. PMID: 28302294. ↩ ↩2 ↩3 ↩4
-
Nagueh SF. Left Ventricular Diastolic Function: Understanding Pathophysiology, Diagnosis, and Prognosis With Echocardiography. JACC Cardiovasc Imaging. 2020 Jan;13(1 Pt 2):228-244. doi: 10.1016/j.jcmg.2018.10.038. Epub 2019 Apr 12. PMID: 30982669. ↩ ↩2 ↩3 ↩4
-
Oh JK, Park SJ, Nagueh SF. Established and novel clinical applications of diastolic function assessment by echocardiography. Circ Cardiovasc Imaging. 2011 Jul;4(4):444-55. doi: 10.1161/CIRCIMAGING.110.961623. PMID: 21772012. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9 ↩10 ↩11
-
Nagueh SF, Sanborn DY, Oh JK, Anderson B, Billick K, Derumeaux G, Klein A, Koulogiannis K, Mitchell C, Shah A, Sharma K, Smiseth OA, Tsang TSM. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography and for Heart Failure With Preserved Ejection Fraction Diagnosis: An Update From the American Society of Echocardiography. J Am Soc Echocardiogr. 2025 Jul;38(7):537-569. doi: 10.1016/j.echo.2025.03.011. PMID: 40617625. ↩ ↩2 ↩3 ↩4 ↩5
-
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016 Apr;29(4):277-314. doi: 10.1016/j.echo.2016.01.011. PMID: 27037982. ↩
-
Oh JK, Miranda WR, Bird JG, Kane GC, Nagueh SF. The 2016 Diastolic Function Guideline: Is it Already Time to Revisit or Revise Them? JACC Cardiovasc Imaging. 2020 Jan;13(1 Pt 2):327-335. doi: 10.1016/j.jcmg.2019.12.004. PMID: 31918901. ↩ ↩2 ↩3
-
Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Gomez de Diego JJ, Oliva MJ, Hagendorff A, Hristova K, Lopez T, Magne J, Martinez C, de la Morena G, Popescu BA, Penicka M, Ozyigit T, Rodrigo Carbonero JD, Salustri A, Van De Veire N, Von Bardeleben RS, Vinereanu D, Voigt JU, Zamorano JL, Bernard A, Donal E, Lang RM, Badano LP, Lancellotti P. Echocardiographic reference ranges for normal cardiac Doppler data: results from the NORRE Study. Eur Heart J Cardiovasc Imaging. 2015 Sep;16(9):1031-41. doi: 10.1093/ehjci/jev083. Epub 2015 Apr 20. PMID: 25896355. ↩