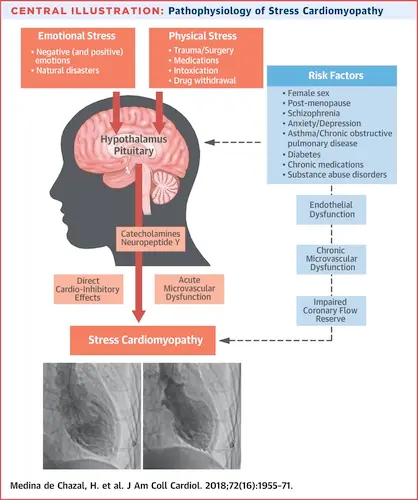
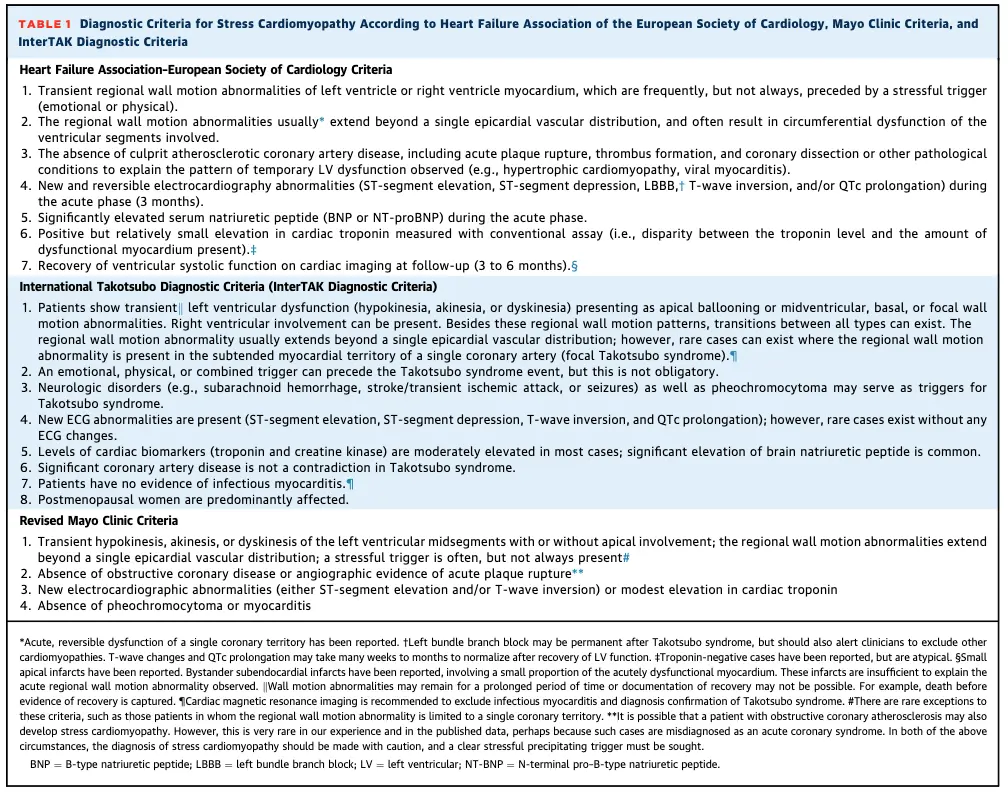
Stress cardiomyopathy is a clinical syndrome characterized by an acute and transient (<21 days) left ventricular (LV) systolic (and diastolic) dysfunction often related to an emotional or physical stressful event, most often identified in the preceding days (1 to 5 days). The presence of LV regional wall motion abnormalities characteristically extending beyond a single epicardial coronary artery distribution defines the syndrome. The typical pattern of regional LV wall motion abnormality is the apical hypokinesia/akinesia/dis-kinesia (apical ballooning) with basal hyperkinesis. Other forms of systolic dysfunction localized to the base or the midventricular regions have been described, although less frequently. The presence of a stress cardiomyopathy is suspected on the basis of the clinical context, electrocardiographic (ECG) abnormalities, mild elevation of serum cardiac troponin, significant elevation in serum natriuretic peptide levels (BNP or NT-proBNP), and noninvasive cardiovascular imaging. Coronary angiography is usually performed to exclude an acute obstruction in an epicardial coronary artery. Cases in whom regional wall motion abnormalities that extend beyond a single epicardial vascular distribution, usually in a circumferential distribution, coexist with CAD (bystander CAD), remain consistent with stress cardiomyopathy.1
- Clinical Subtypes
- Primary
- patients are usually admitted to a specialized cardiac care unit and are usually treated with aspirin and anticoagulant agents
- Secondary
- patients are already in the health care setting during evaluation or treatment of another critical illness and often present insidiously in a wide range of clinical and surgery settings
- Primary
- Complications
- acute heart failure (HF)
- left ventricular outflow tract obstruction (LVOTO)
- mitral regurgitation (MR)
- cardiogenic shock
- The typical patient with stress cardiomyopathy is a postmenopausal woman who presents with acute or subacute onset of chest pain (>75%) and/or shortness of breath (approximately 50%), often with dizziness (>25%) and occasional syncope (5% to 10%).
- Risk factors
- The typical patient with stress cardiomyopathy is a postmenopausal woman who has experienced severe, unexpected emotional stress in the prior 1 to 5 days. This is often superimposed on a background of elevated levels of stress or anxiety, or an anxiety or panic disorder, but it may also be unheralded.
- Cannabis use disorder has been identified as a risk factor for stress cardiomyopathy and is associated with a 3-fold higher risk of cardiac arrest.
Diagnosis
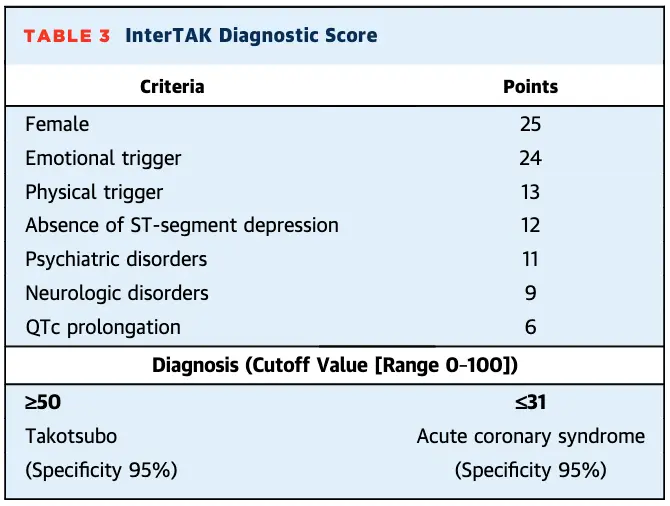
- InterTAK Diagnostic Score
Anatomical Variants
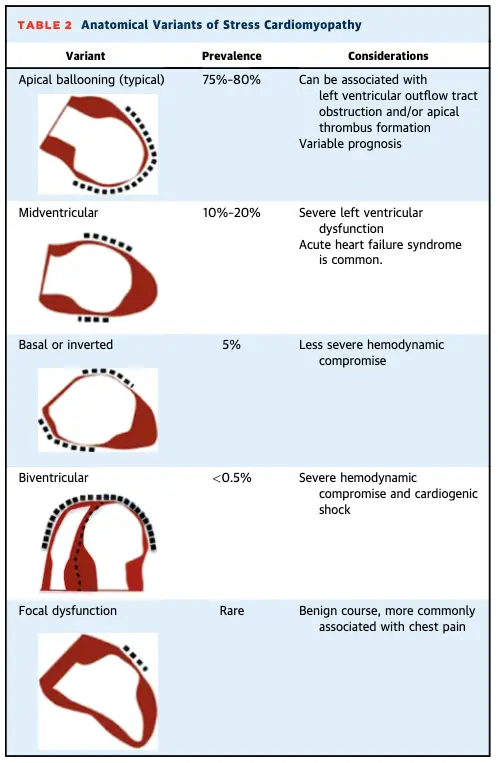
- Takotsubo” or octopus pot (75-80% of patients) - “apical ballooning” pattern
- a narrow neck and globular lower portion in the apical ballooning form
- associated with typical complications of apical akinesis (thrombus formation) and of basal hyperkinesis (LVOTO and MR due to systolic anterior movement of the mitral leaflet)
- 📝 The higher β-adrenoceptor density in the apical myocardium may account for the greater susceptibility of the apex to the cardiac sympathetic stimulation, but this finding has never been replicated in humans.
- Midventricular ballooning pattern (10-20%)
- mid-LV is hypo- or akinetic, with normal apical and basal contraction
- associated with more severe reduction in cardiac output and Cardiogenic Shock
- Basal ballooning pattern, aka ‘Inverted Takotsubo’ (<5%)
- associated with less severe hemodynamic compromise
- Other rare variants include biventricular dysfunction and isolated right ventricular (RV) compromise, which are associated with severe hemodynamic compromise and shock, and localized focal dysfunction that are more benign in nature and resemble cases of focal myocarditis
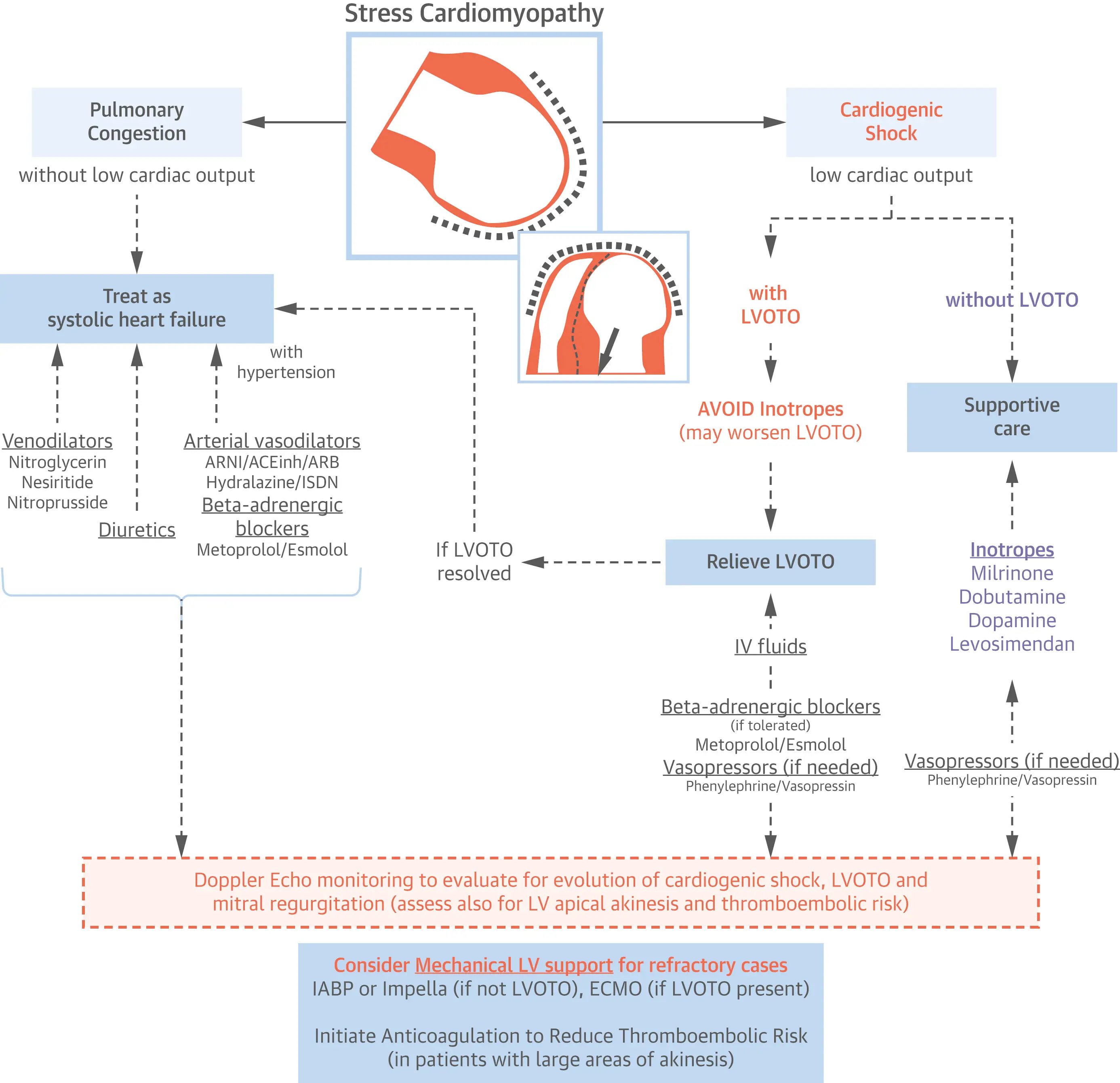
Management
Footnotes
-
Medina de Chazal, H., Del Buono, M. G., Keyser-Marcus, L., Ma, L., Moeller, F. G., Berrocal, D., & Abbate, A. (2018). Stress Cardiomyopathy Diagnosis and Treatment. Journal of the American College of Cardiology, 72(16), 1955–1971. https://doi.org/10.1016/j.jacc.2018.07.072 ↩