- The presence of significant CoA is based on evidence of upper extremity hypertension (at rest, on ambulatory BP monitoring, or with pathologic blood pressure response to exercise) or left ventricular hypertrophy and evidence for 1 of these gradient measurements:
- A noninvasive BP difference of >20 mm Hg between the upper and lower extremities
- A peak-to-peak gradient of >20 mm Hg across the coarct by catheterization; or a peak-to-peak gradient of >10 mm Hg across the coarct by catheterization in the setting of decreased left ventricular systolic function or significant collateral flow
- A mean gradient of >20 mm Hg across the coarct by Doppler echocardiography; or a mean gradient of >10 mm Hg across the coarct by Doppler echocardiography in the setting of decreased left ventricular systolic function or significant collateral flow
Echo
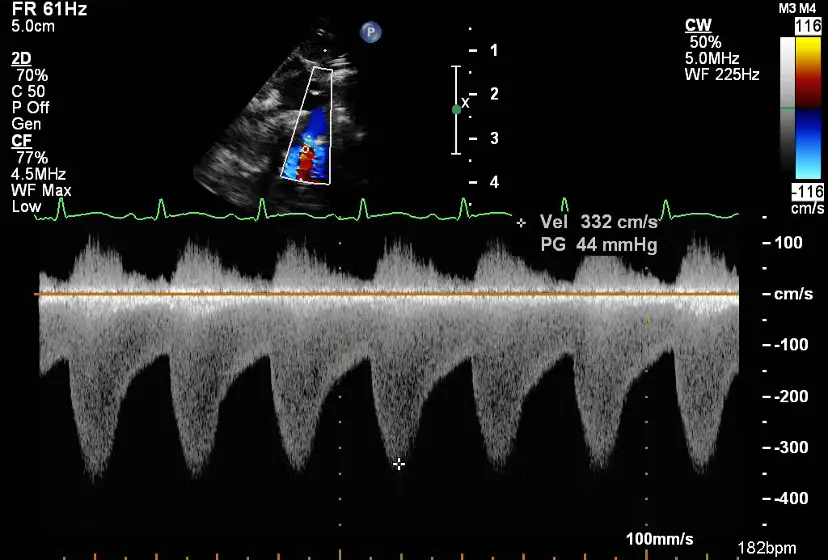
- Continuous-wave Doppler enables assessment of transaortic gradients and abdominal aortic flow.
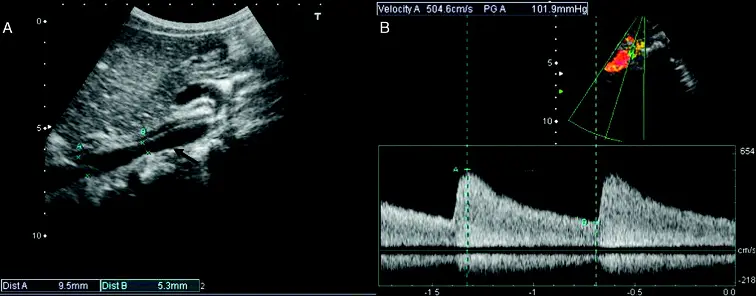
- Suprasternal Doppler for Coarctation of the Aorta
- The Doppler doesn’t go back to baseline, i.e. doesn’t get back to
- Coarctation of aorta for abdominal aorta U/S will be flipped (i.e. positively oriented) and less prominent (as your measuring further away from the coarctation), but similarly won’t return back to baseline
Cath Hemodynamics
- Cardiac catheterization–derived peak-to-peak gradient (reflecting the pressure difference proximal and distal to the site of coarctation) remains the “gold standard” for the hemodynamic assessment of aortic coarctation severity.
- 📝 the mean gradient by echocardiography has the best correlation with the peak-to-peak gradient obtained at catheterization