- The shape of the action potential determines the conduction velocity, refractory, and automaticity of cardiac tissue
- Phase 0: raid depolarization, INa channels
- Phase 1: early repolarization, Ito channels
- rapid inactivation of the INa channels and activation of the Transient Outward K current ( for short)
- Ito channels play an important role in Brugada Syndrome
- Phase 2: plateau phase, ICa channels
- Inward (depolarizing current): late inactivating Na channels and also from L-type Ca current
- Outward (repolarizing current): derive from K channels (including inactivation of Ito channels and slow activation of IKs and IKr channels). Also affected by Na-Ca exchange and Na-K exchange as well.
- Phase 3: late repolarization, IKr and IKs channels
- Phase 4: resting membrane potential,
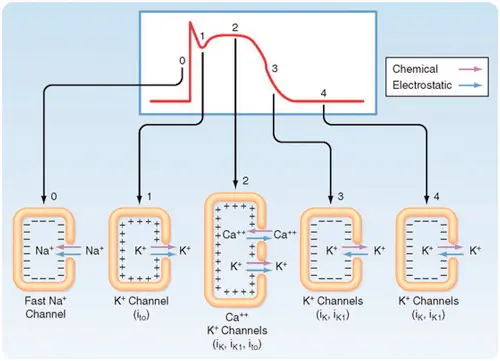
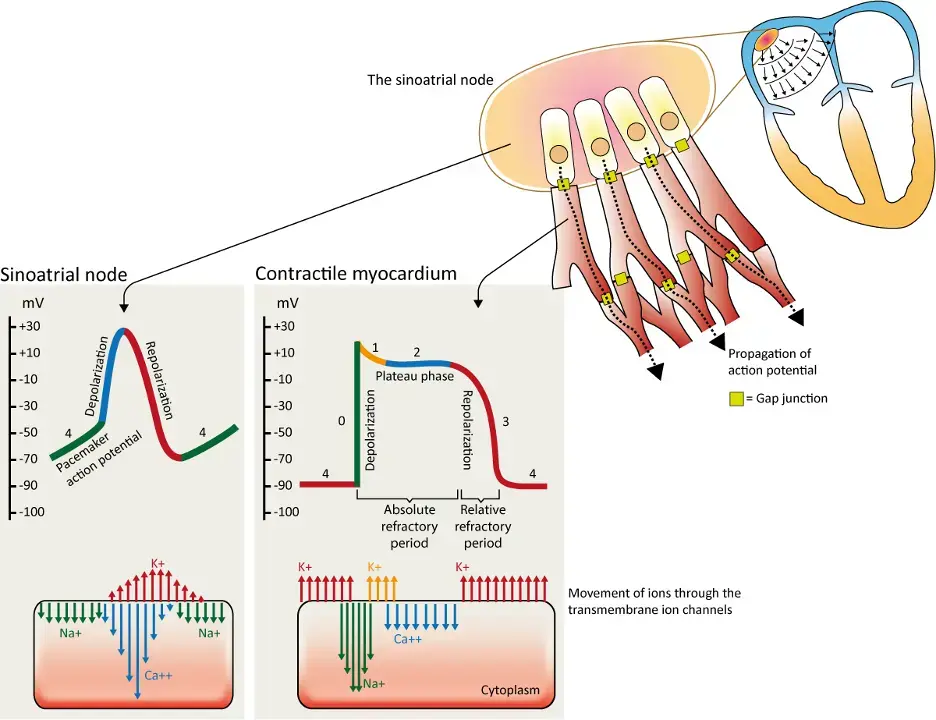
Depolarization occurs when rapid Na channels open and and Na+ ions rush into the cell. Phase 0 of the cardiac action potential, the speed of depolarization of the cell is reflected by the slope of phase 0 of the action potential, and determines how soon the next cardiac cell will be polarized, and thus determines the speed at which the electrical impulses propagate across the heart. If we do something to change the speed in which sodium ions enter the cell (∆ the slope of phase 0), we therefore change the speed of conduction (the conduction velocity) of cardiac tissue.
Repolarization is represented by Phase 1-3. Once a cell is depolarized, it cannot be depolarized again until the ionic fluxes that occurred during depolarization are reversed, i.e. repolarization. Because a second depolarization cannot take place until repolarization occurs, the time from end of phase 0 to late in phase 3 is called the refractory period of cardiac tissue.
Phase 2 is the plateau phase and is unique to cardiac cells. Phase 2 gives “duration” to the cardiac cells. It is mediated by the slow calcium channels, which allow positively charged calcium ions to slowly enter the cell, thus interrupting repolarization and prolonging the refractory period.
In some cardiac cells, Phase 4 is kinda flat and quiescent, but in the SA node, there is leakage of ions back-and-forth across the cell membrane during phase 4 → causes a gradual increase in the transmembrane potential, which if high enough triggers activation of channels causing the cell to depolarize → depolarization of nearby cells → generates electrical impulses that can be proximal irrigated across the heart. This phase for activity, which leads to spontaneous depolarization, is called automaticity.
The action potential actually looks different depending on the area of the heart. The one we often draw is the AP for the Purkinje fiber. Notably, the APs in the SA and AV node don’t have that rapid Phase 0 depolarization as these tissues lack the rapid sodium channels responsible for rapid Phase 0 depolarization. Instead the SA and AV nodes are thought to be entirely dependent on calcium channels for depolarization.
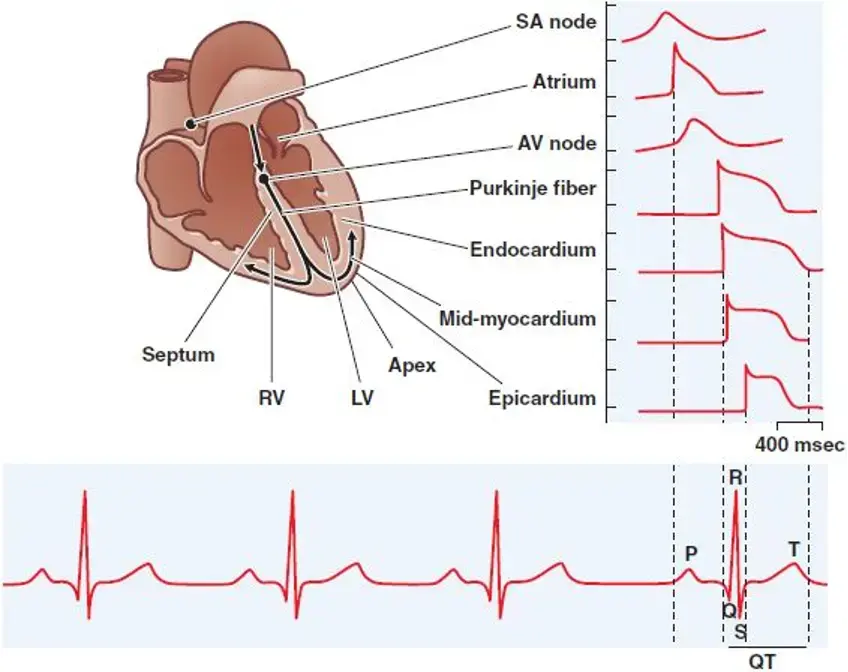
- In the SA node, there is gradual depolarization during electrical diastole (upsloping during Phase 4), which is mediated by the “funny current”, channel. Fun fact: the channel is the target of ivabradine.
- Increased sympathetic tone → ↑ rate of Phase 4 diastolic depolarization → ↑ HR
- Phase 4 diastolic depolarization can also develop in some disease states, and in that case, it is called abnormal automaticity.