- Cellular mechanisms of bradyarrhythmias can be thought of as falling under one of two buckets: either impulses aren’t being formed or conducted
- ↓ impulse formation
- Hyperpolarization of cell membrane (e.g. SA Node as a consequence of hyperkalemia)
- ↓ impulse conduction (sometimes called ‘exit block’)
- Impaired intercellular communication (ion channels, gap junctions etc. that prevent or impair electrical conduction through myocardial tissue
- ↓ impulse formation
Sinus node dysfunction is most often related to age-dependent progressive fibrosis of the sinus nodal tissue and surrounding atrial myocardium leading to abnormalities of sinus node and atrial impulse formation and propagation and will therefore result in various bradycardic or pause-related syndromes.
Both sleep disorders of breathing and nocturnal bradycardias are relatively common, and treatment of sleep apnea not only reduces the frequency of these arrhythmias but also may offer cardiovascular benefits. The presence of nocturnal bradycardias should prompt consideration for screening for sleep apnea, beginning with solicitation of suspicious symptoms. However, nocturnal bradycardia is not in itself an indication for permanent pacing.
The presence of left bundle branch block on electrocardiogram markedly increases the likelihood of underlying structural heart disease and of diagnosing left ventricular systolic dysfunction. Echocardiography is usually the most appropriate initial screening test for structural heart disease, including left ventricular systolic dysfunction.
In sinus node dysfunction, there is no established minimum heart rate or pause duration where permanent pacing is recommended. Establishing temporal correlation between symptoms and bradycardia is important when determining whether permanent pacing is needed.
In patients with a left ventricular ejection fraction between 36% to 50% and atrioventricular block, who have an indication for permanent pacing and are expected to require ventricular pacing >40% of the time, techniques that provide more physiologic ventricular activation (e.g., cardiac resynchronization therapy, His bundle pacing) are preferred to right ventricular pacing to prevent heart failure.
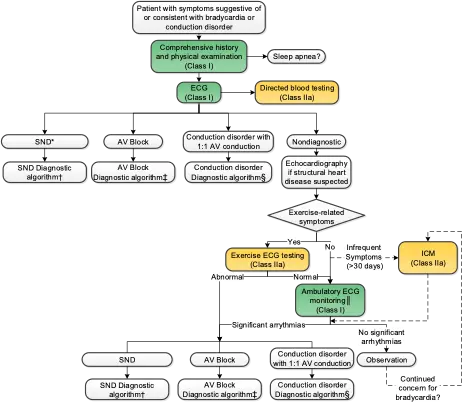
- Initial evaluation with comprehensive H&P and ECG →
- Sinus Node Dysfunction (SND)
- AV block
- Conduction disorder with 1:1 block
Note
Bradycardia (symptomatic/asymptomatic)
- ECG: ***
- Labs: TSH/fT4, BMP, Lyme titer
- Echo if LBBB, Mobitz 2, High-degree AV block or CHB
- Dispo: Sleep clinic referralCauses
Medications Causing Bradycardia
| Antihypertensive | Antiarrhythmic | Psychoactive | Other |
|---|---|---|---|
| - Beta-blockers (including BB eye drops used for glaucoma) - Clonidine - Methyldopa - Non-dihydropyridine calcium channel blockers - Reserpine | - Adenosine - Amiodarone - Dronedarone - Flecainide - Procainamide - Propafenone - Quinidine - Sotalol | - Donepezil - Lithium - Opioid analgesics - Phenothiazine antiemetics and antipsychotics - Phenytoin - Selective serotonin reuptake inhibitors - Tricyclic antidepressants | - Anesthetic drugs (propofol) - Cannabis - Digoxin - Ivabradine - Muscle relaxants (e.g., succinylcholine) |
Conditions Associate with Bradycardia
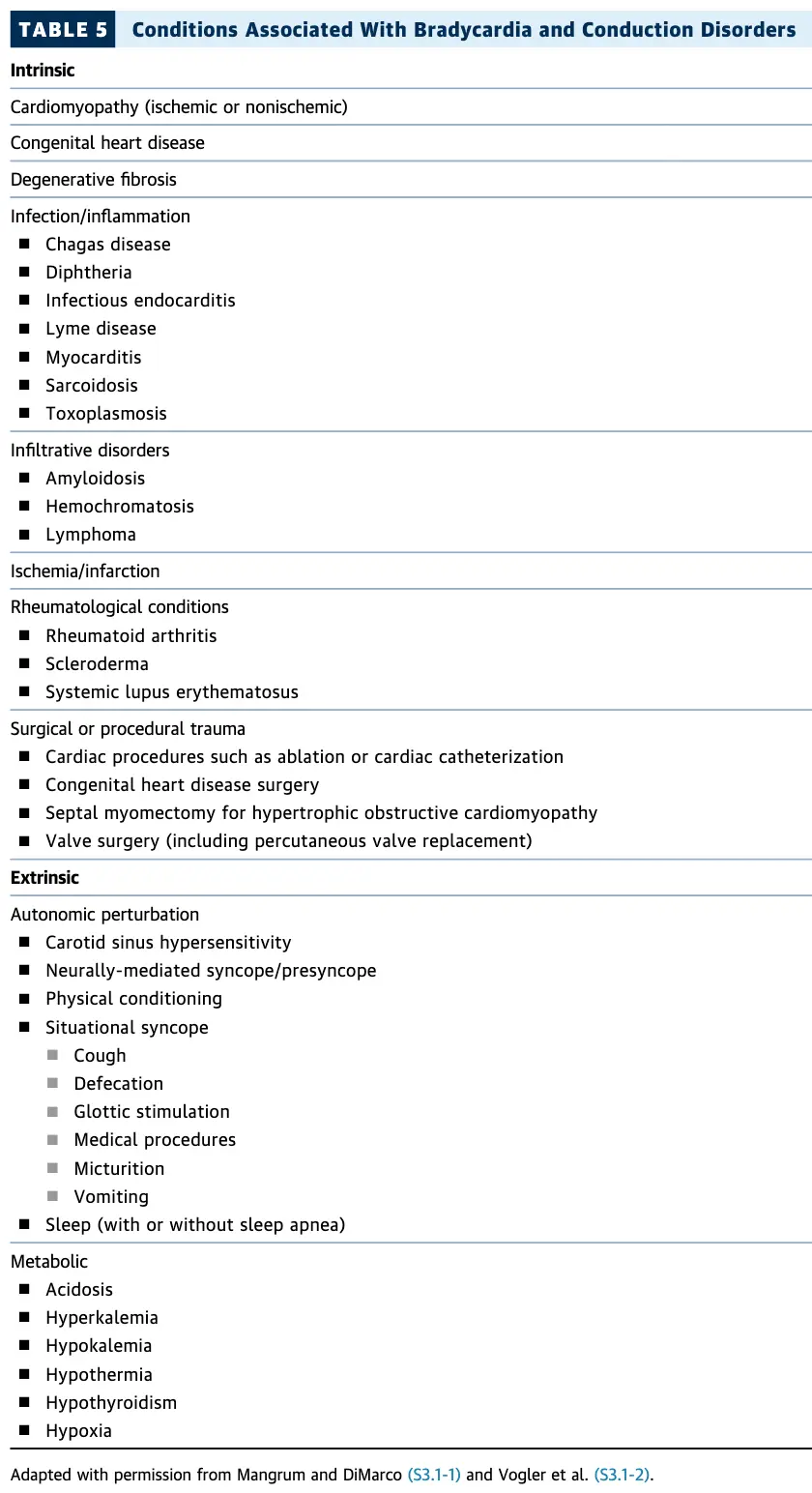
Etiologies
Sinus Node Dysfunction (SND)
See Sinus Node Dysfunction (SND)
Atrioventricular Block
In patients with acquired second-degree Mobitz type II atrioventricular block, high-grade atrioventricular block, or third-degree atrioventricular block not caused by reversible or physiologic causes, permanent pacing is recommended regardless of symptoms. For all other types of atrioventricular block, in the absence of conditions associated with progressive atrioventricular conduction abnormalities, permanent pacing should generally be considered only in the presence of symptoms that correlate with atrioventricular block.
Conduction Disorder
Work-up
ECG
- In patients with suspected bradycardia or conduction disorder, a 12-lead ECG is recommended to document rhythm, rate, and conduction, and to screen for structural heart disease or systemic illness. (Class I) 1
Exercise ECG testing
- In patients with suspected chronotropic incompetence, exercise electrocardiographic testing is reasonable to ascertain the diagnosis and provide information on prognosis. (Class 2a)
- In patients with exercise-related symptoms suspicious for bradycardia or conduction disorders, or in patients with 2:1 atrioventricular block of unknown level, exercise electrocardiographic testing is reasonable. (Class 2a)
Echo
- Class 1 indications:
- Newly identified LBBB, second-degree Mobitz type II atrioventricular block, high-grade atrioventricular block, or third-degree atrioventricular block with or without apparent structural heart disease or coronary artery disease
- Class 2a indications
- Reasonable to get TTE if bradycardia or conduction disorders secondary to causes other than those with a Class 1 indication
- Class 3
- Routine cardiac imaging is NOT indicated for “patients with asymptomatic sinus bradycardia or first-degree atrioventricular block and no clinical evidence of structural heart disease.”
Ambulatory ECG Monitoring
Genetic Testing
- “In patients in whom a conduction disorder-causative mutation has been identified, genetic counseling and mutation-specific genetic testing of first-degree relatives is recommended to identify similarly affected individuals.” (Class 1)
- “In patients with inherited conduction disease, genetic counseling and targeted testing may be considered to facilitate cascade screening of relatives as part of the diagnostic evaluation.” (Class 2b)
Sleep apnea screening
Implantable Loop Recorder (ILR)
- “In patients with infrequent symptoms (>30 days between symptoms) suspected to be caused by bradycardia, long-term ambulatory monitoring with an implantable cardiac monitor (ICM) is reasonable if initial noninvasive evaluation is nondiagnostic.” (Class 2a)
Management
Acute Bradycardia Management
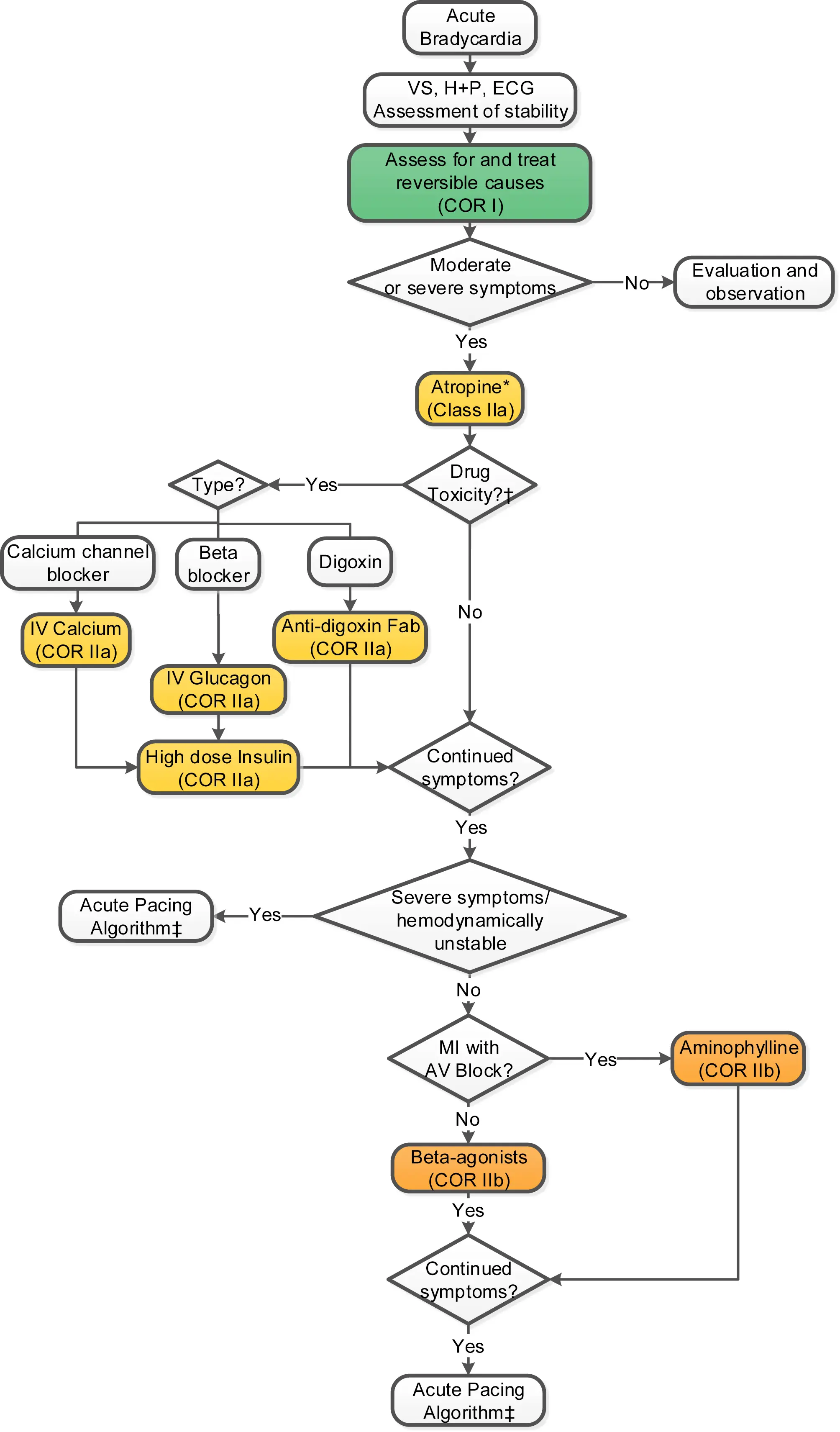
Symptomatic sinus bradycardia or AV Block
| Medication | Dosage | Comments |
|---|---|---|
| Atropine | 0.5-1 mg IV (may be repeated every 3-5 min to a maximum dose of 3 mg) | |
| Dopamine | 5 to 20 mcg/kg/min IV. starting at 5 mcg/kg/min and increasing by 5 mcg/kg/min every 2 min | Dosages of >20 mcg/kg/min may result in vasoconstriction or arrhythmias |
| Isoproterenol | 20-60 mcg IV bolus followed doses of 10-20 mcg, or infusion of 1-20 mcg/min based on heart rate response | Monitor for potential development of ischemic chest pain |
| Epinephrine | 2-10 mcg/min IV or 0.1-0.5 mcg/kg/min IV titrated to desired effect |
Second degree or Third degree (3˚) AV Block in setting of Inferior MI
| Medication | Dosage |
|---|---|
| Aminophylline | 250-mg IV bolus |
| Calcium channel blocker overdose | |
| 10% calcium chloride | 1-2 g IV every 10-20 min or an infusion of 0.2-0.4 mL/kg/h |
| 10% calcium gluconate | 3-6 g IV every 10-20 min or an infusion at 0.6-1.2 mL/kg/h |
BB or CCB overdose
| Medication | Dosage | Comments |
|---|---|---|
| Glucagon | 3-10 mg IV with infusion of 3-5 mg/h | |
| High dose insulin therapy | IV bolus of 1 unit/kg followed by an infusion of 0.5 units/kg/h | Follow glucose and potassium levels |
Digoxin overdose
| Medication | Dosage | Comments |
|---|---|---|
| Digoxin antibody fragment | Dosage is dependent on amount ingested or known digoxin concentration | - One vial binds approximately 0.5 mg of digoxin. - Administer over at least 30 min - May be repeated |
Post-Heart Transplant
| Medication | Dosage | Comments |
|---|---|---|
| Aminophylline | 6 mg/kg in 100-200 mL of IV fluid over 20-30 min | |
| Theophylline | 300 mg IV, followed by oral dose of 5-10 mg/kg/d titrated to effect | - Therapeutic serum levels range from 10-20 mcg/mL - Usual posttransplant dosages average 450 mg±100 mg/d |
Spinal Cord Injury
| Medication | Dosage | Comments |
|---|---|---|
| Aminophylline | 6 mg/kg in 100-200 mL of IV fluid over 20-30 min | |
| Theophylline | Oral dose of 5-10 mg/kg/d titrated to effect | Effective dosages often result in serum levels below the usual effective range of 10-20 mcg/mL |
Temporary Pacing
- TVP
- “In patients with persistent hemodynamically unstable SND refractory to medical therapy, temporary transvenous pacing is reasonable to increase heart rate and improve symptoms until a PPM is placed or the bradycardia resolves.” (Class 2a)
- Temporary cutaneous pacing (used as a bridge to TVP or PPM)
- “In patients with SND with severe symptoms or hemodynamic compromise, temporary transcutaneous pacing may be considered to increase heart rate and improve symptoms until a temporary transvenous or PPM is placed or the bradycardia resolves.” (Class 2b)
Footnotes
-
Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, Goldschlager NF, Hamilton RM, Joglar JA, Kim RJ, Lee R, Marine JE, McLeod CJ, Oken KR, Patton KK, Pellegrini CN, Selzman KA, Thompson A, Varosy PD. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. J Am Coll Cardiol. 2019 Aug 20;74(7):932-987. doi: 10.1016/j.jacc.2018.10.043. Epub 2018 Nov 6. Erratum in: J Am Coll Cardiol. 2019 Aug 20;74(7):1014-1016. doi: 10.1016/j.jacc.2019.06.046. PMID: 30412710. ↩