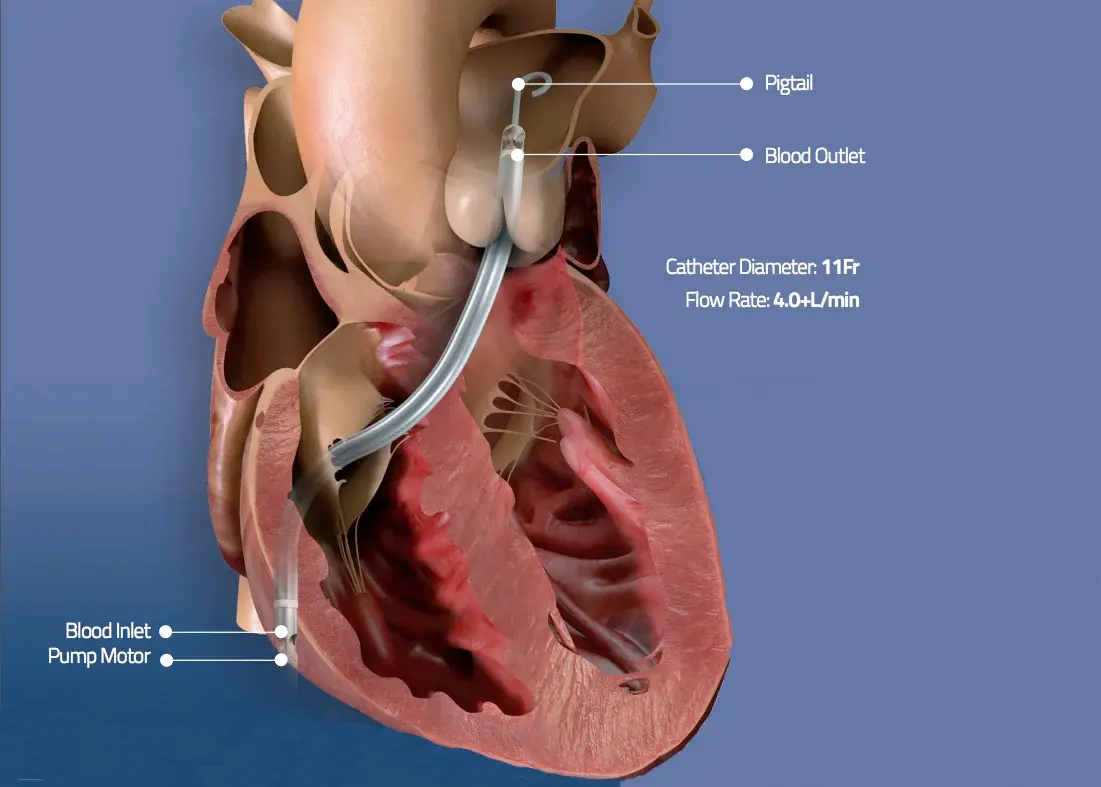
- Impella microaxial flow pumps are placed fluoroscopically in retrograde fashion through the femoral artery, axillary artery, or ascending aorta
- Blood 🩸 is suctioned from an inlet (located just superior to the catheter’s pigtail in the LV cavity) and then delivered through the Impella outlet, which is seated just above the aortic valve.
- The distal portion of the Impella is a pigtail configuration that is meant to reside in the mid LV approximately 3.5 cm below the aortic annulus. The Impella 5.5 should be 5 cm from the aortic valve annulus.
- Uses: high-risk PCI, post-MI shock, ADHF, post-cardiotomy shock, etc.
- Complications
- hemolysis
- pigment-induced nephropathy
- vascular access complications, e.g. limb ischemia, major bleeding
- pericardial tamponade
- MV impingement w/ mitral regurgitation
- thrombosis → device failure
Note
“BiPELLA”: combination of LV and RV Impella support devices
- Catheter based ventricular assist device based off of Archimedes screws
- Rotating impellar with a microaxial motor moves
- blood from LV to aorta
- Continuously draws blood from the LV inlet port
- and expels into the ascending aorta via the
- outlet port
- 2.5, CP, 5.0, 5.5, and RP
- Unloads the LV by continuously drawing blood from LV
- Reduces LV work and myocardial oxygen demand
- Increases MAP and CO
- Improved systemic perfusion and coronary blood flow
- Decreases PCWP
- Reduction in RV afterload
- Purge solution is used through the impella catheter
- One or the other - NOT used together
- D5W with 25 or 50 IU/ml Heparin
- D5W with 25 or 50 mEq/L Sodium Bicarbonate
- especially if indication not to use heparin
- One or the other - NOT used together
Impella CP
- CP - Catheter diameter is 9 Fr, 14 Fr pump motor
- 14 Fr sheath
- Peak flows up to 4.3 L/min
- CP Advantages
- Quick Percutaneous placement
- Axillary or femoral
- CP Disadvantages
- Expensive ($25k)
- Higher vascular complications
- Can move with femoral placement
- More hemolysis and thrombocytopenia
- Difficulty mobilizing
Impella 5.5
- 5.5 - catheter diameter is 9 Fr, 19 Fr pump motor
- 21 Fr cannula in 10mm Hemashield graft
- Peak flows up to 6.0 L/min (even though its called “5.5”)
- 5.5 Advantages
- Stable positioning
- Good flows
- No pigtail
- Patient can mobilize
- 5.5 Disadvantages
- Expensive ($45k)
- Surgical placement and removal
Indications
- Cardiogenic Shock
- Treatment of acute MI complicated by cardiogenic shock
- Facilitate high risk PCI
- Cardiomyopathy with acute decompensation
- Postcardiotomy cardiogenic shock
- Off pump CABG
- Hemodynamic support during ablation for VT
- Temporary mechanical support as bridge to VAD or transplant
- Temporary mechanical support as bridge to recovery
Contraindications
- Presence of thrombus in the LV
- Moderate to severe aortic insufficiency
- Will worsen Al and LV dilation
- Aortic Stenosis with AVA 0.6cm
2or less - Severe PVD
- May still place axillary or direct aortic approaches
- Presence of mechanical aortic valve
- ASD or VSD
- LV rupture or cardiac tamponade
Impella RP Right Ventricular Support Device
- delivers blood from the cannula inlet seated in the inferior vena cava to the outlet located above the pulmonic valve within the proximal pulmonary artery.
- The pump is inserted under fluoroscopic guidance via the femoral vein into the right atrium, across the tricuspid and pulmonic valves, and then into the pulmonary artery.
Note
Because access is presently available only via the femoral vein, patients are not able to ambulate.
Resuscitation (CPR, AED) in a patient with Impella
CPR should be performed based on loss of perfusion pressure and/or flow, rather than on electrocardiogram or flattening of the arterial waveform, since the device can often maintain adequate perfusion pressures despite ventricular tachycardia.
- ==Consider reducing Impella P-level to P-2 during CPR== to minimize potential damage to cardiac structures (especially when suction alarm) and increase the level of support again at return of circulation.
- This also resolves the arrhythmia when it was induced by suction events. (Continuing support, however, can be considered for patients that have extremely poor native heart function).
- An Impella device is not a contraindication for electrical defibrillation.
- Assess Impella position after return of circulation, to ensure the Impella has not dislodged during CPR.
Repositioning an Impella
- ↓ to P2
- Unlock the fasteners to allow you to rotate the wire
- Teamwork:
- Have one person press down on the blue button 🔵
- Have another person holding the Echo probe so you can see the Impella device to ensure appropriate repositioning
- You can rotate the wire to reposition
- Once done getting the Impella repositioned:
- release the blue button 🔵,
- fasten everything back up,
- slowly ramp back up the P-level, e.g. ↑ by 2 every 2 minutes or so
Impella Controller
- Changing the P-level → Impella Flow (bottom left of controller) should adjust as well
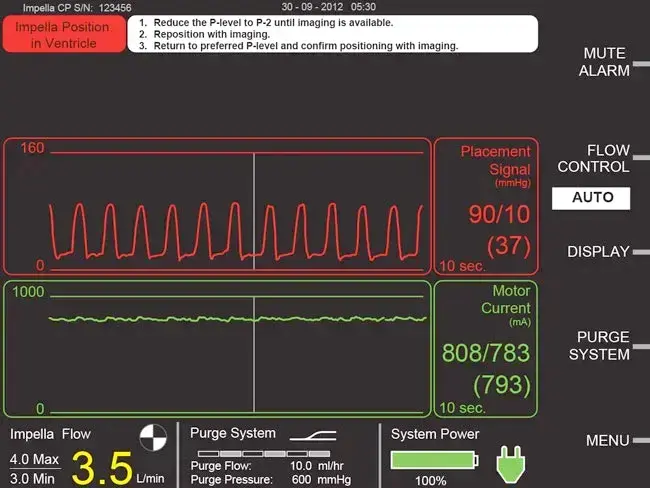
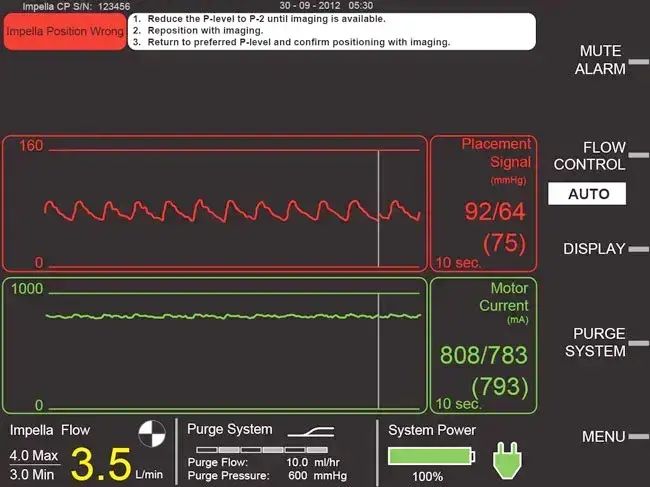
- Waveforms (Source)
- Placement Signal (red 🔴)
- Ao and LV waveforms
- The Ao waveform is from the optical sensor where the cannula and outflow meet
- The LV waveform is derived from optical sensor and motor current
- Motor Current (green 🟢)
- the amount of energy and flow through the cannula
- peaks on motor current waveform are when valve open, valleys are when valve closed
- Normal: pulsatile waveform
- If flat waveform, then something is up. For example, malpositioned such that aortic valve no longer creating pressure gradient across the cannula
- Placement Signal (red 🔴)
- Bottom of screen (Source)
- Impella Flow: max flow on top, min flow on bottom, average flow is what’s more prominently displayed
- Purge System
- Purge Flow: the rate of the purge solution
- Purge Pressure: the pressure built up behind the purge
- Cardiac Output
- CPO
Troubleshooting
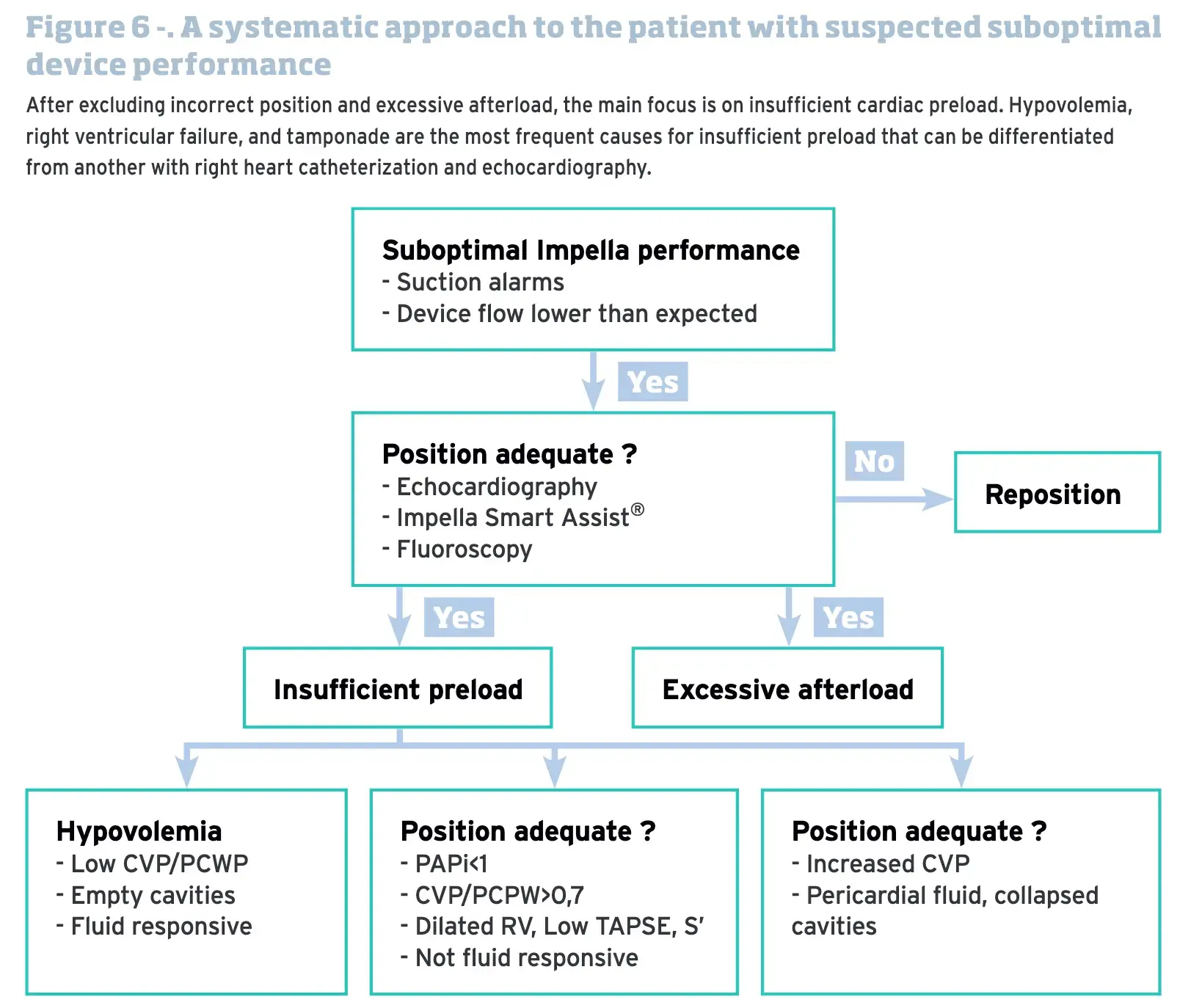
Impella Alarms
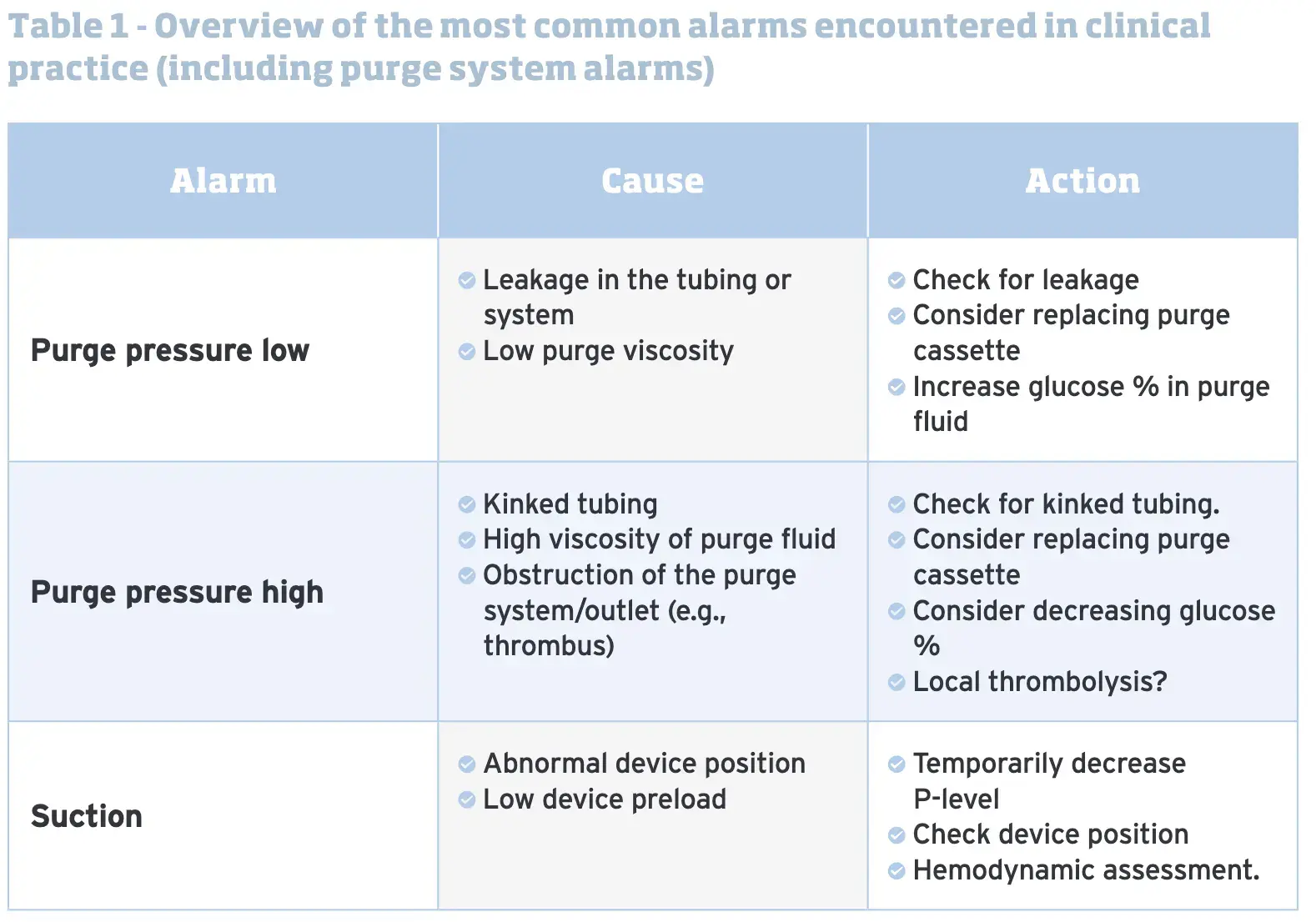
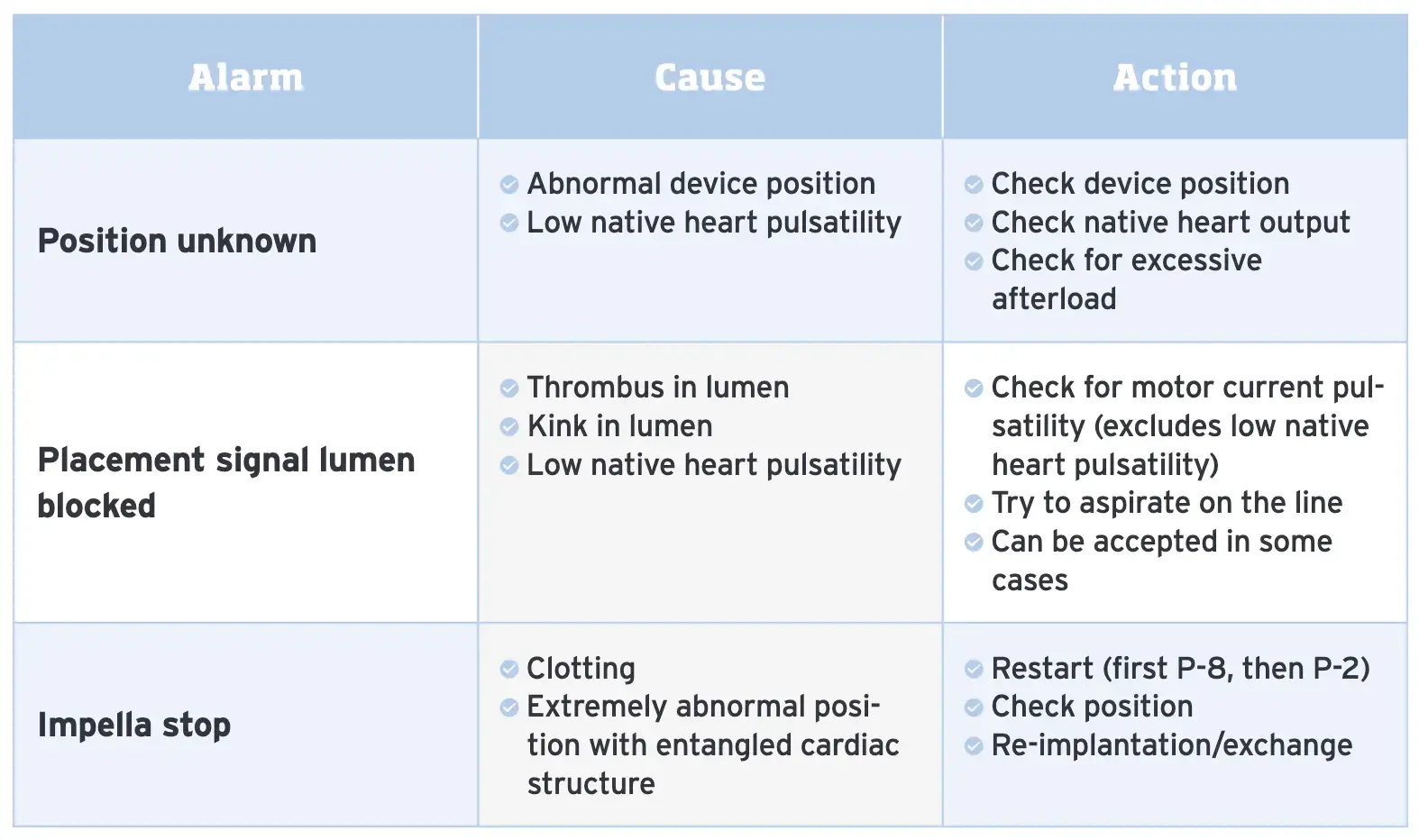
Position unknown (white banner)
- Often arises in situations where the patient has low native heart pulsatility
- When a patient has poor native ventricular function, the placement signal may remain pulsatile; however, the amplitude will be dampened.
- The green waveform may even appear as if its almost a flat line
Impella Position In Ventricle (red banner)
- Arises if catheter is fully in the ventricle
Impella Position Wrong (red banner)
- Arises in the following circumstances:
- catheter completely in the aorta
- if the inlet and outlet areas are in the ventricle and the open pressure area is in the aorta
Suction Alarms (yellow banner)
Suction events are amongst the most common problems encountered during Impella mana- gement in the cardiac intensive care unit and should be avoided at any time. Longer standing suction events can lead to haemolysis and insufficient circulatory support. (Source)
- Common causes
- Contact of the Impella device inlet with a ventricular structure (mitral valve leaflet, chordal structure, ventricular wall,…).
- Abnormal / altered device positions.
- Insufficient preload.
- Device related thrombus formation.
- Excessive support to a recovering heart.
- Potential harms that may arise
- Decrease the level of support that is provided to the circulation, which may result in hemodynamic deterioration.
- Increase shear stress for red blood cells, resulting in hemolysis. It is also possible to encounter hemolysis without overt suction alarms in case of subtle abnormalities.
- The preferred test to quantify hemolysis is the plasma free hemoglobin (PfHb).
Purge Alarms
Excessive purge system pressures
- Causes
- Kinked tubing
- High viscosity of purge fluid
- Obstruction of the purge system/outlet (e.g., thrombus)
- Diagnosis/Solution:
- Check for kinked tubing
- Consider decreasing glucose viscosity if higher than 5%
- Consider replacing the purge cassette
- Local thrombolysis is used by some centrers with good results; but data remain scarce
Low purge system pressures
- Causes:
- Leakage somewhere in the purge system
- Low purge solution viscosity
- Diagnosis/Solution:
- Check for leakage in the system
- Consider replacing the purge cassette
- Consider increasing the glucose viscosity in the purge fluid if less than 20%
HARVI with Burkhoff
- Pump Flow and “HQ Curve”
- H stands for pressure head and Q stands for flow
- HQ curve is the hemodynamic signature of the pump
- Curve modified by the RPMs
- Hemodynamic effect
- ventricle is unloading: ↓ volume in the ventricle, ↓ PCWP
- ∆ in shape from rectange to triangle b/c “continuously unloading” (always pumping independent of phase in the cardiac cycle) and loss of isovolumetric contraction and isovolumetric relaxation
- LV-aortic pressure uncoupling (doesn’t always occur)
- ↑ aortic pressure
- ↓ LV pressure
- during cardiac cycle pressure gradient varies (large pressure gradient during diastole, small gradient during systole d/t ∆ in LV pressure)
- Flow waveform tells you about the placement of the impella device
- flat line (no pressure gradient) at a high flow (it’ll pump a lot of blood) if misplaced in the aorta
- flat line can also occur d/t other causes, e.g. if no LV contraction, severe RHF where LV is completely underfilled; i.e. any condition where not able to generate phasic pressure ∆
- Energetic effects
- ↓ PVA, ↓ MVO2