Definitions
| Term | Definition/Comments and References |
|---|---|
| Syncope | A symptom that presents with an abrupt, transient, complete loss of consciousness, associated with inability to maintain postural tone, with rapid and spontaneous recovery. The presumed mechanism is cerebral hypoperfusion.There should not be clinical features of other nonsyncope causes of loss of consciousness, such as seizure, antecedent head trauma, or apparent loss of consciousness (ie, pseudosyncope). |
| Loss of consciousness | A cognitive state in which one lacks awareness of oneself and one’s situation, with an inability to respond to stimuli. |
| Transient loss of consciousness | Self-limited loss of consciousness can be divided into syncope and nonsyncope conditions. Nonsyncope conditions include but are not limited to seizures, hypoglycemia, metabolic conditions, drug or alcohol intoxication, and concussion due to head trauma. The underlying mechanism of syncope is presumed to be cerebral hypoperfusion, whereas nonsyncope conditions are attributed to different mechanisms. |
| Presyncope (near-syncope) | The symptoms before syncope. These symptoms could include extreme lightheadedness; visual sensations, such as “tunnel vision” or “graying out”; and variable degrees of altered consciousness without complete loss of consciousness. Presyncope could progress to syncope, or it could abort without syncope. |
| Unexplained syncope (syncope of undetermined etiology) | Syncope for which a cause is undetermined after an initial evaluation that is deemed appropriate by the experienced healthcare provider. The initial evaluation includes but is not limited to a thorough history, physical examination, and ECG. |
| Orthostatic intolerance | A syndrome consisting of a constellation of symptoms that include frequent, recurrent, or persistent lightheadedness, palpitations, tremulousness, generalized weakness, blurred vision, exercise intolerance, and fatigue upon standing. These symptoms can occur with or without orthostatic tachycardia, OH, or syncope. Individuals with orthostatic intolerance have ≥1 of these symptoms associated with reduced ability to maintain upright posture. |
| Orthostatic tachycardia | A sustained increase in heart rate of ≥30 bpm within 10 min of moving from a recumbent to a quiet (nonexertional) standing position (or ≥40 bpm in individuals 12–19 y of age). |
| Orthostatic hypotension (OH) | A drop in systolic BP of ≥20 mm Hg or diastolic BP of ≥10 mm Hg with assumption of an upright posture. |
| Initial (immediate) OH | A transient BP decrease within 15 s after standing, with presyncope or syncope. |
| Classic OH | A sustained reduction of systolic BP of ≥20 mm Hg or diastolic BP of ≥10 mm Hg within 3 min of assuming upright posture. |
| Delayed OH | A sustained reduction of systolic BP of ≥20 mm Hg (or 30 mm Hg in patients with supine hypertension) or diastolic BP of ≥10 mm Hg that takes >3 min of upright posture to develop. The fall in BP is usually gradual until reaching the threshold. |
| Neurogenic OH | A subtype of OH that is due to dysfunction of the autonomic nervous system and not solely due to environmental triggers (eg, dehydration or drugs). Neurogenic OH is due to lesions involving the central or peripheral autonomic nerves. |
| Cardiac (cardiovascular) syncope | Syncope caused by bradycardia, tachycardia, or hypotension due to low cardiac index, blood flow obstruction, vasodilatation, or acute vascular dissection. |
| Noncardiac syncope | Syncope due to noncardiac causes, which include reflex syncope, OH, volume depletion, dehydration, and blood loss. |
| Reflex (neurally mediated) syncope | Syncope due to a reflex that causes vasodilation, bradycardia, or both. |
| Vasovagal syncope (VVS) | The most common form of reflex syncope mediated by the vasovagal reflex. VVS: 1) may occur with upright posture (standing or seated or with exposure to emotional stress, pain, or medical settings; 2) typically is characterized by diaphoresis, warmth, nausea, and pallor; 3) is associated with vasodepressor hypotension and/or inappropriate bradycardia; and 4) is often followed by fatigue. Typical features may be absent in older patients.24 VVS is often preceded by identifiable triggers and/or by a characteristic prodrome. The diagnosis is made primarily on the basis of a thorough history, physical examination, and eyewitness observation, if available. |
| Carotid sinus syndrome | Reflex syncope associated with carotid sinus hypersensitivity.30 Carotid sinus hypersensitivity is present when a pause ≥3 s and/or a decrease of systolic pressure ≥50 mm Hg occurs upon stimulation of the carotid sinus. It occurs more frequently in older patients. Carotid sinus hypersensitivity can be associated with varying degrees of symptoms. Carotid sinus syndrome is defined when syncope occurs in the presence of carotid sinus hypersensitivity. |
| Situational syncope | Reflex syncope associated with a specific action, such as coughing, laughing, swallowing, micturition, or defecation. These syncope events are closely associated with specific physical functions. |
| Postural (orthostatic) tachycardia syndrome (POTS) | A clinical syndrome usually characterized by all of the following: 1) frequent symptoms that occur with standing (eg, lightheadedness, palpitations, tremulousness, generalized weakness, blurred vision, exercise intolerance, and fatigue); and 2) an increase in heart rate of ≥30 bpm during a positional change from supine to standing (or ≥40 bpm in those 12–19 y of age); and 3) the absence of OH (>20 mm Hg reduction in systolic BP). Symptoms associated with POTS include those that occur with standing (eg, lightheadedness, palpitations); those not associated with particular postures (eg, bloating, nausea, diarrhea, abdominal pain); and those that are systemic (eg, fatigue, sleep disturbance, migraine headaches).37 The standing heart rate is often >120 bpm.31,38–42 |
| Psychogenic pseudosyncope | A syndrome of apparent but not true loss of consciousness that may occur in the absence of identifiable cardiac, reflex, neurological, or metabolic causes. |
Mimics or Look-Alikes
- Drug intoxication
- Alcohol intoxication
- Seizure
- Trauma
- Falls
- Psychiatric conditions
- Pseudo-syncope
- Pseudo-seizure
Work-up
- History
- Syncope during exercise → think cardiac etiology
- Syncope after exercise → think situational syncope
- Nausea, flushing, or sweats → think vasovagal
- frequently prodrome is long enough to get into safe position
- Abrupt symptoms/syncope (minimal if any prodrome) → think arrhythmia / cardiac
- 📝 seizure usually lacks a prodrome
- Unable to protect head → think arrhythmia or seizure
- Did the person ease him/herself down → Usually not arrhythmia
- Palpitations → think arrhythmia/cardiac
- Medication review
- Check orthostatic BP and HR
- 12-lead ECG
- Focused labs and testing
Vaso-vagal syncope
- Vasovagal (reflex) syncope, which portends a more benign clinical course, generally is manifested with an inciting factor or event (eg, dehydration, sight of blood, post–bowel movement) and preceding symptoms (eg, nausea, diaphoresis).1
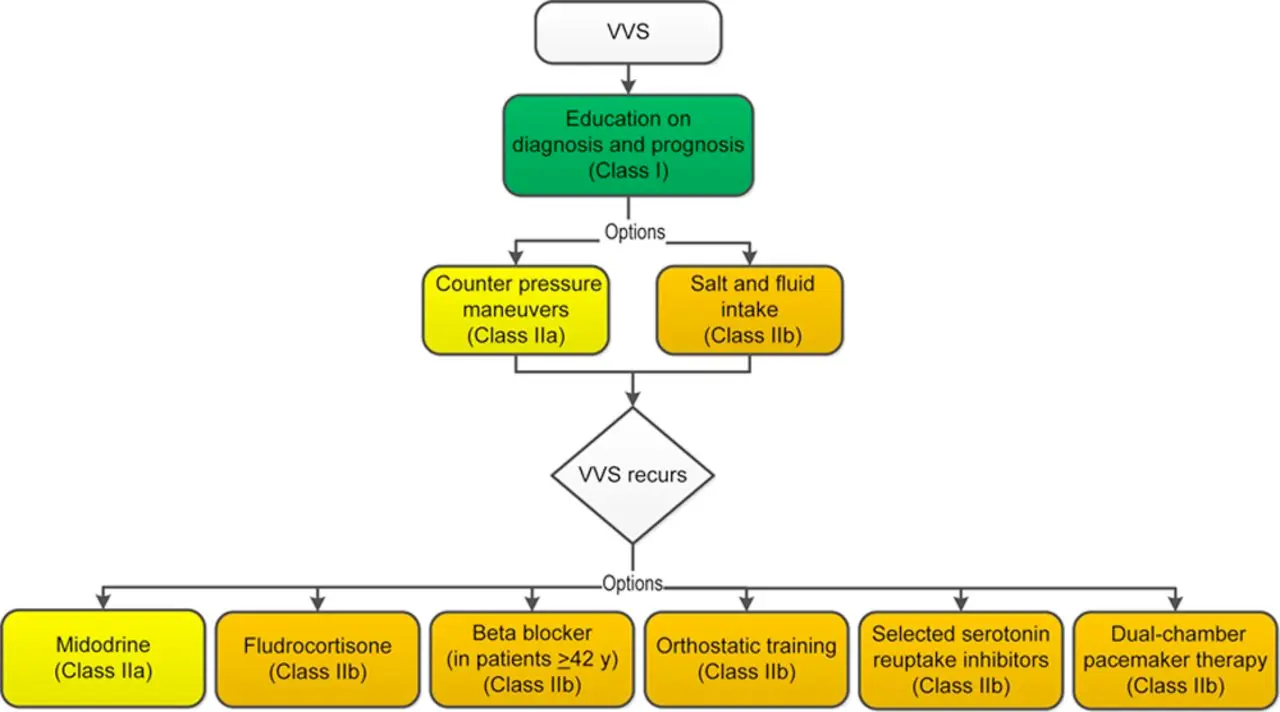
- Reassurance
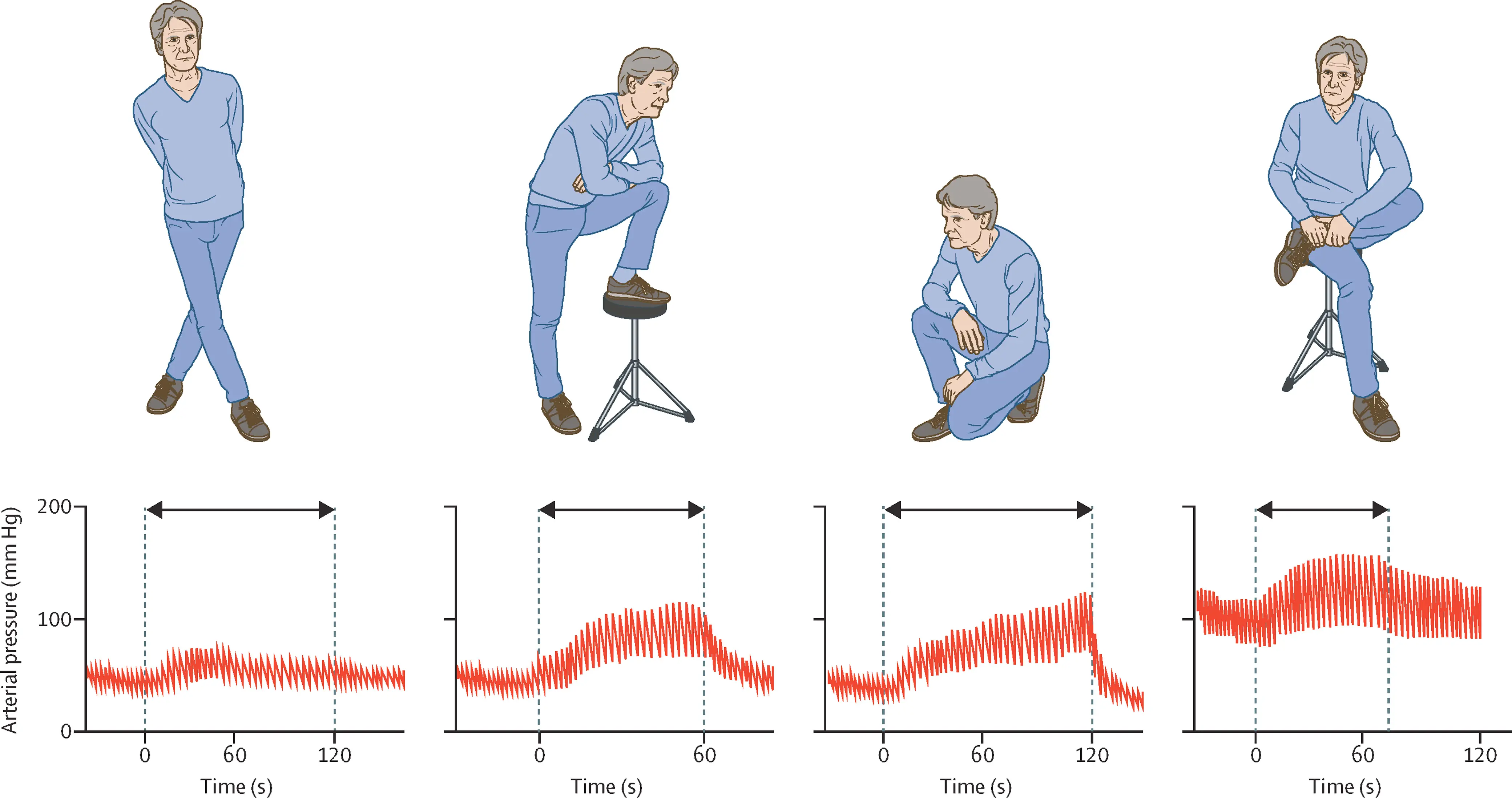
- Counter-pressure maneuvers, e.g. leg crossing, limb and/or abdominal contraction, squatting
- Liberalize salt (at least 5 g)
- Liberalize fluid (80 -100 oz or 2.5 — 3 L)
- Can consider fludrocortisone if unable to take in enough salt and fluid
- If recurrence
- Midodrine (if no HTN or CHF)
- BBs (if ≥ 42 years old)
Cardiac Syncope
- Cardiogenic or arrhythmogenic syncope comes on suddenly and without warning and may be associated with exertion.
- Evaluation
- ECG
- Ambulatory ECG Monitoring
- Echo: looking for depressed LVEF, ICM, HCM
- 📝 Do a Stress Echo if there is exertion-related syncope or suspect a relation to catecholamine surge
- EP study
- Class I indications include unexplained syncope + ICM, unexplained syncope + structural heart disease, NSVT + prior MI w/ EF ≤ 40%
Footnotes
-
Tseng AS, Kowlgi GN, DeSimone CV. Management of Premature Ventricular Complexes in the Outpatient Setting. Mayo Clin Proc. 2023 Jul;98(7):1042-1053. doi: 10.1016/j.mayocp.2023.01.021. PMID: 37419573. ↩