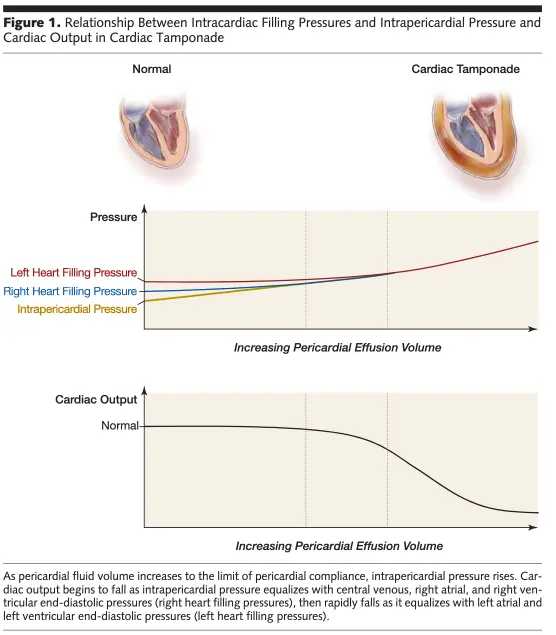
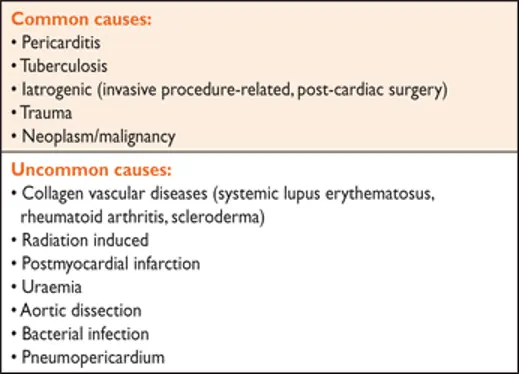
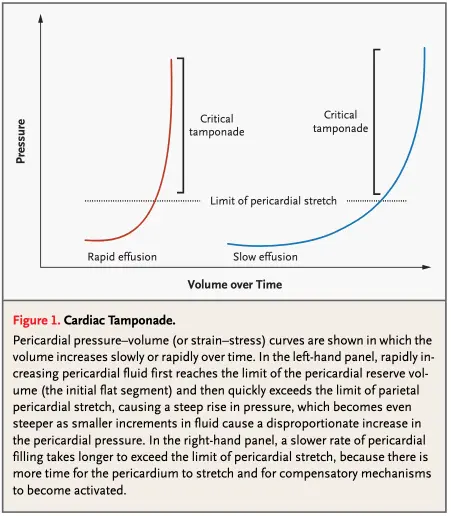
Cardiac tamponade is a life-threatening, slow or rapid compression of the heart due to the pericardial accumulation of fluid, pus, blood, clots or gas as a result of inflammation, trauma, rupture of the heart or aortic dissection.
- Cardiac Tamponade is a clinical diagnosis, so assessing for pulsus paradoxus at bedside is very useful.
- H&P
- Clinical signs in a patient with cardiac tamponade include tachycardia, hypotension, pulsus paradoxus, raised jugular venous pressure, muffled heart sounds
- ECG:
- low-voltage
- electrical alternans
- May show signs of pericarditis
- Chest imaging (e.g., CXR) with enlarged cardiac silhouette
- Classic signs include Beck’s triad
- neck vein distension with elevated JVP,
- pulsus paradoxus,
- diminished heart sounds
- Pericardial friction rub can be heard if concomitant pericarditis
- Fun fact: cath will show equilibration of average diastolic pressure and characteristic respiratory reciprocation of cardiac pressures, i.e. an inspiratory increase on the right and a concomitant decrease on the left---the proximate cause of pulsus paradoxus.
- Except in low-pressure tamponade, diastolic pressures throughout the heart are usually in the range of 15-30 mmHg.
- Rate of accumulation is more important than the size of the effusion
- Figure source: 1
Diagnosis
Clinical Exam
- Elevated JVP that does NOT change with respiration (- Kussmaul’s sign) may be seen. This is because of equalization of diastolic pressures with tamponade (“the pericardial pressure takes over everything in tamponade”)
- Recall, Kussmaul’s sign is where the JVP increases with respiration
Pulsus Paradoxus at Bedside
- Inflate BP cuff until you can’t hear Korotkoff sounds
- Start deflating until you hear sounds intermittently (sounds disappear with inspiration). Record the systolic pressure at which Korotkoff sounds are first audible -
- sounds are initially intermittent and respirophasic, becoming audible with expiration and inaudible with inspiration
- Keep deflating until you hear sounds continuously (during inspiration and expiration) -
- Pulsus paradoxus cutoffs:
- >10 mmHg → sens 98%, spec 70%, +LR 3.3, -LR 0.03
- >12 mmHg → sens 98%, spec 83%, +LR 5.9, -LR 0.03
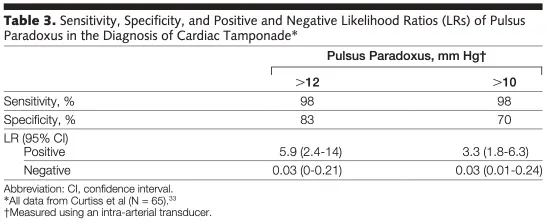
- “Most textbooks define a greater than 10-mm Hg difference between the initial detection of sounds on expiration and the constant presence of sounds with each heartbeat through the respiratory cycle as a “pulsus paradoxus.” Some experts suggest that the absolute value of pulsus paradoxus should be interpreted as a percentage of the pulse pressure or as a percentage of the expiratory systolic pressure.” 2
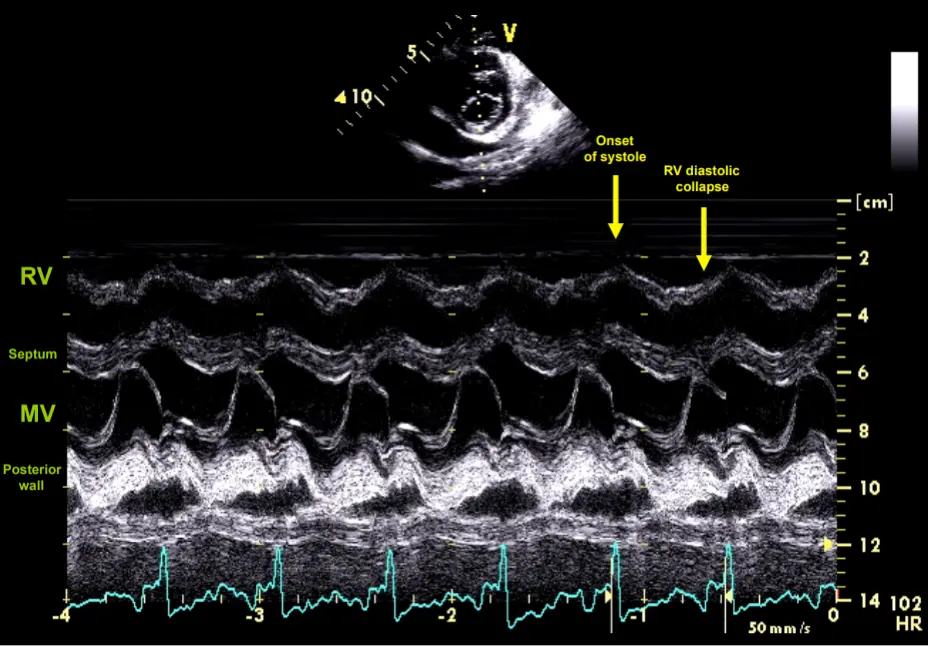
Echo in Cardiac Tamponade
- Echo is the single most useful diagnostic tool to identify pericardial effusion and estimate its size, location and degree of hemodynamic impact
- Other findings not listed below include:
- Abnormal ventricular septal motion
- Inspiratory decrease and expiratory increase in pulmonary vein diastolic forward flow
- Respiratory variation in ventricular chamber size
- Aortic outflow velocity (echocardiographic pulsus paradoxus)
Early Echo Findings
- IVC dilated, not collapsing (“plethora”)
- If IVC isn’t dilated, you may want to question Dx of cardiac tamponade
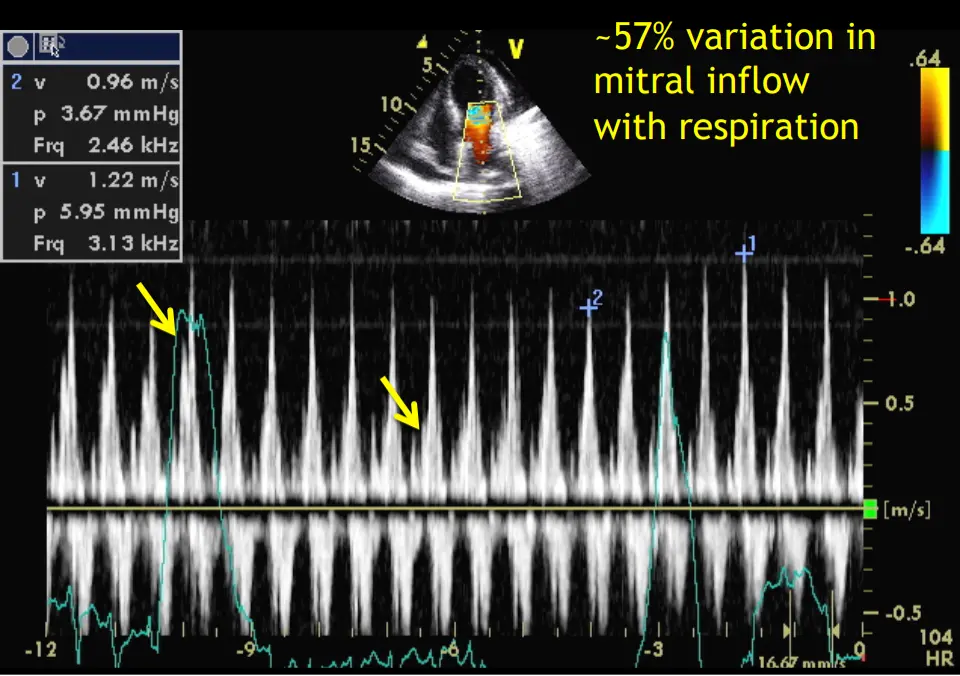
- Increased respiratory variation in mitral (> 25%) and tricuspid (> 40%) mitral inflow velocities
- ⚠️ ASE guideline documents have used mitral >30% and tricuspid >60% as well.
- Using the measured peaks (➕1 and ➕2), the variation is 21%, . The peaks as designated by the arrows in Dr. Shah’s talk are probably the peaks you should be using, which gives your 57% variation, i.e. concerning for tamponade
Late Echo Findings
- Early diastolic collapse of RV
- Late diastolic collapse of RA
Very Late Echo Findings
- LA and/or LV collapse
Waveforms
-
Can also see equalization of mean RA, RV, and PA diastolic pressures and mean PCWP
-
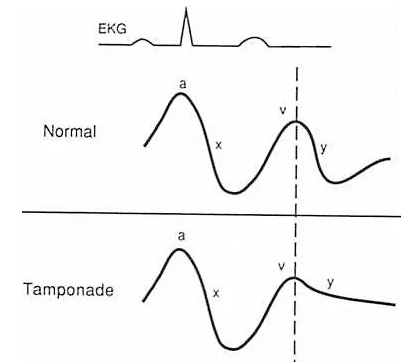
Recall, normal RA waveform tracings
- V wave: Passive filling of the RA during RV systole
- Y descent: TV opens, passive RA emptying
- A wave: RA contraction
- X descent: RA relaxation
-
In tamponade you will see a blunted Y descent
- Passive emptying of RA is dependent on pressure difference between RA and RV: in tamponade, the pericardial pressure takes over all other diastolic pressures (∴, loss of Y descent)
- Occurs d/t diastolic equalization of pressures in the RA and RV + lack of effective flow across the TV in early ventricular diastole
Footnotes
-
Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003 Aug 14;349(7):684-90. doi: 10.1056/NEJMra022643. PMID: 12917306. ↩
-
Roy CL, Minor MA, Brookhart MA, Choudhry NK. Does this patient with a pericardial effusion have cardiac tamponade? JAMA. 2007 Apr 25;297(16):1810-8. doi: 10.1001/jama.297.16.1810. PMID: 17456823. ↩