- Clinical definition
- frequent symptoms that occur with standing
- e.g. lightheadedness, palpitations, tremulousness, generalized weakness, blurred vision, exercise intolerance, and fatigue
- chronic (≥3 months, some say ≥6 months)
- often with standing HRs >120 bpm 1
- ↑ in HR of ≥30 bpm when going from lying to standing or upright tilt (or ≥40 bpm in those 12 to 19 years of age)
- 📝 the tachycardia of POTS is a sinus tachycardia 1
- absence of orthostatic hypotension
- frequent symptoms that occur with standing
- Typical demographic is young women (mean age 30.2 ± 10.3 years, 86% women), with an average HR increment of 44.2 ± 13.2 beats/min from supine to upright in the absence of provocative medications such as nitroglycerin or isoproterenol. 1
- Frequently preceded by symptoms of a viral illness (in 42%) or may occur post-operatively (in 9.5%) 1
Phenotypes
Work-up
-1747924821963.webp)
- All patients
- H&P
- Orthostatic vital signs
- 12-lead ECG
- CBC, TSH
- Selected patients (based on history)
- Ambulatory ECG Monitoring
- Autonomic testing
- Echo
- The cardiologist who first evaluates a patient for POTS must also exclude structural cardiac disease that would reduce upright stroke volume, including valvular heart disease, cardiac tumors or other causes of right or left ventricular outflow tract obstruction, pulmonary hypertension, undiagnosed congenital heart disease, or acquired myocardial diseases.1
- Tilt Table test
- Exercise ECG
Management
-1747924875426.webp)
Non-pharmacologic management
-1747924958671.webp)
- Diet
- Small, frequent meals are recommended, and a high-fiber diet can help normalize GI symptoms.1
- Large meals should be avoided, especially those high in fat and complex carbohydrates, because these can lead to postprandial aggravation of symptoms due to increased blood flow to the gut.
- ↑ salt intake
- 2 showed that “high dietary sodium intake compared with low dietary sodium intake increases plasma volume, lowers standing plasma norepinephrine, and decreases change in HR.”
-1747923540124.webp)
- Small, frequent meals are recommended, and a high-fiber diet can help normalize GI symptoms.1
- Non-upright aerobic exercise - at least 30 mins 4x/wk
- e.g. rowing machine, recumbent bike, swimming
- physical reconditioning with a short-term (3 month) progressive exercise training program leads to improvement or remission of POTS in the majority of patients 1
- Compression garments and/or Abdominal binders1
- helps with hemodynamically significant venous pooling from gravitational gradients in the upright position
- to be of any benefit, they must extend at least to the top of the thighs and preferably to the abdomen.
- Abdominal binders can decrease splanchnic–mesenteric venous pooling and may be easier to use, particularly in combination with thigh-high compression stockings.
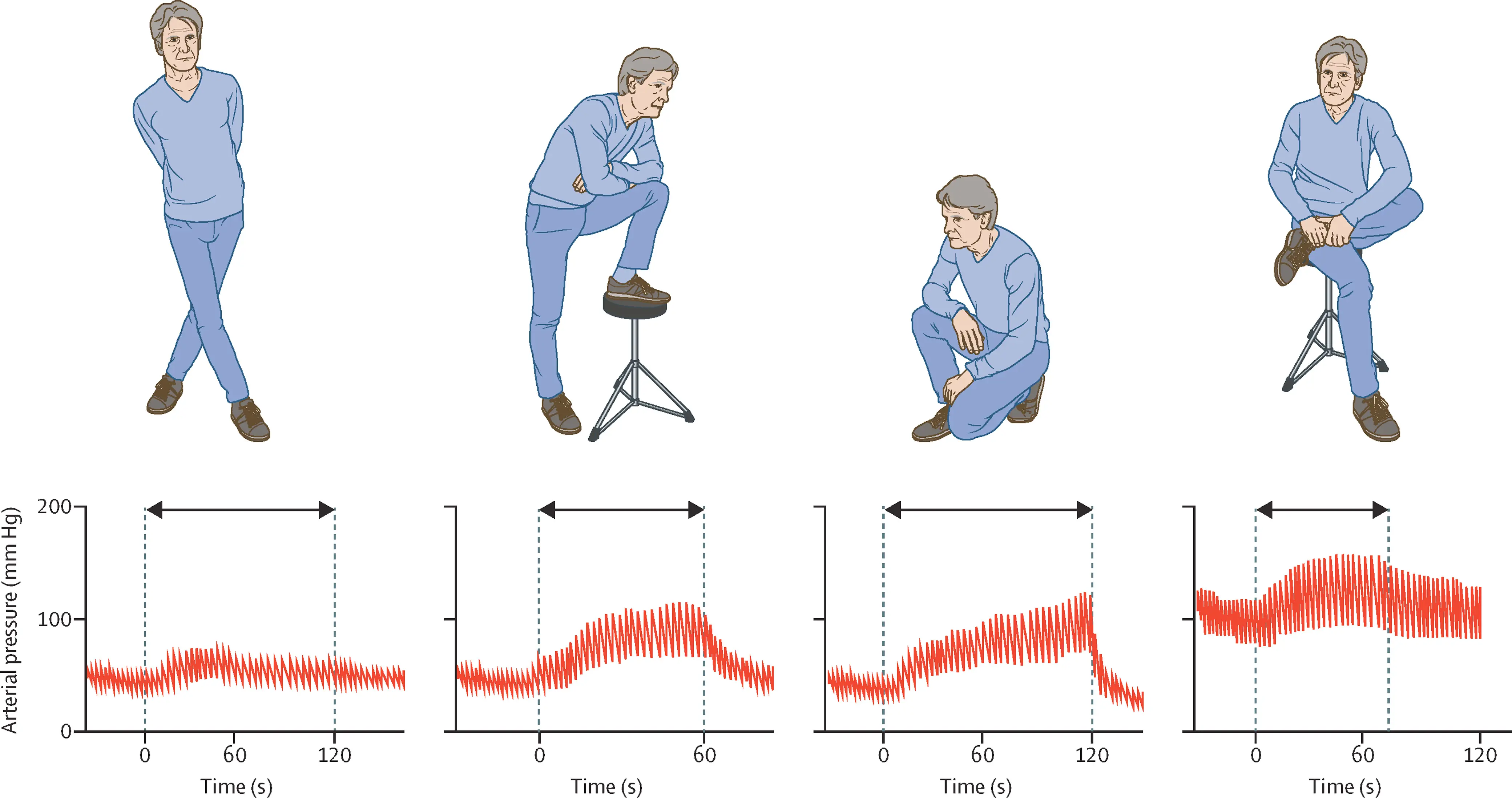
- Counter maneuvers at the onset of prodromal symptoms in those with VVS
- Avoid triggers
- Environmental heat, prolonged upright posture, prolonged fasting, excessive alcohol intake, straining (such as during urination or bowel movements), or vasodilatory medications will exacerbate orthostatic intolerance and should be avoided when possible.1
Pharmacologic management
- ⚠️ Due to potential side effects and absence of clinical trials supporting efficacy, medications should be avoided in POTS if possible. Medications can be considered in patients with severe symptoms who are having difficulty initiating an exercise program as a bridge to help minimize some symptoms and allow them to initiate the exercise program.1
- No medication is Food and Drug Administration approved to treat POTS; all use is off-label
- Drugs
- Midodrine (2b)
- 2.5 to 10 mg 3 times daily in a front-loaded regimen can be tried in patients with low or low-normal BP at rest
- first dose should be given 15-30 min before getting out of bed in the morning. The last dose should not be taken later than 4 pm because supine hypertension is a major potential side effect of vasoactive medications such as midodrine (though more frequently seen in patients with autonomic failure).
- Patients should take care not to lie flat for several hours after using the drug.
- Other reported adverse or bothersome side effects include urinary retention, scalp tingling, and piloerection (“goose bumps”).
- These are direct effects of the drug and should be expected.
- Fludrocortisone (2b)
- starting at 0.1 mg daily and increasing up to 0.2 mg daily can be used to ↑ blood volume
- In order to be maximally effective, this medication should be taken with a high salt diet, and is best taken at night.
- ⚠️ hypOkalemia potential
- should increase potassium intake because hypokalemia is a potential medication side effect, and potassium must be checked after initiation because hypokalemia can be profound
- ⚠️ Prolonged use should be avoided because of concern for development of myocardial fibrosis from chronic elevation in aldosterone activity.
- Pyridostigmine (2b)
- 30 to 60 mg 3 times a day can increase parasympathetic autonomic tone
- Potential side effects include abdominal cramping, diarrhea, and muscle cramps, which can be limiting in some patients but might be a beneficial effect in others, particularly those with constipation.
- Propranolol (2b), especially if hyperadrenergic POTS
- starting at 10 mg and increasing to 60 mg may be used to limit the HR increment and reduce symptoms
- Atenolol 25 mg or metoprolol 25 mg daily are alternatives for patients with a history of bronchospasm, although nonselective beta-blockers are preferable because they additionally block epinephrine-mediated β-2-vasodilation.
- Clonidine
- 0.1 mg twice daily can be used to reduce autonomic instability in pts with hyperadrenergic POTS or significant hypertensive responses during tilt
- alpha-methyldopa
- Ivabradine
- reduces intrinsic HR by specifically blocking the cardiac “funny” channel, the I
fcurrent that controls the pacemaker activity of the sinus node -1747923856707.webp)
- reduces intrinsic HR by specifically blocking the cardiac “funny” channel, the I
- Midodrine (2b)
Footnotes
-
Bryarly M, Phillips LT, Fu Q, Vernino S, Levine BD. Postural Orthostatic Tachycardia Syndrome: JACC Focus Seminar. J Am Coll Cardiol. 2019 Mar 19;73(10):1207-1228. doi: 10.1016/j.jacc.2018.11.059. PMID: 30871704. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9 ↩10 ↩11
-
Garland EM, Gamboa A, Nwazue VC, Celedonio JE, Paranjape SY, Black BK, Okamoto LE, Shibao CA, Biaggioni I, Robertson D, Diedrich A, Dupont WD, Raj SR. Effect of High Dietary Sodium Intake in Patients With Postural Tachycardia Syndrome. J Am Coll Cardiol. 2021 May 4;77(17):2174-2184. doi: 10.1016/j.jacc.2021.03.005. PMID: 33926653; PMCID: PMC8103825. ↩