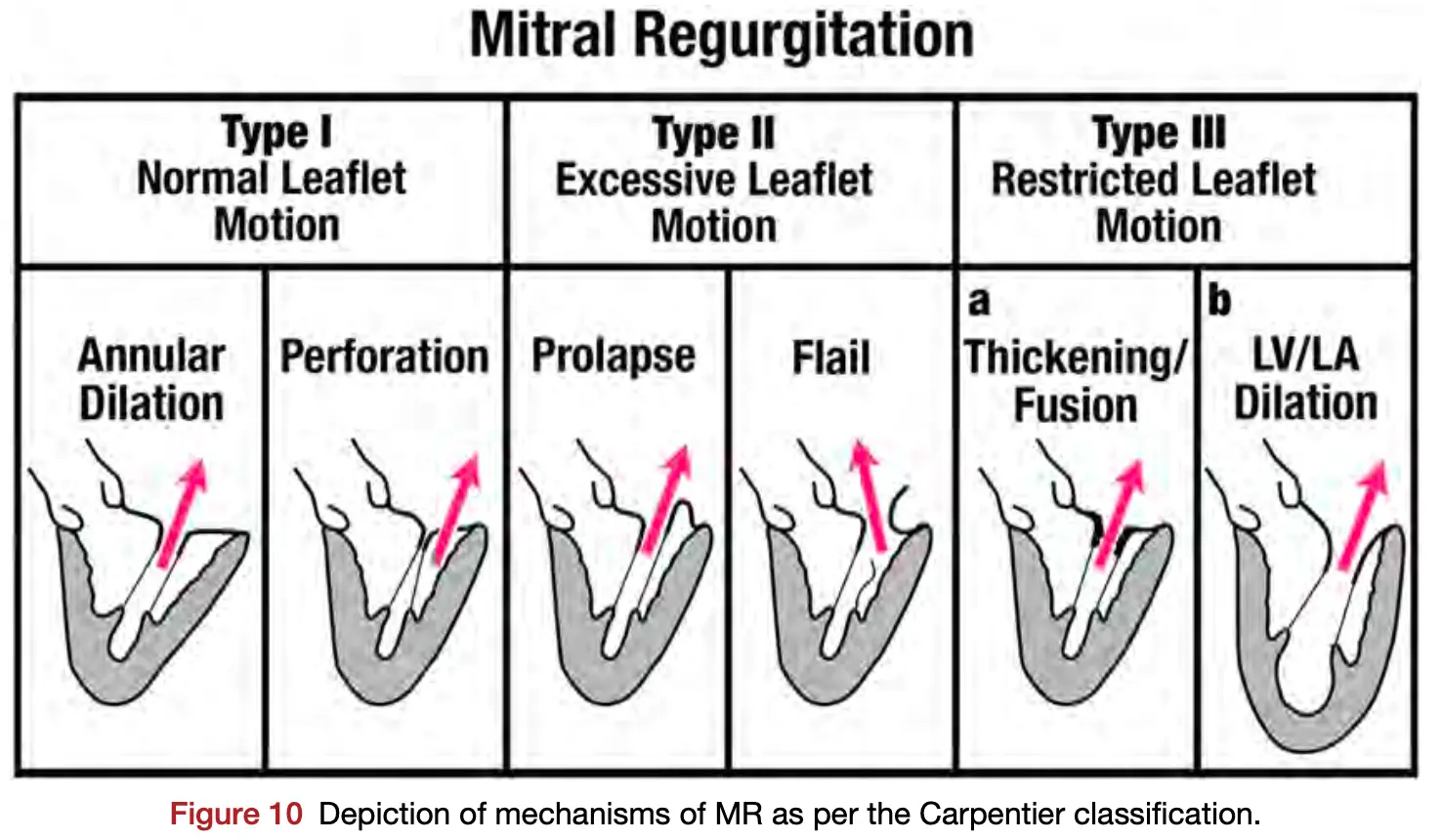
- It is useful to consider whether leaflet motion is intrinsically normal or abnormal according to the Carpentier classification:
- Type I leaflet motion is normal but can be associated with MR if there is annular dilation (secondary MR) or a leaflet perforation.
- Type II leaflet motion is excessive and is most commonly due to MVP or flail leaflet.
- Type III leaflet motion is restrictive, commonly seen in the presence of LV dilation (secondary MR) or rheumatic MV disease or other post-inflammatory conditions such as collagen vascular disease, radiation injury, carcinoid syndrome, or drug-induced inflammatory changes.
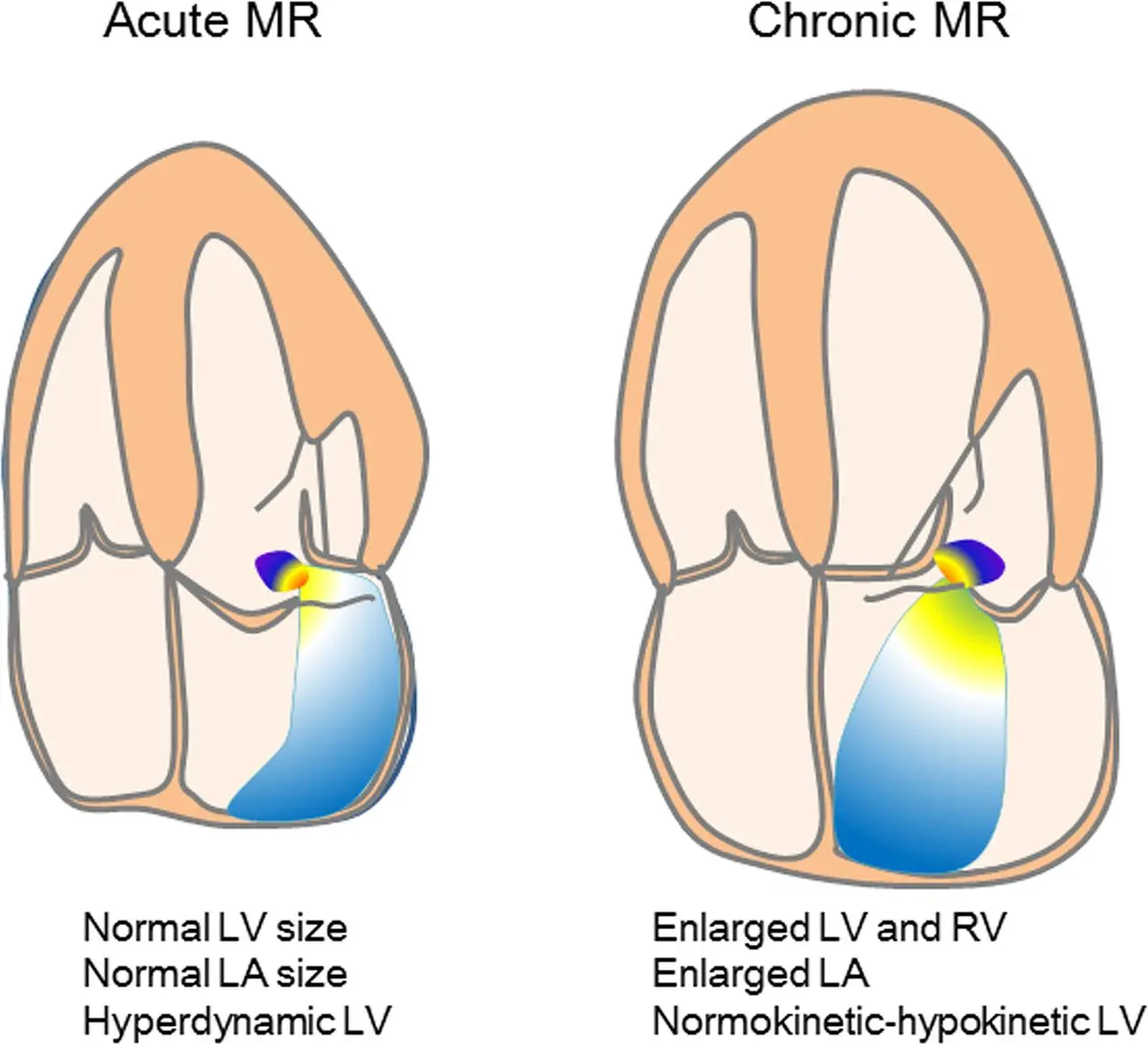
Acute MR
-
Acute MR is far less common than chronic MR and usually results in hemodynamic compromise.
-
It occurs most commonly due to ruptured papillary muscle after acute myocardial infarction, ruptured chordae tendinae resulting in a flail leaflet, or leaflet destruction due to endocarditis and less frequently due to rapid onset of cardiomyopathy (e.g., Takotsubo, myocarditis, or postpartum cardiomyopathy).
-
Patients often present with pulmonary edema from elevated LA pressure, tachycardia, and severe hypotension from loss of forward SV.
-
The combination of hypotension and high LA pressure results in a low driving pressure and therefore lower MR jet velocity across the MV. ==Accordingly, color Doppler imaging often will NOT show a large turbulent flow disturbance, and thus MR may be underestimated or not appreciated at all.== The color Doppler jet is usually markedly eccentric, which again can underestimate MR severity.
-
==Anatomic imaging of flail leaflet or ruptured papillary muscle and the finding of a hyperdynamic LV with low Doppler systemic output along with clinical findings should be enough to substantiate the diagnosis, even if color Doppler does not show a large MR jet.== Systolic flow reversal in the pulmonary veins is usually present and is helpful. TEE may be better at identifying acute severe MR.
-
Common causes include:
- Endocarditis
- Papillary muscle rupture or chordal muscle rupture, e.g. after recent MI or infarction
- Can result in flail leaflet
-
Sudden ↑ in LA and LV volume in the absence of compensatory LV or atrial dilation.
-
Management
- Urgent surgery
Post-MI Mitral Regurgitation
Papillary muscle rupture
- Complicates 1-5% of acute Medications
- Usually 2-7 days after the acute ischemic event; typically first MI
- Posteromedial papillary muscle more commonly ruptured (10x more likely) due to have single blood supply (posterior descending artery)
- The anterolateral papillary muscle has dual blood supply
- ⚠️ Exam may not have feature a hyperdynamic precordium or audible murmur
- d/t rapid and complete equalization of pressure between the LV and LA.
- By contrast, ventricular septal rupture would present similarly, but you’ll hear a loud murmur.
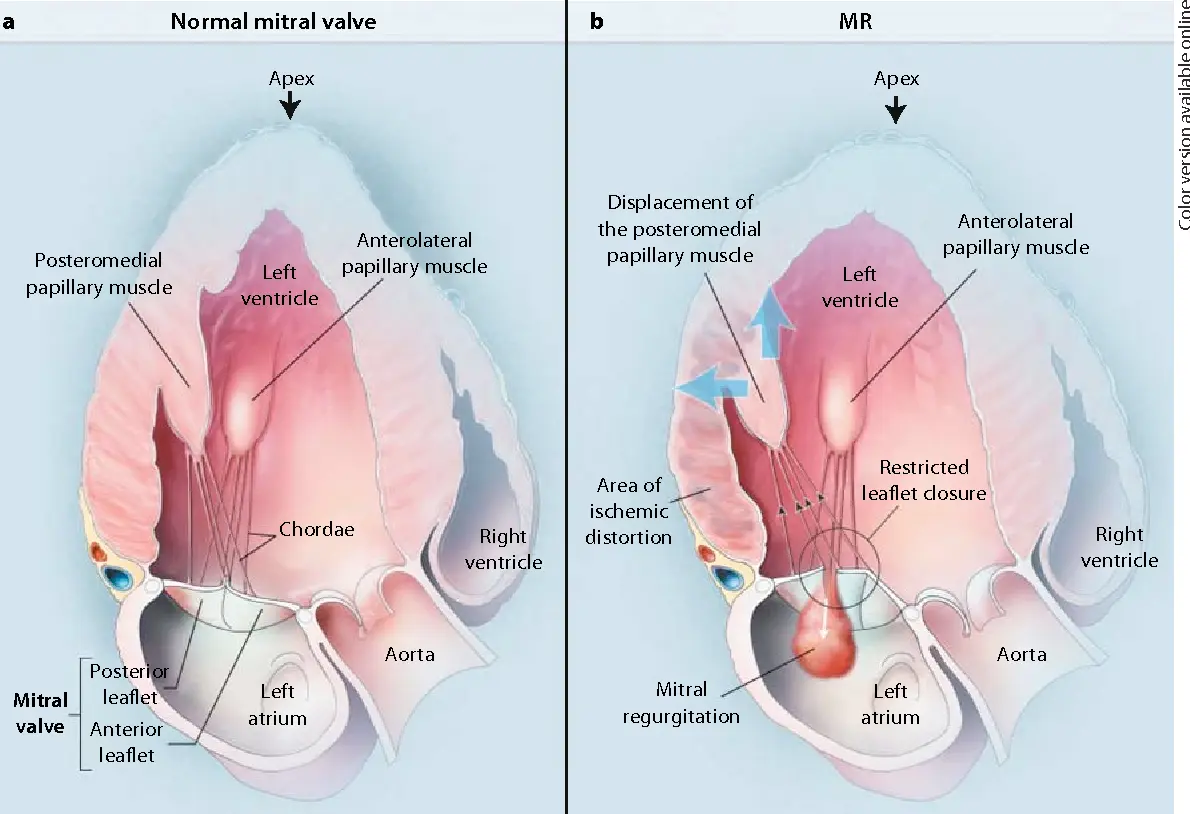
Ischemic Mitral Regurgitation
Chronic Mitral Regurgitation
- “If you see MR, you need to ask why?”
- “A comprehensive evaluation of valvular regurgitation should include identifying the mechanism and the severity of valvular regurgitation, along with adaptation of the heart to the volume overload.”
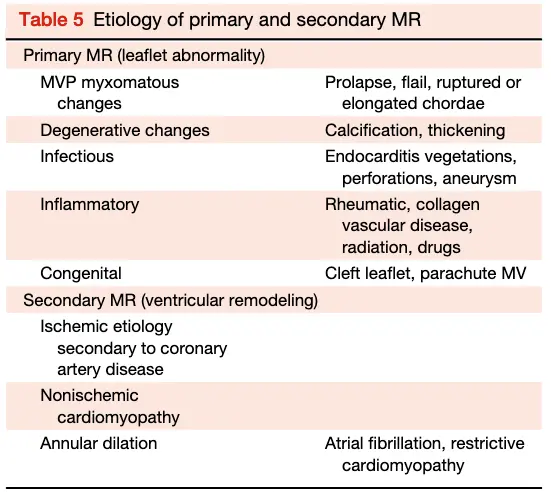
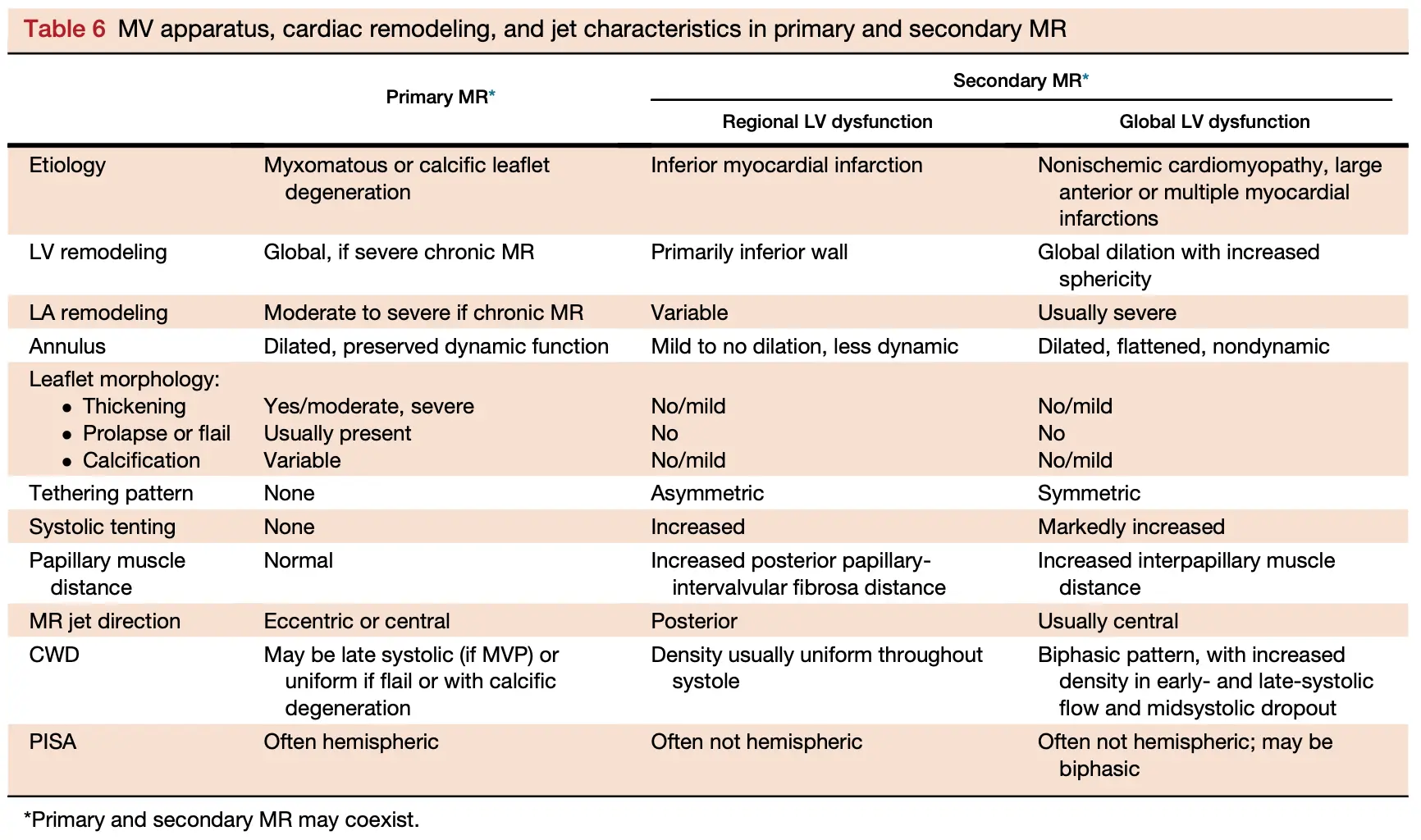
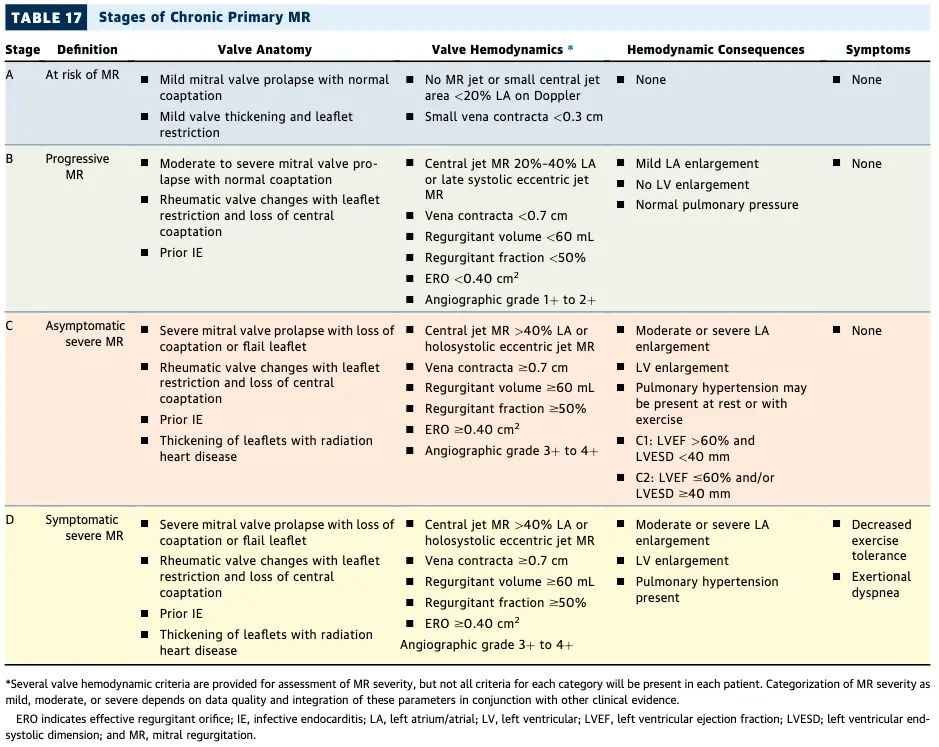
- In primary MR, an intrinsic abnormality of the MV apparatus (including the leaflets, chords, and/or papillary muscles) causes the MR, whereas secondary MR results from distortion of the MV apparatus due to LV and/or LA remodeling.
- It is important to distinguish primary from secondary MR as therapeutic approaches and outcomes differ.
- Most secondary MR is a disease of the LV.
- Results in LV volume overload → ventricular (and atrial) remodeling w/ eccentric hypertrophy, i.e. LV dilation w/o increased wall thickness.
- Can be tolerated for several years. Only after several years (typically), may it lead to ↓ contractility and systolic dysfunction → ↑ pulmonary venous pressure, ↓ SV and ↓ CO.
- ↑ LAP: pulmonary congestion, pulmonary hypertension, and atrial fibrillation
- LA dilation
- LA dilation is an expected consequence of severe MR. A normal LA size generally excludes severe chronic MR. LA volumes are superior to LA diameters in evaluating LA dilation and in predicting outcomes and atrial fibrillation. However, LA dilatation can occur in many disease states including hypertension and AFib. ∴, a dilated LA does not necessarily imply severe MR.
Table 5 Etiology of primary and secondary MR
| Primary MR (leaflet abnormality) | Primary MR (leaflet abnormality) |
|---|---|
| MVP myxomatous changes | Prolapse, flail, ruptured or elongated chordae |
| Degenerative changes | Calcification, thickening |
| Infectious | Endocarditis vegetations, perforations, aneurysm |
| Inflammatory | Rheumatic, collagen vascular disease, radiation, drugs |
| Congenital | Cleft leaflet, parachute MV |
| Secondary MR (ventricular remodeling) | Secondary MR (ventricular remodeling) |
| Ischemic etiology secondary to coronary artery disease | Ischemic etiology secondary to coronary artery disease |
| Nonischemic cardiomyopathy | |
| Annular dilation | Atrial fibrillation, restrictive cardiomyopathy |
4, 5, 6, 7 of Severe MR
EROA ≥ 0.4 cm2 Regurgitant fraction ≥ 50% Regurgitant volume ≥ 60 mL Vena contracta ≥ 0.7 cm
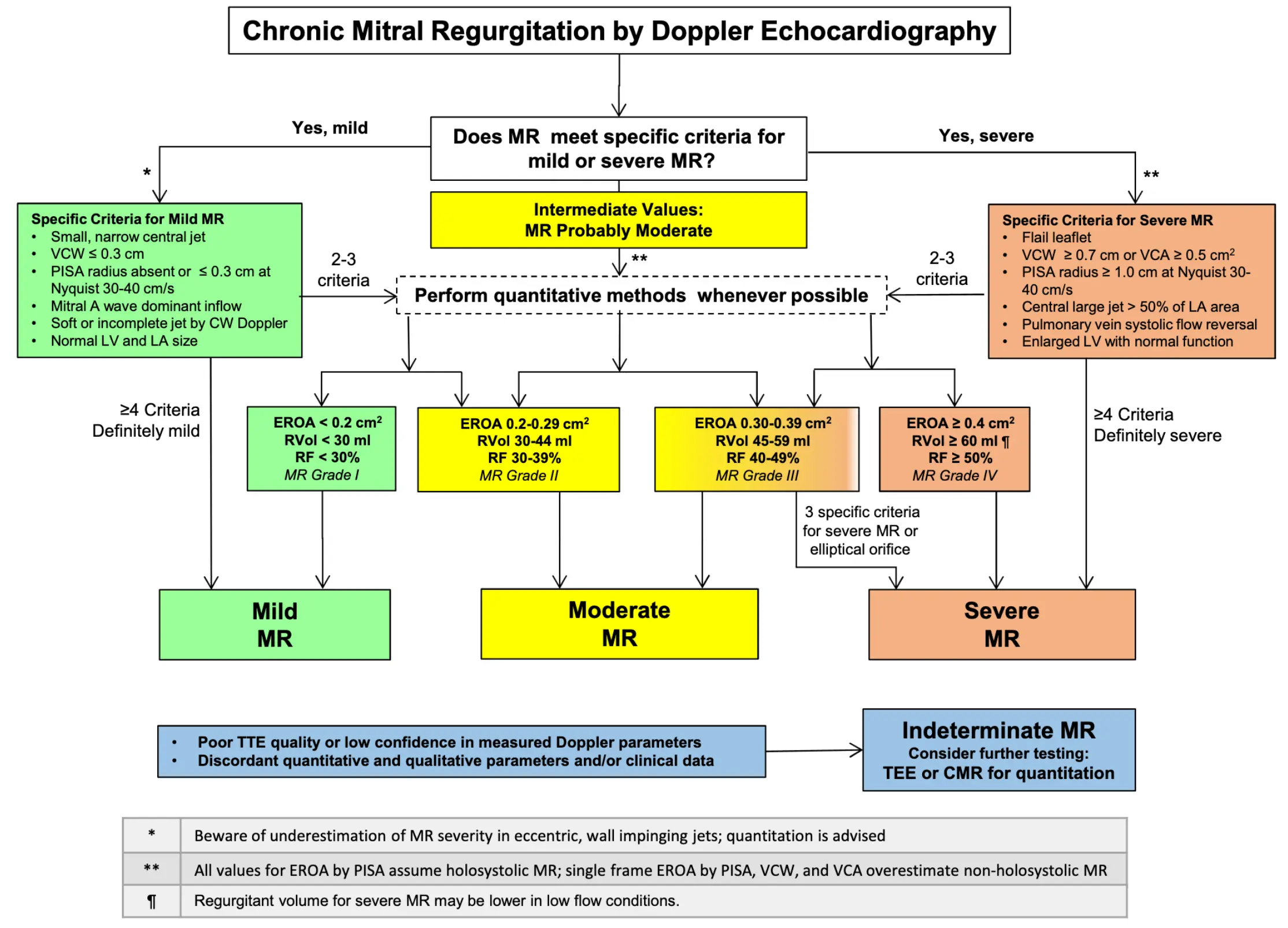 Source: Figure 18 of 2017 ASE Valvular Guidelines
Source: Figure 18 of 2017 ASE Valvular Guidelines
- Primary or Secondary (functional) MR?
- differentiates 1˚ lesions of the mitral leaflets and subvalvular apparatus from 2˚ dysfunction d/t annular or LV dilatation/remodeling and/or dysfunction.
- The most common cause of primary MR is myxomatous degeneration, most frequently MVP.
- Most common causes of MR: Secondary MR is the most prevalent form of MR, followed by Mitral Valve Prolapse (MVP), ischemic MR.
- Primary MR includes:
- myxomatous ∆, notably Mitral Valve Prolapse (MVP)
- Mitral Annular Calcification (MAC)
- Rheumatic Heart Disease
- Connective Tissue Disease
- radiation therapy ☢️
- adverse effects of medications 💊
- Echo
- Don’t forget to provide information regarding the associated conditions or sequelae of MR, such as pulmonary hypertension, tricuspid regurgitation, LA dilation, and ventricular dilation or systolic dysfunction
- ⚠️ In the presence of severe primary or secondary MR, use of LVEF may overestimate systolic function because of the lower impedance of the LA chamber.
- Be sure to check LVESD
- TEE can also be helpful given its ↑ spatial resolution and the proximity of the probe to the MV.
- MV surgical views are 🔥
- Echo Doppler
- vena contracta width, ERO, spatial distribution of MR jet w/in the LA, flow convergence
- Screening
- After the initial echocardiographic evaluation, repeat echocardiography is indicated for patients with moderate or greater MR, even in the absence of symptoms
- Frequency
- Severe MR: every 6-12 months
- Moderate MR: every 1-2 years
- Mild MR: every 3-5 years
- ⚠️ Repeat echocardiography is also recommended for patients with any degree of MR and a change in clinical status or physical examination findings.
Primary Mitral Regurgitation
“Primary MR is a fancy way for saying prolapse.”
- David Skolnick, August 9, 2024
| Etiology | Affected Valve Level(s) |
|---|---|
| Degenerative (see MVP) | leaflets, chordae, annulus |
| Mitral Annular Calcification (MAC) | annulus, leaflets |
| CAD → ruptured papillary mm. | papillary mm. |
| Rheumatic Heart Disease | leaflets, chordae |
| Endocarditis | leaflets, chordae |
| Hypertrophic Cardiomyopathy | leaflets, chordae, papillary mm. |
| Connective Tissue Dz (RA, SLE, APLS) | leaflets, annulus |
| Radiation ☢️ | leaflets, chordae |
| Drugs (ergotamines, methysergide, pergolide, fenfen, dexfen) | leaflets, chordae |
- “A mechanical problem requires a mechanical solution”
- Primary MR is a mechanical problem of the leaflet coaptation that only has a mechanical solution, i.e. MV intervention
- A flail leaflet is part of the MVP spectrum and occurs when the leaflet edge, not just the leaflet body, is located in the LA with free motion. It occurs most commonly from rupture of the marginal chords. A flail leaflet almost always denotes severe MR and is clearly associated with adverse outcomes. An extreme of flail MV is papillary muscle rupture.
Secondary Mitral Regurgitation
- Secondary MR occurs in approximately 65% of cases reported with left ventricular dysfunction or remodeling as the predominant cause.
- The leaflets are intrinsically normal in secondary MR, although minor leaflet thickening and annular calcification can be present.

Echo
Regardless of etiology, if there is a small central jet, normal leaflet morphology, a VCW < 0.3 cm, no proximal flow convergence, and an A-wave dominant mitral inflow pattern, then MR is mild and further quantitation is not necessary. Conversely, if there is a large jet, with a prominent flow convergence, large VCW > 0.7 cm, flow reversal in the pulmonary veins, then MR is severe; quantitation would substantiate the severity of the regurgitation.
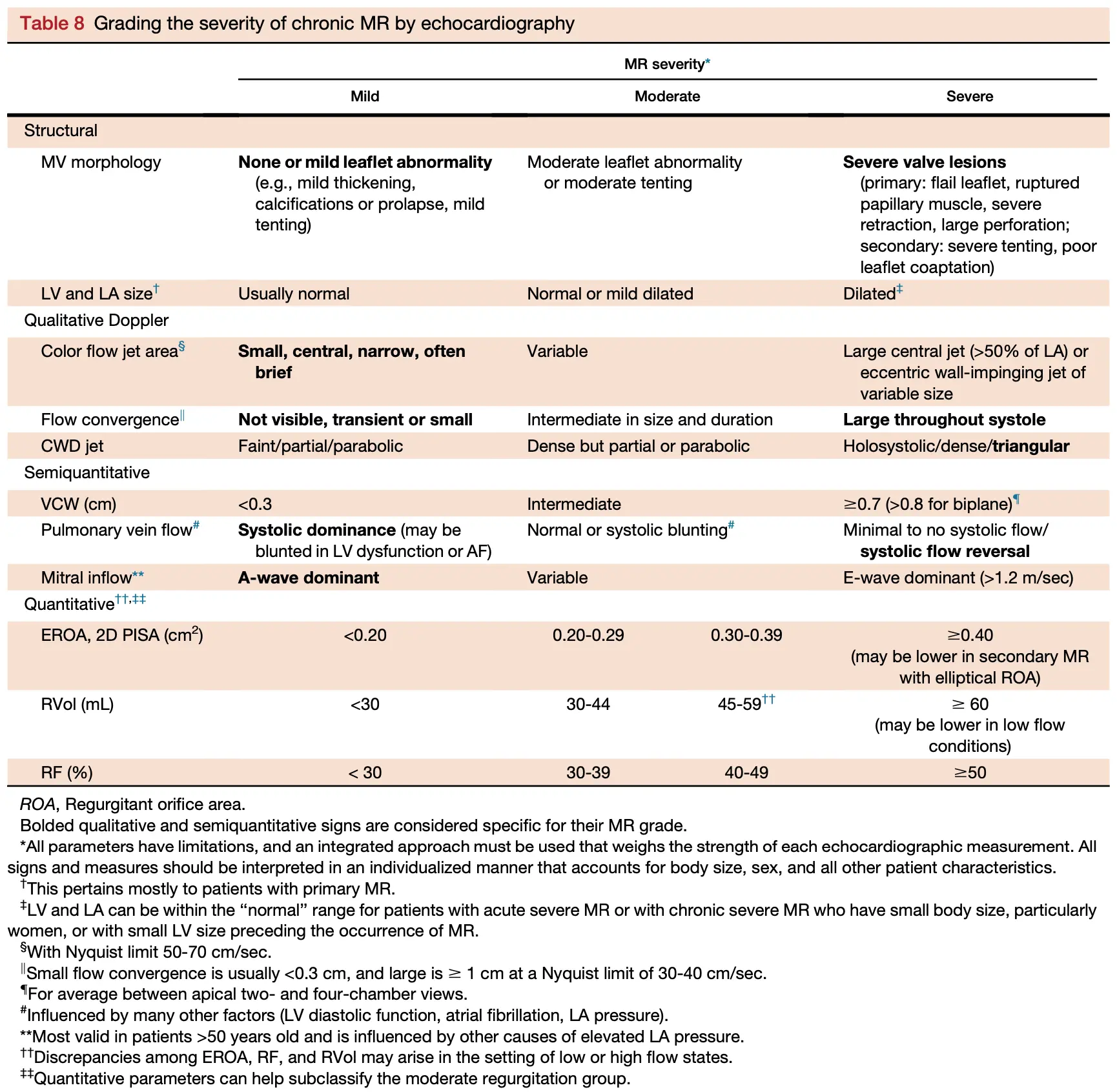
- Findings that are a slam dunk, i.e. unquestionably severe MR (bolded in Table above):
- Severe valve lesions on 2D or 3D imaging, e.g. flail leaflet, ruptured papillary muscle, severe leaflet retraction, or a large perforation
- A properly measured VCW ≥0.7 cm is specific for severe MR
- Systolic flow reversal in more than one pulmonary vein
- Findings are specific for nonsevere MR:
- failure to identify a proximal flow convergence region
- presence of an A-wave dominant mitral filling pattern
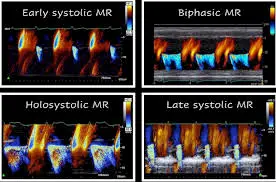
- late systolic MR (e.g. MVP) is rarely severe
- early systolic MR (e.g. ventricular dyssynchrony) is rarely severe
- biphasic MR is rarely severe (See non-holosystolic MR)
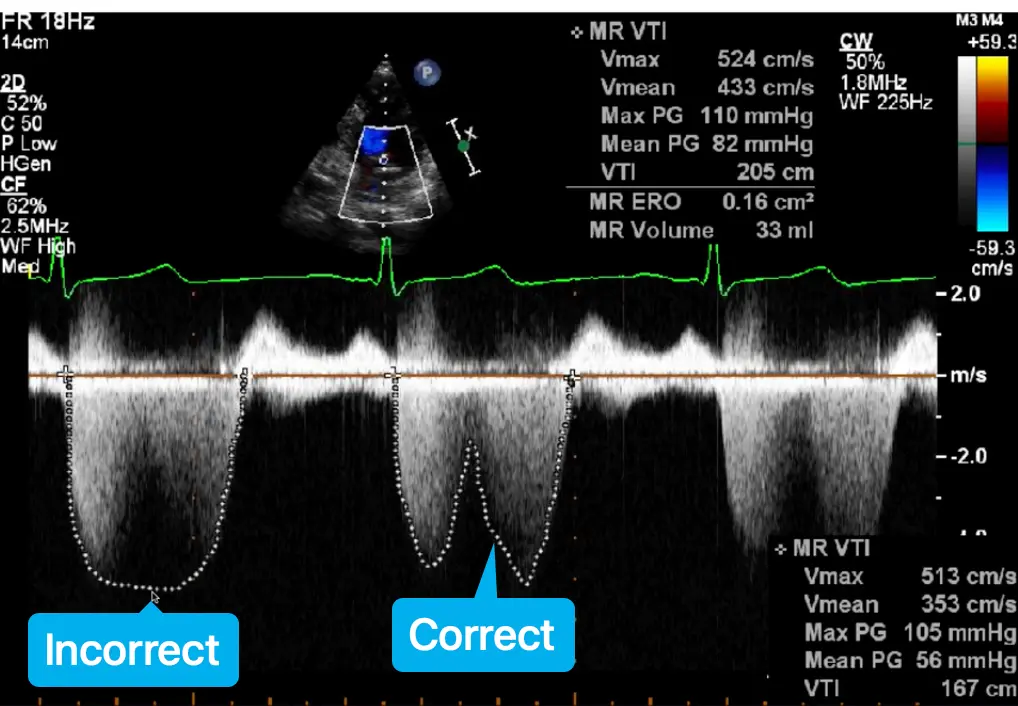
- Avoid overtracing the jet or turning up doppler gains to make the signal look holosystolic as this may overestimate the PISA
- Chronic severe MR almost always leads to dilated LV and LA, and thus normal chamber volumes are unusual with chronic severe MR.
- MR limited to late systole (MVP) or early systole (ventricular dyssynchrony) is usually not severe but may be misinterpreted as severe when based only on single-color frame measurements such as VC or PISA
EROA cutoffs for severe Primary vs Secondary MR
For primary MR, the cutoff for severe MR is ≥ 0.4 cm2. However, in cases of secondary MR, a lower cutoff of ≥0.3 cm2 may still be likely severe MR by 2D PISA because the regurgitant orifice is frequently semilunar or elliptical in 2˚ MR, affecting measurements of VCW and possibly leading to underestimating EROA by the 2D PISA method
MR quantification in MVP
⛔ Avoid using single frame measurements - PISA EROA and VCW - when the MR is not holosystolic, e.g. MVP with late systolic MR, functional MR with biphasic MR, LV dyssynchrony with early systolic MR, as they can overestimate MR severity.
When non-holosystolic, you should use regurgitant volume (RVol) method.
Color Doppler
- There are three methods of evaluating MR severity by color flow Doppler:
- regurgitant jet area
- VC
- flow convergence
Regurgitant jet area
- Although jet area is excellent for excluding MR, it is not reliable for grading MR severity, even when indexed for LA area.
- Patients with acute severe MR, in whom blood pressure is low and LA pressure is elevated, may have a small color flow jet area, whereas hypertensive patients with mild MR may have a large jet area.
- Jet area is dependent on the mechanism of MR.
- With flail leaflet, the MR jet is often very eccentric; jet area is small, underestimating MR severity as the jet spreads out along the wall and loses energy.
- In secondary MR, central jets with a slit-like orifice can appear large, particularly in the two-chamber view, along the line of MV coaptation, even when the EROA is small.
- ∴, MR grade should not be determined by ”eyeballing” 👀 the color flow area of the MR jet alone, without considering the origin of the jet (VC) and its flow convergence.
- A small noneccentric jet with a narrow VC (<0.3 cm) and no visible flow convergence region usually indicates mild MR.
- A large jet with a wide VC (≥ 0.7 cm) and where the jet wraps around the LA and penetrates into the pulmonary veins is almost always severe MR.
Vena Contracta
- Vena contracta (width and area). The VC is a measure of the effective regurgitant orifice.
- VC width
- For MR, the VC width (VCW) should be imaged preferably in a PLAX view (axial resolution) and measured using zoom mode at the narrowest portion of the jet as it emerges from the orifice.
- VC < 0.3 cm usually denotes mild MR
- VC ≥ 0.7 cm is specific for severe MR.
- Intermediate values overlap substantially between MR grades, so additional methods should be used for confirmation.
- VCW works equally well for central and eccentric jets, however, it is dependent on orifice geometry, underestimating MR severity if there are multiple jets or if there is a markedly elliptical (noncircular) orifice shape, as often seen in secondary MR.
Flow convergence (PISA)
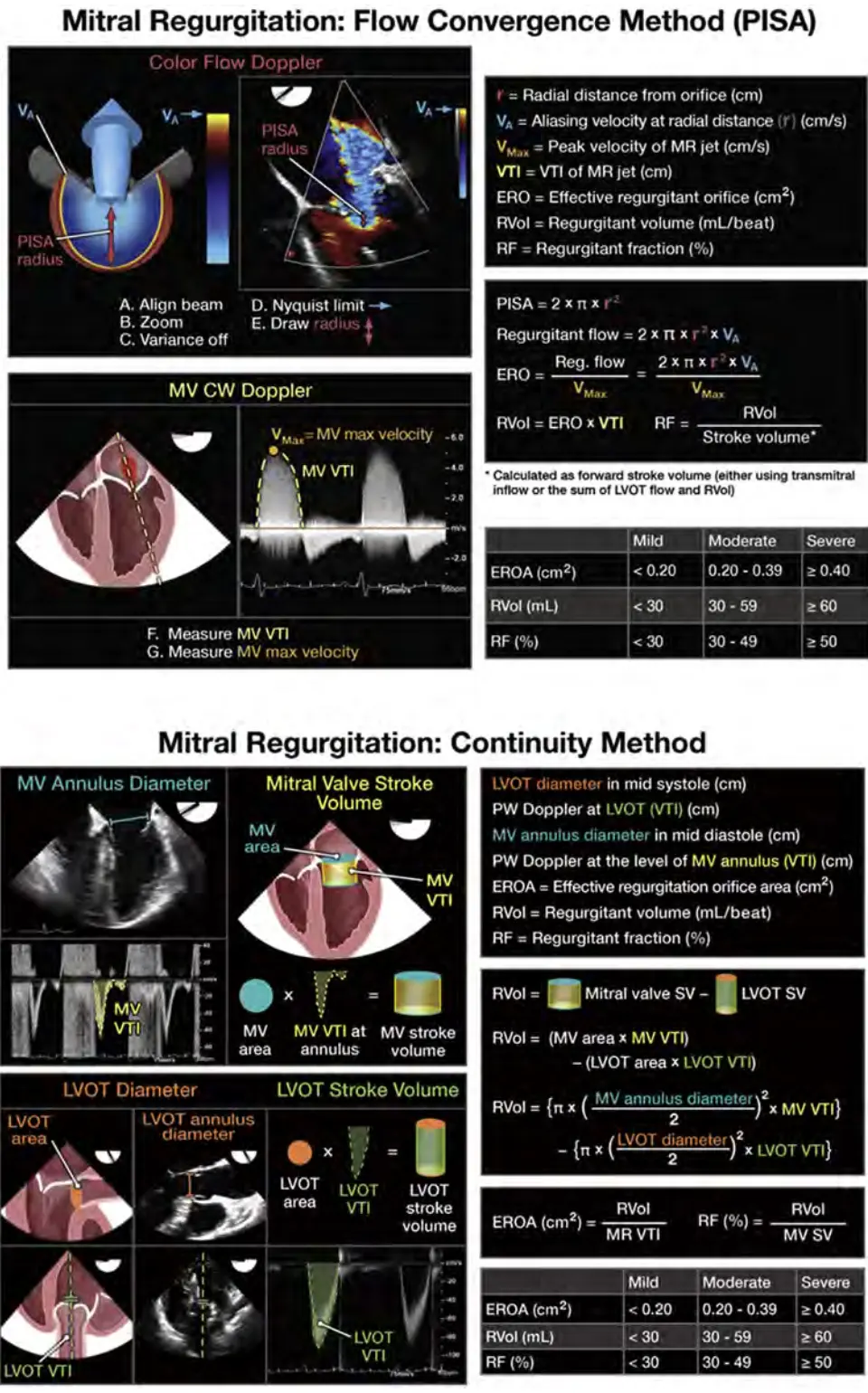 Figure source: 1
Figure source: 1
Recall from Echo Math:
- Interpretation (at least in primary MR):
- EROA ≥0.4 cm2 → severe MR
- 0.20-0.39 cm2 → moderate MR
- <0.20 cm2 → mild MR
- ⚠️ In MR, PISA is more accurate for central regurgitant jets than eccentric jets and for circular orifices than noncircular orifices.
- It is usually easy to identify the aliasing line of the hemisphere; however, it can be difficult to judge the exact location of the orifice. Optimization of acquisition and measurement of PISA are essential, as any error in radius is subsequently squared in the derivation of EROA.
- Errors of 10%-25% are common even among expert readers and are the smallest for central jets; therefore, PISA should always be considered in the context of the other echo/Doppler findings.
- The dynamic nature of the orifice in MR can also lead to errors with the PISA formula.
- The regurgitant orifice is often crescent shaped in secondary MR. In such cases, the assumption of circular orifice geometry inherent to 2D PISA may result in underestimation of secondary MR.
- This may partly explain the finding that lower values of EROA by 2D PISA are associated with worsened prognosis in secondary MR.
- Also, it should be remembered that PISA EROA, like VCW or VCA, is calculated from a single-frame image. These parameters therefore will overestimate MR severity when MR is not holosystolic.
Color M-mode
Continuous Wave Doppler
- In most patients, maximum MR velocity is 4-6 m/sec due to the high systolic pressure gradient between the LV and LA. The velocity itself does not provide useful information about the volumetric severity of MR, but it does provide clues to the hemodynamic consequences of MR.
- A low MR peak velocity (e.g., 4 m/sec) suggests hemodynamic compromise (↓ BP/↑ LA pressure).
- The contour of the velocity profile and its density are useful.
- A truncated, triangular jet contour with early peaking of the maximal velocity indicates ↑ LA pressure or a prominent regurgitant pressure wave.
- The density of the CWD signal is a qualitative index of MR severity
- a dense signal suggests significant MR
- a faint signal is likely to be mild or trace MR.
- CWD should also be used to interrogate the TR jet to estimate PA systolic pressure, another indirect clue as to MR severity and compensation for the volume overload.
Pulsed Wave Doppler
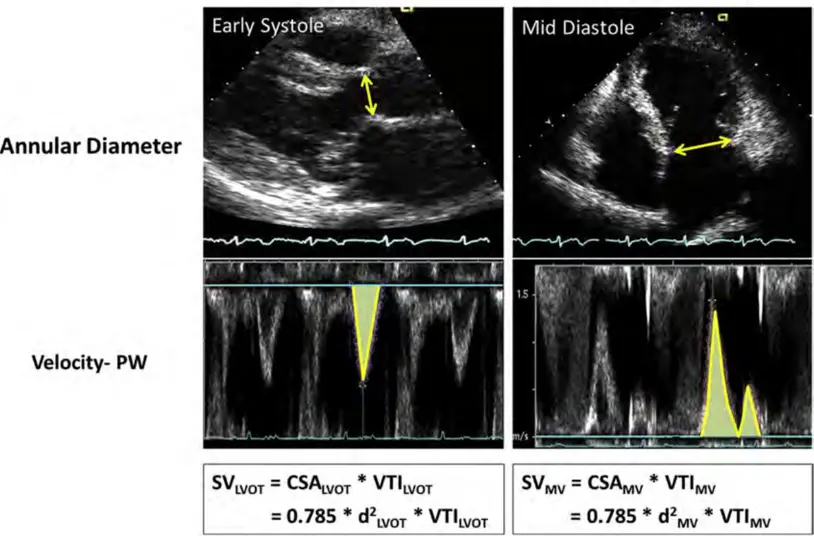
- Pulsed Doppler methods can be used to calculate SVs at the LVOT and MV level and determine RVol and RF.
- RVol can also be calculated by comparing Doppler LVOT SV to total LV SV derived from LV volumes.
- Pulsed Doppler tracings at the mitral leaflet tips are commonly used to evaluate LV diastolic function but can be helpful in MR.
- Patients with severe MR have a dominant early filling (increased E velocity) due to increased diastolic flow across the MV (E velocity is usually ≥1.2 m/sec).
- An impaired relaxation pattern with a low E velocity and A wave dominance virtually excludes severe MR.
- Because of the effect of relaxation on mitral inflow indices, these observations are more applicable in individuals older than 50 years of age or in conditions of impaired myocardial relaxation.
- The mitral inflow pattern is more reliable for assessing primary MR because, in secondary MR, it is difficult to determine whether E dominance is due to significant MR or elevated LV filling pressures.
- ⚠️ Peak E velocity is also affected by even mild degrees of mitral stenosis in the presence of rheumatic disease, MAC, or a mitral annular ring.
Regurgitant Volume (RVol) and Regurgitant Fraction
The example below is from Figure 4 of the 2 showing Doppler calculations of SV at the LVOT and MV annulus sites. In this example of severe MR, was 183 mL (d = 3.5 cm, VTI = 19 cm) and was 58 mL (d = 2.3 cm, VTI = 14 cm). This yielded an RVol of 125 mL () and an RF of or 68%.
Also see Figure 16 from 1 shown above in the Flow Convergence (PISA) section.
Pulmonary Vein Flow
Pulsed Doppler of pulmonary venous flow is a useful adjunct to evaluating the hemodynamic consequences of MR. With increasing severity of MR, there is a diminution of the systolic velocity, culminating with systolic flow reversal in severe MR.
- Since the MR jet may selectively enter a vein, sampling more than one vein is recommended, especially during TEE.
- One limitation of the pulmonary venous pattern is that elevation in LA pressure of any etiology as well as atrial fibrillation may also result in a blunted systolic forward flow. Thus, systolic blunting is less valuable in secondary MR than in primary MR. ∴, the pulmonary venous flow pattern should be used adjunctively with other parameters.
- Nevertheless, the finding of systolic flow reversal in more than one pulmonary vein is specific for severe MR.
- If the MR is confined to late systole, flow reversal may be present only during late systole. It is also important to distinguish true systolic flow reversal from contamination by the MR jet itself, a more difficult task during TTE compared with during TEE.
When to get TEE?
TEE is indicated to evaluate MR severity in patients in whom TTE is inconclusive or technically difficult. In addition, TEE is particularly well suited to identify the underlying mechanism of MR and for planning MV surgery or percutaneous valve procedures and provides overall a better accuracy in localizing MV pathology. 12 The majority of the above methods of quantifying MR can be used during TEE. In particular, the higher resolution of TEE, multiplane and 3D capabilities, and proximity to the MV makes VC imaging and PISA easier and probably more accurate. Furthermore, interrogation of all pulmonary veins is generally feasible and better than with TTE. A few cautionary points are worth mentioning regarding TEE. Since jet size is affected by transducer frequency, PRF, and signal strength, the same jet may appear larger on TEE compared with on TTE. Because sedatives are used, careful attention to blood pressure is important; secondary MR may appear less severe if the blood pressure is significantly lowered. Quantitative pulsed Doppler is more challenging and is the most affected quantitative MR parameter with TEE: acquisition of pulsed Doppler in the LVOT is usually hampered by angulation issues, leading to underestimation of systemic output.
When to get Cardiac MRI?
CMR offers several important advantages in the assessment of MR. This includes identifying the mechanism of MR, quantifying MR severity, and determining its consequences on cardiac remodeling.
- Mechanism of MR. Like echocardiography, CMR can provide information about the mechanism of MR by identifying morphologic abnormalities of the MVapparatus. 148 The presence of billowing, prolapse, or flail segments can be identified by dedicated cine imaging performed through the different scallops of the MV leaflets (Figure 17). 149,150 In secondary MR, CMR offers accurate assessment of LV dilation and function in addition to identification of myocardial and papillary muscle scar (Figure 17). 151,152
- Methods of MR Quantitation. MR can be assessed using several techniques by CMR. This includes qualitative or semiquantitative visual assessment of MR jet based on spin dephasing in the LA, 153 measurement of the VCA or anatomical regurgitant orifice area on short-axis cine of phase-contrast images, 77,154 and quantification of RVol and RF. 155-157 Among these techniques, quantification of RVol and fraction is recommended (Figures 8 and 17). The suggested preference order for calculation of RVols is the use of
- The difference between LV SV using planimetry of short-axis cine images and aortic SV obtained by phase-contrast images
- The difference in LV and RV SV by endocardial contouring of LV and RV cine images
- The difference between the mitral inflow SVand aortic SV by phase-contrast imaging
The RF can be calculated by dividing the RVol by the LV SV for the first two methods and by the mitral inflow SV for the third method.
- LV and LA Volumes and Function. CMR provides the most accurate and reproducible assessment of LV volume and ejection fraction and LA volume. All measurements should be indexed to BSA, and remodeling can be assessed based on existing reference values. 158,159
- When Is CMR Indicated? The primary indication of CMR is the evaluation of MR severity when assessment by echocardiography is felt to be unsatisfactory or when there is a discrepancy between MR severity and clinical findings. CMR may provide additional information about the mechanism of MR and myocardial viability, both of which may have implications for surgical intervention, and CMR importantly provides quantitative evaluation of chamber size, RVol, and fraction.
Examples
Flail Leaflet
Non-holosystolic MR
MR quantification in MVP
⛔ Avoid using single frame measurements - PISA EROA and VCW - when the MR is not holosystolic as they can overestimate MR severity.
When not holosystolic, you should use regurgitant volume (RVol) method.
- Examples of non-holosystolic MR include:
- MVP with late systolic MR
- functional MR with biphasic MR
- LV dyssynchrony with early systolic MR