- When AR is detected, the evaluation starts:1
- assessment of the anatomy of the aortic valve and root to determine the etiology of the regurgitation
- an assessment of LV size, geometry, and function
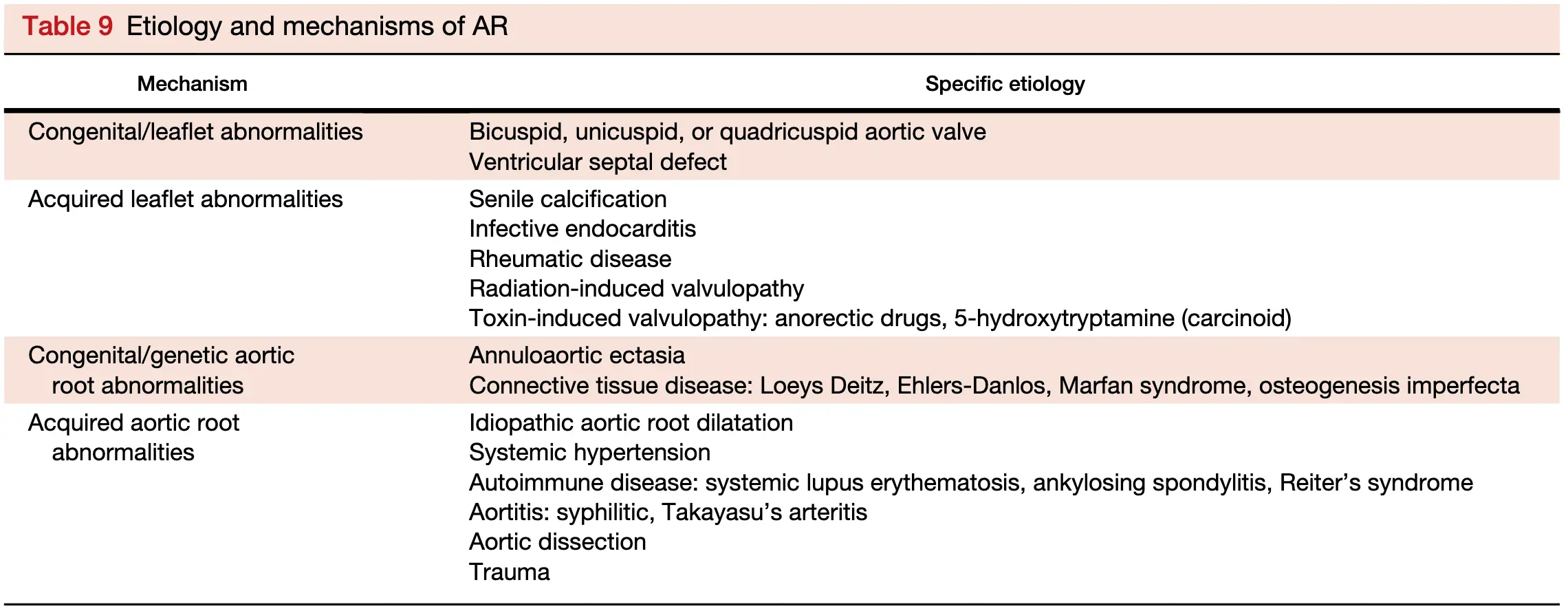
 Type Ia depicts sinotubular junction enlargement and dilatation of the ascending aorta. Type Ib depicts dilatation of the sinuses of Valsalva and sinotubular junction. Type Ic depicts dilatation of the ventriculoarterial junction (annulus). Type Id denotes aortic cusp perforation. Type II is associated with excessive leaflet motion from leaflet prolapse as a result of either excessive leaflet tissue or commissural disruption. Type III is associated with restricted leaflet motion seen with congenitally abnormal valves, degenerative calcification, or any other cause of thickening/fibrosis or calcification of the valve leaflets.
Type Ia depicts sinotubular junction enlargement and dilatation of the ascending aorta. Type Ib depicts dilatation of the sinuses of Valsalva and sinotubular junction. Type Ic depicts dilatation of the ventriculoarterial junction (annulus). Type Id denotes aortic cusp perforation. Type II is associated with excessive leaflet motion from leaflet prolapse as a result of either excessive leaflet tissue or commissural disruption. Type III is associated with restricted leaflet motion seen with congenitally abnormal valves, degenerative calcification, or any other cause of thickening/fibrosis or calcification of the valve leaflets.
Acute Aortic Regurgitation
- Similar to MR, the hemodynamics and cardiac adaptation to acute versus chronic AR are quite different. In severe acute AR, the LV is not dilated and the sudden rise in LV end-diastolic pressure may cause the MV to close prematurely, best documented with an M-mode.1
- Causes include
- valve abnormalities, e.g. Endocarditis
- aorta abnormalities, e.g. Aortic Dissection
- iatrogenic complications, e.g. blunt chest trauma or transcatheter procedure
- Acute AR: acute volume overload → severe pulmonary congestion and low cardiac output
Chronic Aortic Regurgitation
- AR in most patients is easily seen with color flow Doppler as a mosaic blend of colors originating from the aortic valve during diastole.1
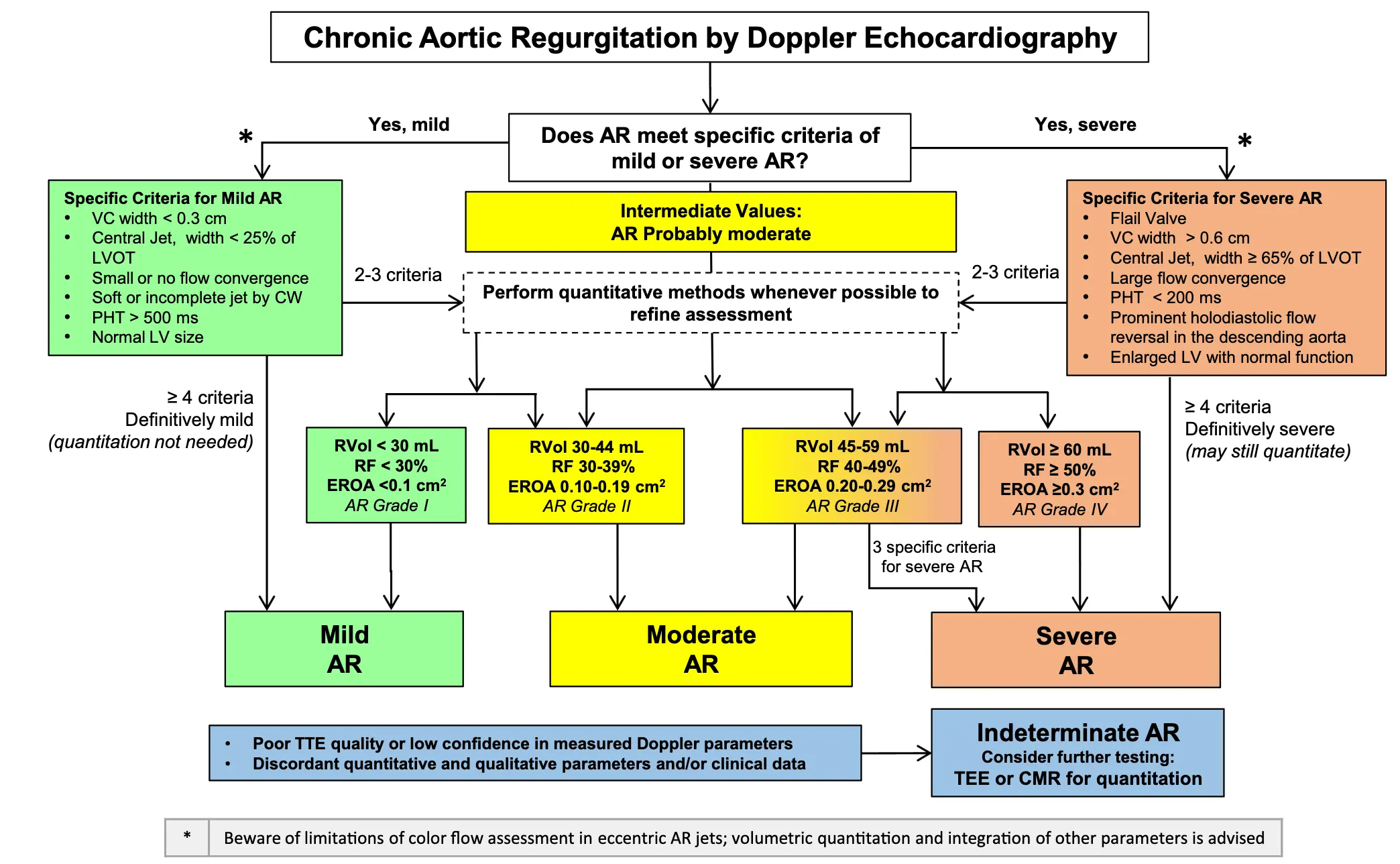
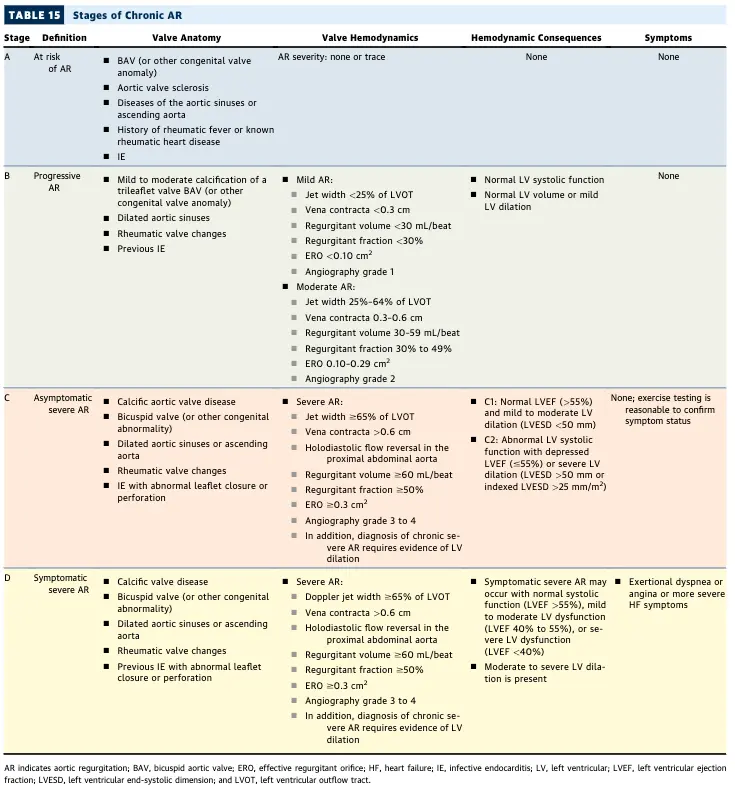
- Stages A-D
- A: at-risk
- B: progressive AR
- C: severe, but asymptomatic
- D: severe, symptomatic AR
Management
Surveillance with repeat non-invasive testing, e.g. repeat TTE
| Stage | Frequency of Echo Monitoring |
|---|---|
| Progressive (Stage B) | Mild: every 3-5 years Moderate: every 1-2 years |
| Severe (Stage C) | every 6-12 months Dilating LV: more frequently |
- 📝 Outcomes are optimal when surgery is performed before LVEF decreases below 55% 2
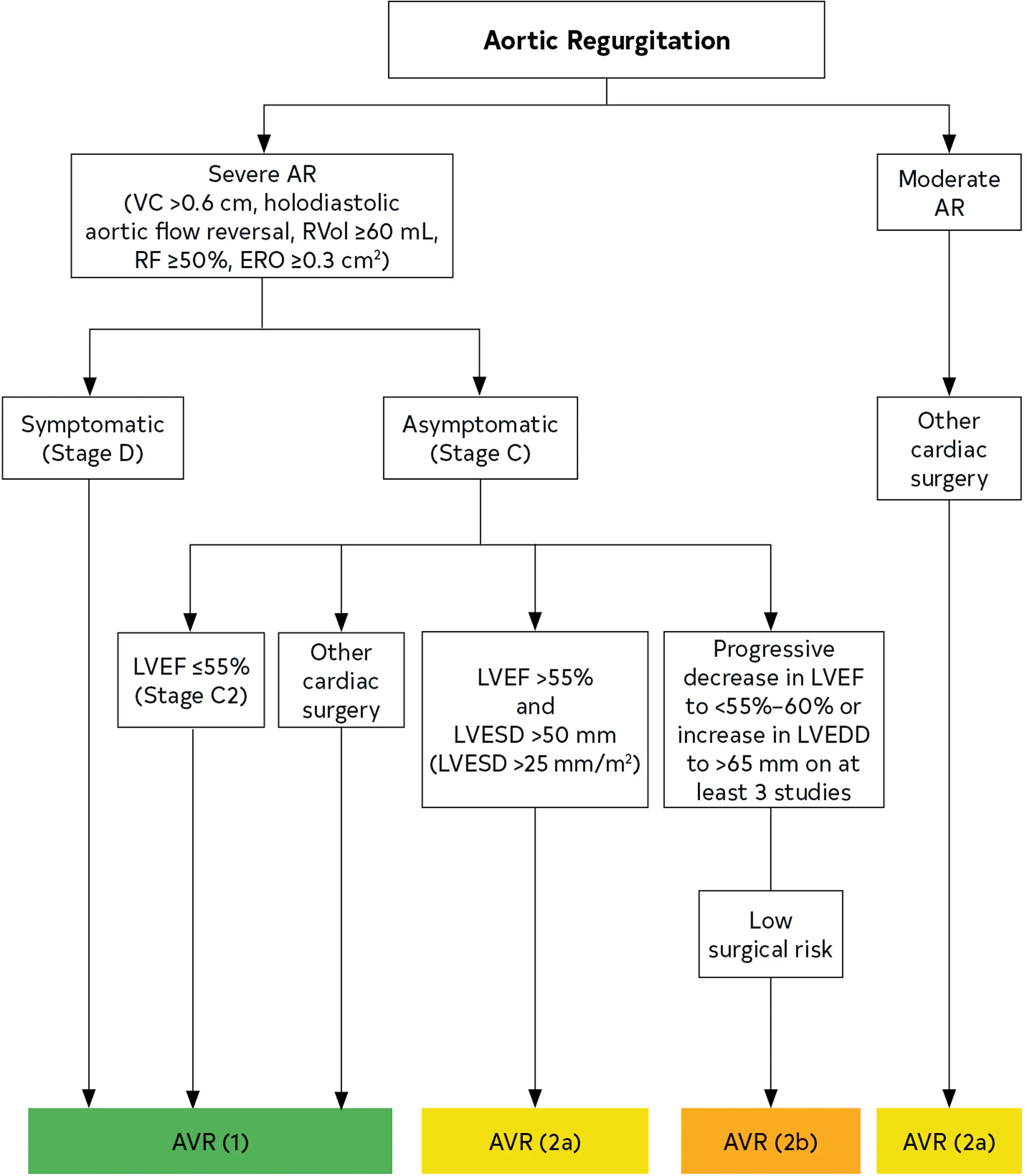
- Who gets surgery? 2
- Severe, symptomatic AR (Stage D)
- Severe, asymptomatic AR (Stage C) if
- LVEF ≤ 55% (Stage C2)
- LVEF > 55%, but LVESD >50 mm (or indexed LVESD > 25 mm/m2)
- Already undergoing cardiac surgery for another reason
- Moderate AR (Stage B) who is already undergoing cardiac or aortic surgery for other indications, aortic valve surgery is reasonable (Class 2a)
- Consider in asymptomatic patients with severe AR and normal LV systolic function at rest (LVEF >55%; Stage C1) and low surgical risk, aortic valve surgery may be considered when there is a progressive decline in LVEF on at least 3 serial studies to the low–normal range (LVEF 55% to 60%) or a progressive increase in LV dilation into the severe range (LV end-diastolic dimension [LVEDD] >65 mm) (Class 2b)
- In asymptomatic patients with chronic AR (Stages B and C), treatment of hypertension (systolic blood pressure >140 mm Hg) is recommended (Class 1) 2
- In patients with severe, symptomatic AR and/or LV systolic dysfunction (Stages C2 and D) but a prohibitive surgical risk, GDMT for reduced LVEF with ACE inhibitors, ARBs, and/or sacubitril/valsartan is recommended (Class 1) 2
- Measures of LV systolic function (LVEF or fractional shortening) and LV end-systolic dimension (LVESD) or LV end-systolic volume are predictive of the development of HF symptoms or death in initially asymptomatic patients (Stages B and C1) and are significant determinants of survival and functional results after surgery in asymptomatic and symptomatic patients (Stages C2 and D)2
- Symptomatic patients (Stage D) with normal LVEF have a significantly better long-term postoperative survival rate than those with depressed systolic function.2
- 📝 In patients with moderate or severe AR and suboptimal TTE images or a discrepancy between clinical and TTE findings, TEE, CMR, or cardiac catheterization is indicated for the assessment of LV systolic function, systolic and diastolic volumes, aortic size, and AR severity (Class 1) 2
Exam
- Wide pulse pressure
- Effect of lowering the heart rate, e.g. with BBs
- Longer diastolic time allows more volume to flow back into the LV
- I’ve seen permitting a slightly elevated HR to ↓ diastolic regurgitant filling
- In some patients this may result in a paradoxical apparent ↑ in BP
- Longer diastolic time allows more volume to flow back into the LV
Echo
There is no such thing as "physiologic" AI
While ‘‘physiologic’’ or mild degrees of tricuspid and PR are commonly noted in normal exams, AR is not. When AR is detected, the evaluation starts with an assessment of the anatomy of the aortic valve and root to determine the etiology of the regurgitation followed by an assessment of LV size, geometry, and function.
- Determine whether there is rapid equilibration of the aortic and LV diastolic pressures; visualizing the aortic root; and evaluating LV size and systolic function
- AR usually lasts throughout diastole except in acute AR, where it may be brief and of lower velocity, making detection and assessment with color Doppler more difficult.1
- Because the length of the AR jet into the LV chamber is so dependent on the driving pressure (diastolic blood pressure), it is not a reliable parameter of AR severity.1
LV should be dilated with chronic AI (and MR)
Chronic severe AR almost always leads to dilated LV, and thus, normal chamber volumes are unusual with chronic severe AR.1
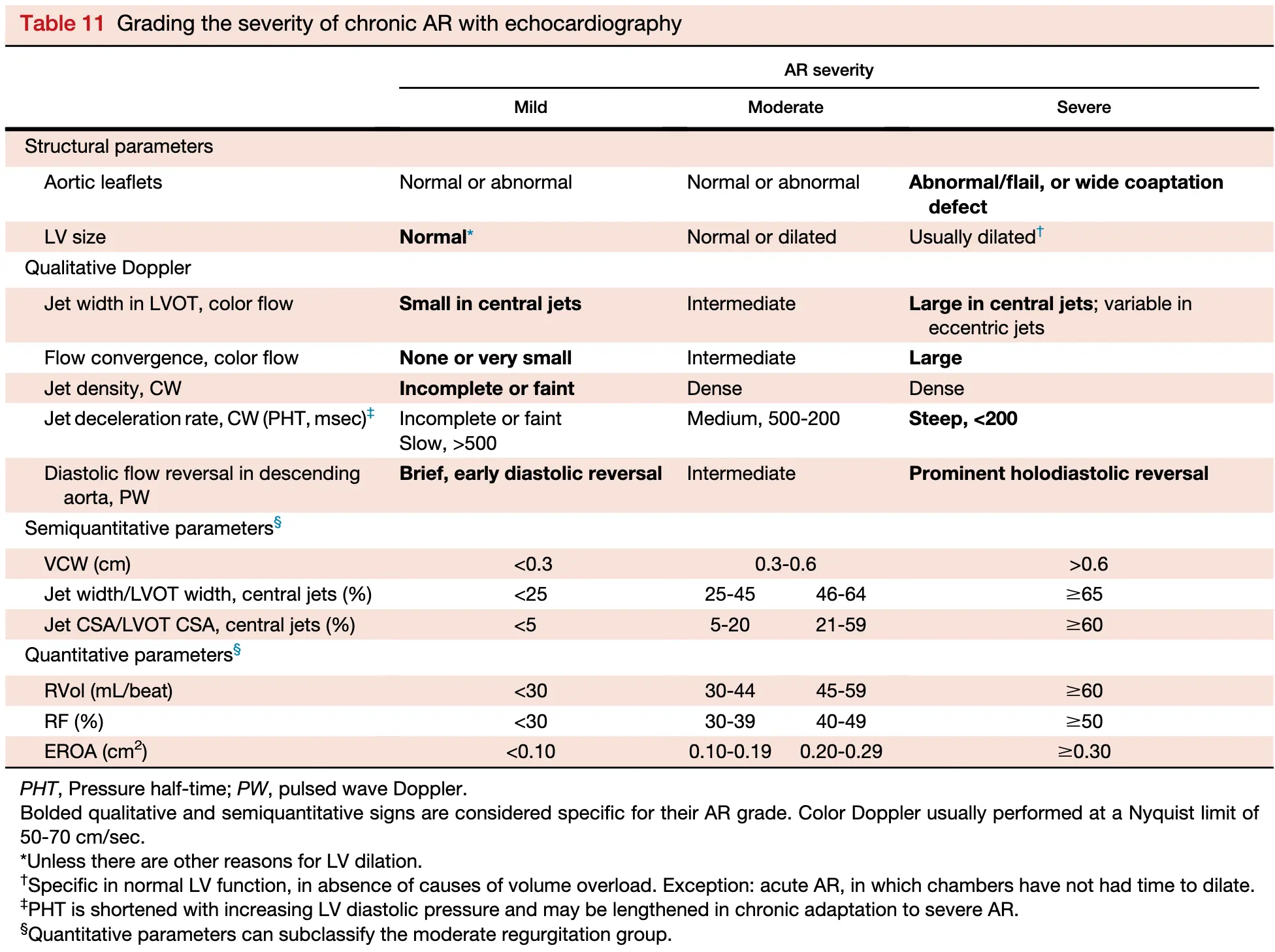
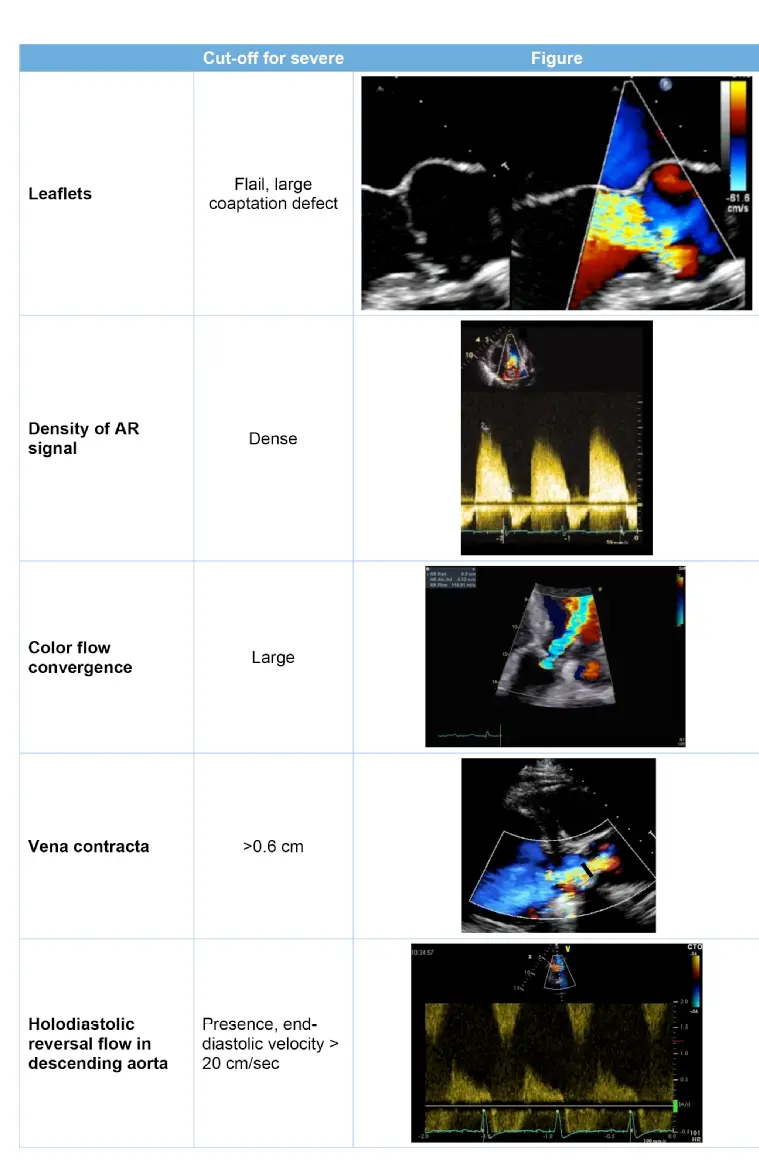 Figure source
Figure source
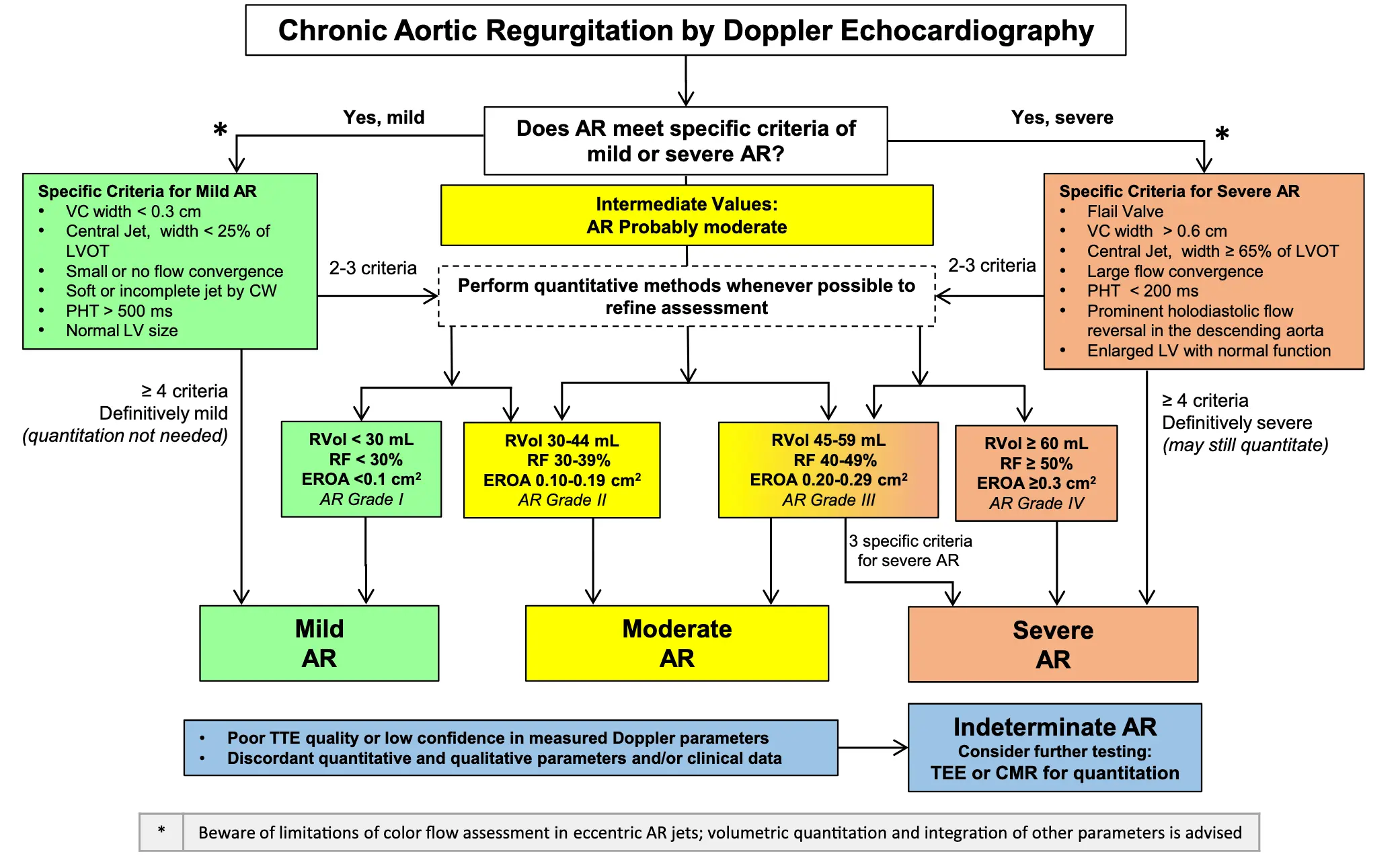
Vena Contracta Width
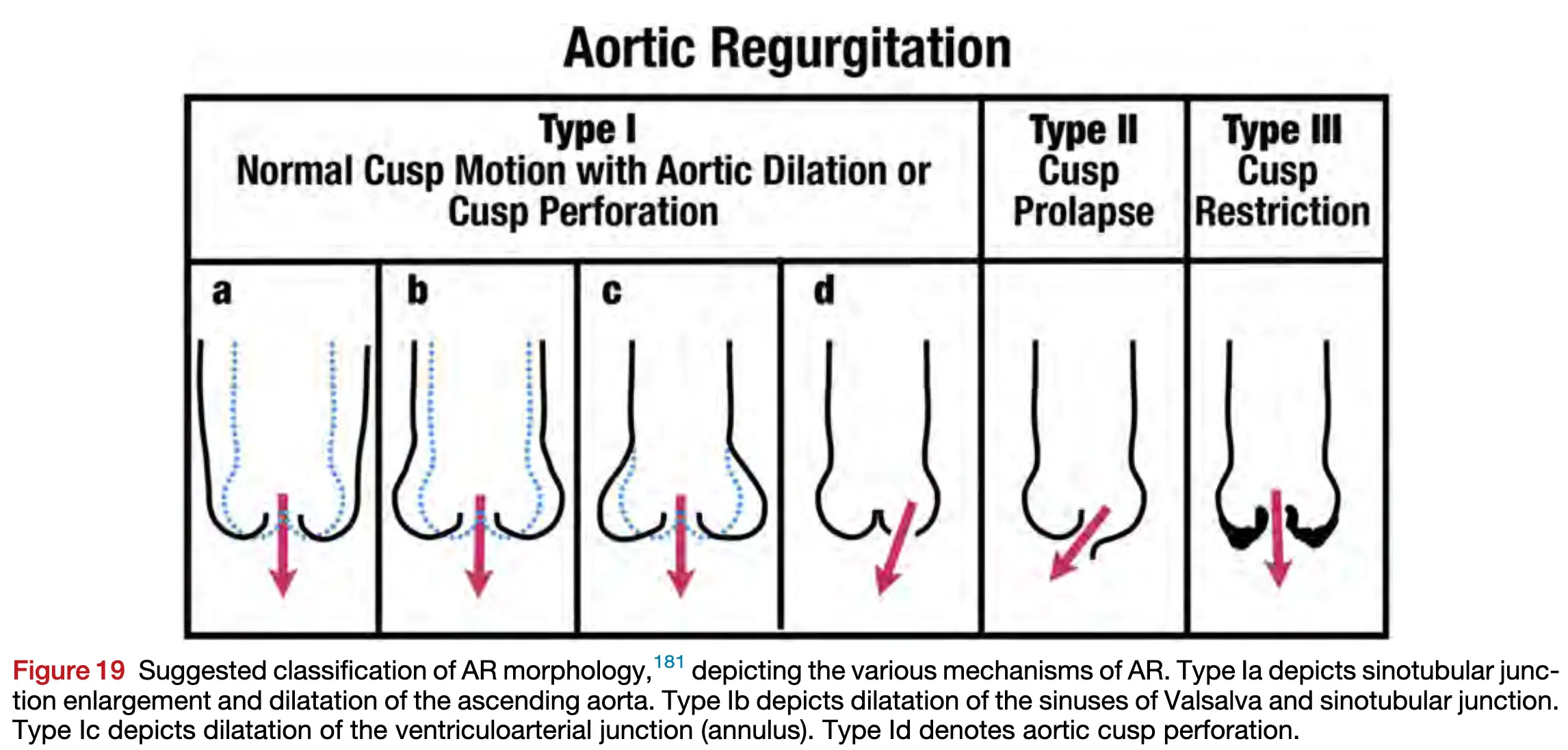
- A VC < 0.3 cm indicates mild, 0.3-0.6 cm indicates moderate, and > 0.6 cm indicates severe AR.1
- 📝 If optimized, VC can still be measured in most eccentric jets.
CWD
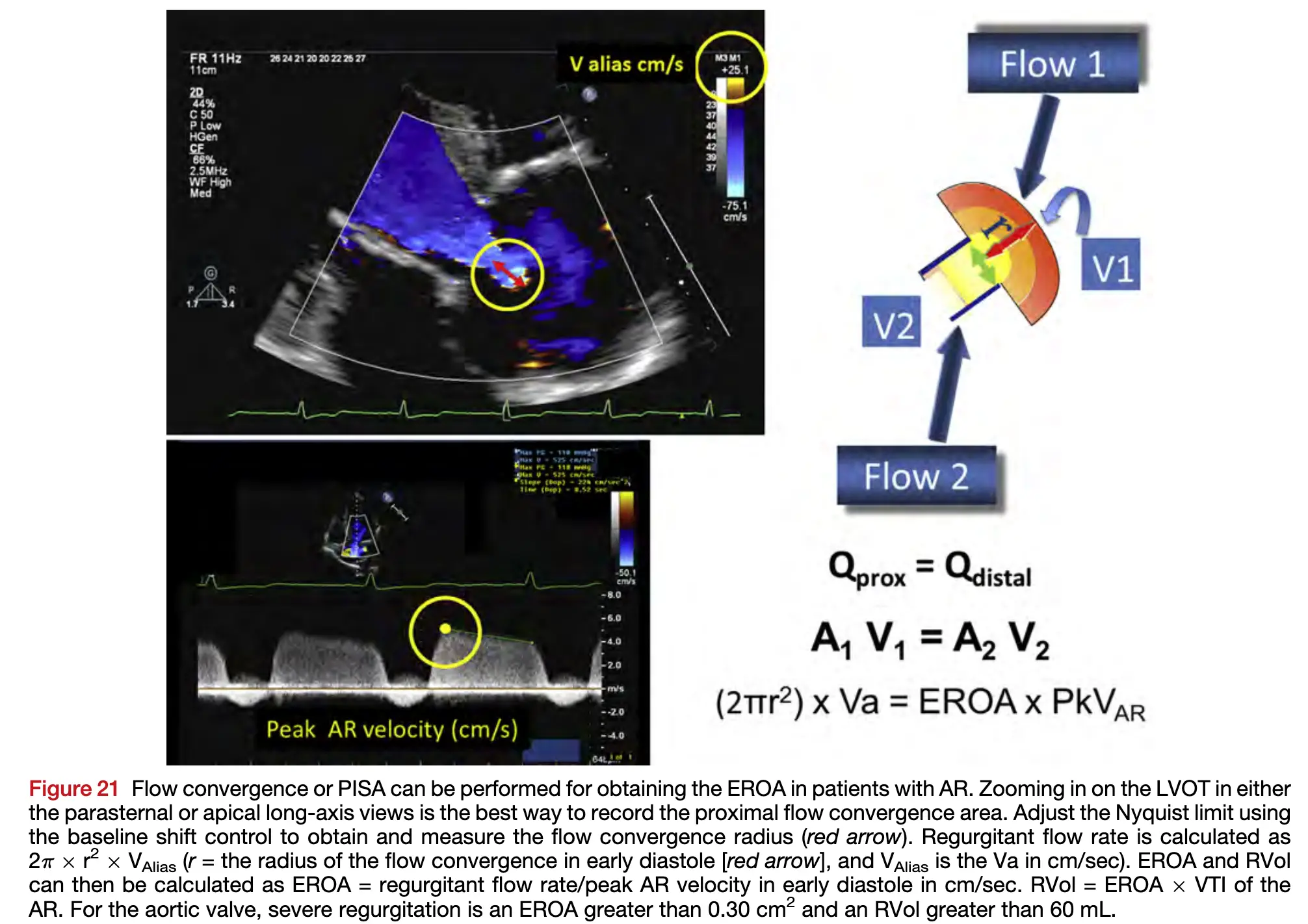
- Measurement of the AR peak velocity and VTI by CWD allows calculation of the EROA and RVol
- The threshold for severe AR is an EROA ≥0.30 cm^2 and an RVol > 60 mL
PWD
- PWD: Holodiastolic flow reversal is an abnormal finding and indicates at least moderate AR; when present in the abdominal aorta, it is consistent with severe AR.
- Holodiastolic reversal (flow throughout diastole) strongly suggests moderate to severe AR
- End-diastolic velocity: a value >20 cm/s in the descending aorta often suggests severe AR, correlating with an aortic regurgitant fraction ≥ 40%
- Ratio of peak systolic velocity to End-diastolic velocity: a lower ratio (e.g., <5.0) indicates greater regurgitation
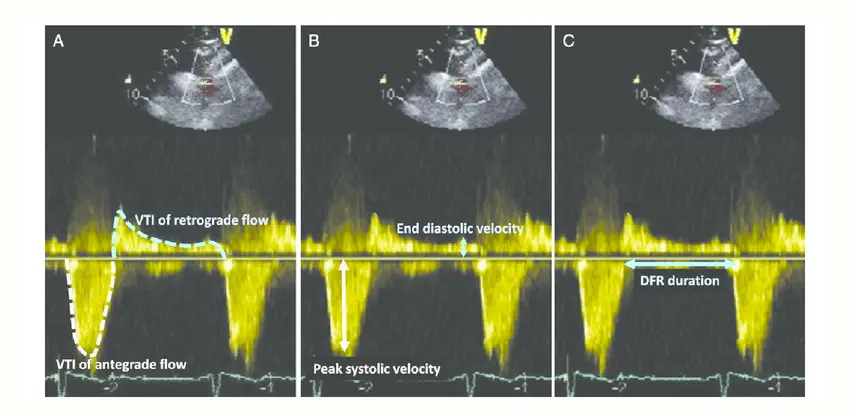
Figure source
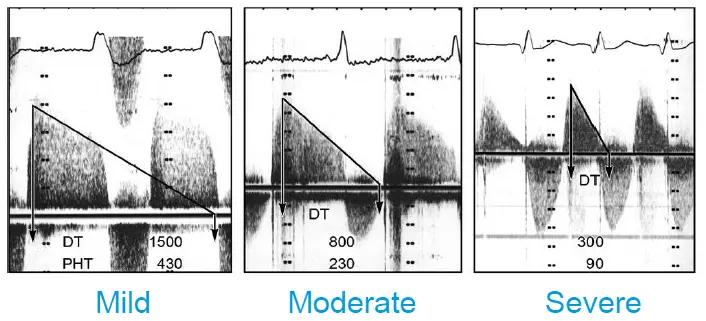
Pressure Half Time (PHT)
Don't use PHT alone for diagnosis of AR severity
Important limitations of PHT in aortic regurgitation, so don’t base determination on PHT alone.
Recall,
and valve area is inversely proportional to PHT, i.e. larger PHT is associated with smaller valve area.
-
PHT < 200 msec → Severe
-
PHT 200-500 msec → Moderate
-
PHT > 500 msec → Mild
-
A pressure half-time of <300 ms on the AR velocity curve indicates rapid equilibration of the aortic and LV diastolic pressures.2
- A pressure half-time >500 msec suggests mild AR, and <200 msec suggests severe AR. However, since this parameter is affected by compliance of the LV, patients with severe chronic regurgitation with well compensated ventricular function may have a pressure half-time in the ”moderate” range. In contrast, mild AR in patients with severe diastolic dysfunction may have short pressure half-time. The pressure half-time reflects reduction in the transvalvular gradient, which can also be accomplished by vasodilator therapy (reduces diastolic blood pressure independent of the AR). Thus, this method is less useful for monitoring AR in patients being treated medically.1
Examples:
Cardiac CT
- CT imaging is the primary approach for diagnosis of acute aortic dissection because it is highly accurate and continuously available at most medical centers.2
Cardiac MRI
When Is CMR Indicated? While echocardiography remains the first line modality for assessment of AR, CMR is indicated in the following situations: (1) suboptimal echocardiographic images; (2) discordance between echocardiographic and Doppler findings (i.e., discordance between LV enlargement and Doppler measures of AR severity); or (3) discordance between clinical assessment and severity of AR by echocardiography 209 ; (4) patients with moderate or severe AR and suboptimal echocardiography for assessment of LV volumes and systolic function and measurement of AR severity 209 ; (5) patients with bicuspid aortic valves, when the morphology of aortic sinuses, sinotubular junction, or ascending aorta (to at least 4 cm above the valve plane) cannot be assessed accurately or fully by echocardiography. 209,210 Lastly, the direct method for AR quantification described in this section is independent of other coexisting valvular lesions, and therefore CMR may be used in the setting of multiple valvular lesions when echocardiographic assessment may be challenged. This will be presented in more detail in the section on multivalvular disease.1
Footnotes
-
https://www.asecho.org/wp-content/uploads/2017/04/2017VavularRegurgitationGuideline.pdf ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9
-
Otto, C. M., Nishimura, R. A., Bonow, R. O., Carabello, B. A., Erwin, J. P., Gentile, F., Jneid, H., Krieger, E. V., Mack, M., McLeod, C., O’Gara, P. T., Rigolin, V. H., Sundt, T. M., Thompson, A., & Toly, C. (2021). 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. Journal of the American College of Cardiology, 77(4), e25–e197. https://doi.org/10.1016/j.jacc.2020.11.018 ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9