- The main pericardial syndromes that are encountered in clinical practice include
- Pericarditis (acute, subacute, chronic and recurrent)
- Pericardial Effusion
- Pericardial Tamponade
- Constrictive Pericarditis
- Pericardial masses
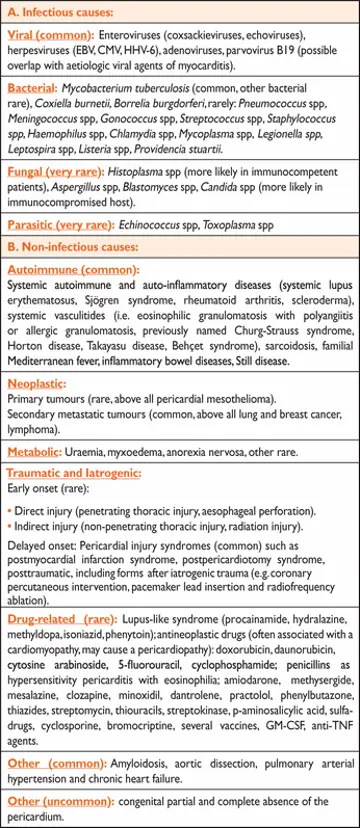
- Etiology can be broken down into Infectious versus Non-infectious 1
Pericardium
- The pericardial sac has two layers, a serous visceral layer (also known as epicardium when it comes into contact with the myocardium) and a fibrous parietal layer. It encloses the pericardial cavity, which contains pericardial fluid.
- The pericardial sac encompasses both ventricles, the right atrium (RA), and most of the LA, whereas the pulmonary venous system and the majority of the SVC and IVC are external to the pericardium.2
- Because most of the SVC and IVC are not intrathoracic, they are largely unaffected by swings in intrathoracic pressure
- Inspiration: diaphragm drops → ↓ intrathoracic pressure (~5-10 mmHg) that is fully transmitted to the cardiac chambers, which augments Right Heart filling. Because the pulmonary veins are entirely intrathoracic, there is a uniform drop in pressure w/in the pulmonary veins and L-sided heart chambers. ∴ L-sided filling does not significantly alter during respiration
- NOTE: R- and L-sided diastolic pressures vary independent of one another during respiration, whereas systolic pressures parallel one another, falling with inspiration and rising with expiration, mirroring intrathoracic pressures
- Under normal circumstances with a normal pericardium and a compliant RV, chamber distention caused by increased flow is easily accommodated, and therefore does not result in significant inspiratory rise in pressures
- Expiration: During expiration, right-sided filling decreases relative to inspiration, whereas left-heart filling remains relatively constant
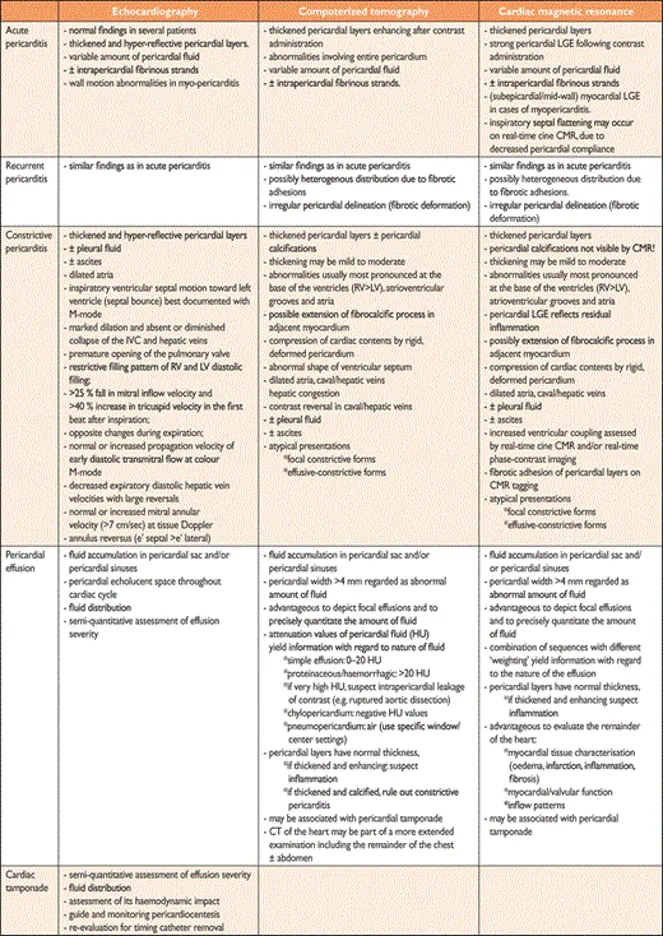
Imaging for Pericardial Diseases
- 🌟 Cardiac MRI is probably the preferred imaging modality to optimally assess pericardial disease
- CMR
- Similar to CT, the normal pericardium appears on T1-weighted imaging as a thin hypointense (‘dark’) curvilinear structure surrounded by hyperintense (‘bright’) mediastinal and epicardial fat.
- Normal pericardial thickness ranges from 1.2 to 1.7 mm.
- CMR can accurately distinguish between mixed myopericardial diseases such as mixed inflammatory forms (e.g. myopericarditis or perimyocarditis) and post-myocardial infarction pericardial injury.
- Compared with CT, CMR has the advantage of providing information with regard to the haemodynamic consequences of the non-compliant pericardium on cardiac filling, and has the potential of showing fibrotic fusion of pericardial layers.
See Table 12 of 1 for nice comparison.
Footnotes
-
Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. European Heart Journal. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318 ↩ ↩2
-
Geske JB, Anavekar NS, Nishimura RA, Oh JK, Gersh BJ. Differentiation of Constriction and Restriction. Journal of the American College of Cardiology. 2016;68(21):2329-2347. doi:10.1016/j.jacc.2016.08.050 ↩