Narrow QRS Complex tachycardias
Narrow QRS complex tachycardias are fast cardiac rhythms (generally more than 100 bpm) with a QRS duration of 100 ms or less.
- SVT is a “grab bag” of tachyarrythmias originating “above the ventricle”
- The most commonly encountered Paroxysmal SVTs are:
- AVNRT (60%)
- AVRT (30%)
- most common PSVT seen in the pediatric population
- Atrial Tachycardia (<10%)
graph TD A[QRS Width] --> B(Narrow Complex Tachycardia) B --> C[Irregularly irregular] B --> D[Regular or Regularly irregular] D --> |Look for P waves| E[Assess RP interval] C --> F[1. AF<br>2. MAT<br>3. Atrial flutter w/ variable conduction] E --> |Sawtooth P waves| G(Atrial flutter) E --> |Short PR, <1/2 RR| H(AVRNT<br>AVRT<br>Atrial flutter<br>Atrial tachy w/ long PR) E --> |Long RP, >1/2 RR| I(Atrial tachy<br>Atrial flutter<br>SNRT<br>Atypical AVNRT<br>Atypical AVRT: PJRT)
- The most common mechanism that underlies narrow QRS complex tachycardias (excluding sinus tachycardia) is reentry
- Other mechanisms of tachycardia include “triggered activity” and “automaticity.”
- The most common causes of SVT are abnormal automaticity or re-entry.
- Starts with an A, ends with a V
- Intracardiac tracings show the normal intervals
- initiation of atrial depolarization A
- His bundle activation H
- Ventricular depolarization V
- AH + HV = PR interval
-20241223150251158.webp)
- Most common is Atrial Fibrillation (AFib)
- Paroxysmal supraventricular tachycardias (PSVT) includes:
- AV Nodal Reentrant Tachycardia (AVNRT) (65%)
- AV reentry tachycardia (AVRT), aka ORT (Orthodromic re-entrant tachycardia) (35%)
- WPW
- AV reentry over concealed bypass tract
- Atrial Tachycardia (5%)
- Adenosine is effective for AVNRT and AVRT, aka ORT
- Not effective in patients with Atrial Tachycardia
- Short R-P tachycardia
- AVNRT - virtually absent p waves, regular R-R interval
- Orthodromic Reciprocating Tachycardia (ORT) - retrograde p waves in terminal portion of QRS, regular R-R interval
- Long R-P tachycardia
- ORT - retrograde p waves in T wave, regular R-R interval
- A Tach - atypical p wave axis, up to 30% variability in R-R interval (“wobble” can appear a touch irregular)
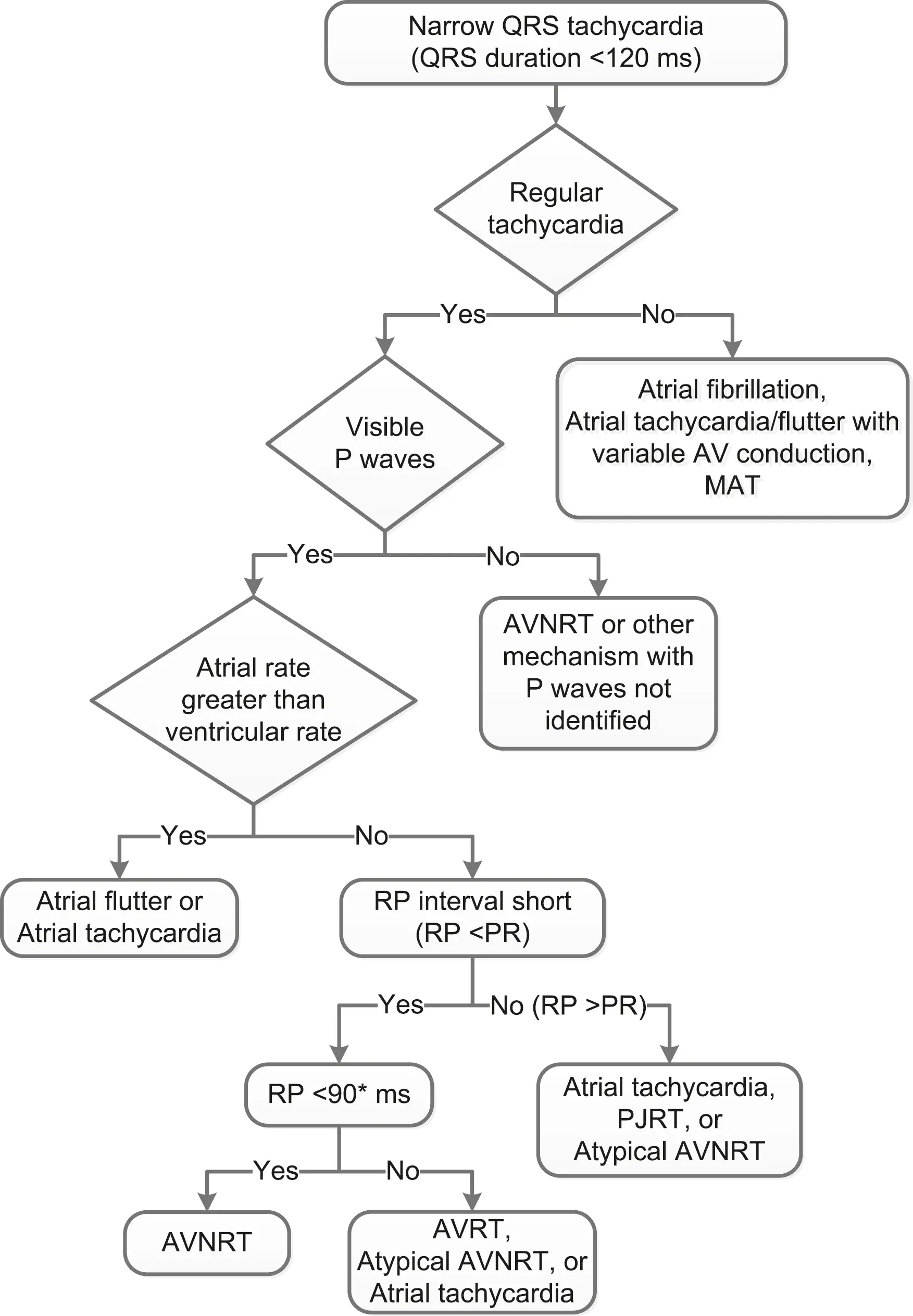
DDx of Regular Narrow Complex Tachycardias
Best deduced by first assessing the relationship of atrial activity (P waves) to the QRS complex. P waves with a morphologic appearance identical to that of the sinus P waves are probably due to tachycardias initiated in (or near) the sinus node, regardless of mechanism.
Regular
- Sinus Tachycardia
- Atrial Flutter
- Atrial Tachycardia
- AV Nodal Reentrant Tachycardia (AVNRT)
- Junctional Tachycardia
- Permanent Junctional Reciprocating Tachycardia
- Nonparoxysmal Junctional Tachycardia
- Sinus Nodal Reentrant Tachycardia
- AV Reentrant Tachycardia (AVRT)
-20241223152259702.webp)
| Short RP (RP < PR) | Long RP (RP > PR) |
|---|---|
| AVNRT AV Reentrant Tachycardia (AVRT) Nonparoxysmal junctional tachycardia | Sinus Tachycardia Sinus nodal reentrant tachycardia (SNRT) Atrial Tachycardia Permanent Junctional Reciprocating Tachycardia Nonparoxysmal Junctional Tachycardia Atypical AV Nodal Reentrant Tachycardia (AVNRT) Atypical AV reentrant tachycardia |
P wave that is morphologically similar to sinus P waves → tachycardia is initiated in (or near) the sinus node. 3 general situations are possible:
- atrial activity precedes QRS complex w/ a normal delay
- In such cases, the RP intervals are longer than the PR intervals, and the tachycardia is designated a “long RP tachycardia”
- P waves occur simultaneously with or shortly after the QRS complex (i.e., in the ST segment or T wave) and thus yield a “short RP tachycardia”
- no relationship may exist between atrial activity and the QRS complex
- AV dissociation
Irregular
- Atrial Fibrillation (AFib)
- Multifocal Atrial Tachycardia
- Atrial Flutter with variable conduction
ECG Clues
- Atrial Fibrillation (AFib), Atrial Flutter
- In the majority of AVNRT, the retrograde P waves occur during the QRS complex and are ∴ invisible on the 12-lead ECG.
- Other flavors of PAT - Bypass tract-mediated macro-re-entry (e.g., AVRT, WPW), Intra-atrial re-entry, and SA nodal re-entry - will have P waves usually identifiable on 12-lead ECG on careful inspection.
- Bypass tract-mediated macro-re-entry (e.g., orthodromic AVRT, WPW): P waves are generated retrograde → tend to be negative in the inferior leads and have RP interval < PR interval (“short RP tachycardia”).
- 📝 because the RP interval is short, the retrograde P wave is often mistaken for a bump on the T wave by the unwary observer.
-20241223150322185.webp)
Response to Adenosine
-20241223150346794.webp)
Automatic SVT
-20241223150451649.webp)
- Relatively uncommon, except in the acutely ill patient.
- There will be an obvious metabolic disturbance, e.g. MI, acute COPD exacerbation, acute alcohol ingestion, and electrolyte disturbances.
- Rule out digoxin toxicity
- If the ventricular response is rapid enough to produce hemodynamic instability →
- Pharmacotherapy 💊: the ventricular rate can usually be slowed with digoxin (if toxicity ruled out), Beta-blockers, or CCBs.
- Consider overdrive pacing in the appropriate setting
Automatic Atrial Tachycardia
See Automatic Atrial Tachycardia
Re-entrant SVT
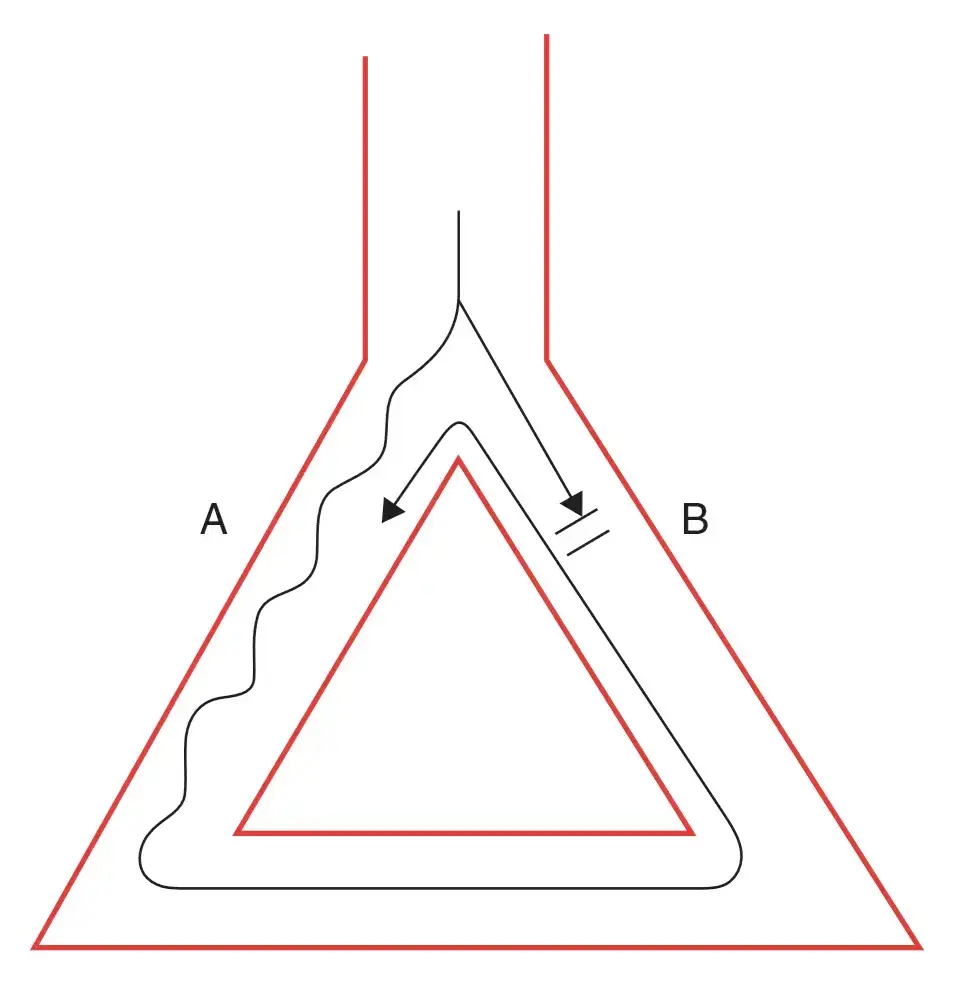 A core assumption here is that pathway A conducts slower, and has a shorter refractory period. Pathway B conducts faster, but has a longer refractory period. Recall, Dr. Gupta’s boat-and-wake analogy from AV Nodal Reentrant Tachycardia (AVNRT) where the fast boat creates a long wake (long refractory period) and the slow boat has a short wake. A signal that originates at the top of the diagram (above the branch) may conduct through both pathways. The signal conducted through A may conduct into B (e.g. if B is blocked → not in refractory period), which then continues conducting all the way through A again, creating a perpetual loop.
A core assumption here is that pathway A conducts slower, and has a shorter refractory period. Pathway B conducts faster, but has a longer refractory period. Recall, Dr. Gupta’s boat-and-wake analogy from AV Nodal Reentrant Tachycardia (AVNRT) where the fast boat creates a long wake (long refractory period) and the slow boat has a short wake. A signal that originates at the top of the diagram (above the branch) may conduct through both pathways. The signal conducted through A may conduct into B (e.g. if B is blocked → not in refractory period), which then continues conducting all the way through A again, creating a perpetual loop.
- Vast majority of ambulatory patients with SVT are d/t re-entry, i.e. patients who are not necessarily acutely ill.
- In contrast to re-entrant ventricular tachyarrhtymias, re-entrant SVT is usually seen in pts w/o chronic heart disease. Instead for re-entrant SVT the re-entrant substrate is often congenital. ∴ the typical patient is young and healthy.
- 5 general categories:
- AV nodal re-entry (60% of PAT)
- Bypass tract-mediated macro-re-entry (30% of PAT)
- Examples: AV Reentrant Tachycardia (AVRT), WPW
- Intra-atrial re-entry
- SA nodal re-entry
- Atrial Flutter/Atrial Fibrillation (AFib)
- 📝 the first four are sometimes lumped together into one large group as ‘Paroxysmal Atrial Tachycardia’
- Bypass tract-mediated macro-re-entrant tachycardia is a “macro-re-entrant” circuit because it involves the AV node, His-Purkinje system, the ventricular and atrial myocardia, and the bypass tract, i.e. the circuit consists of several types of cardiac tissue.
-20241223152409985.webp)
- If they conduct in the antegrade direction, the patient is said to have WPW and the surface ECG will show pre-excitation of the QRS complex.
- Unlike AVNRT where the atria and ventricles depolarize nearly simultaneously, in macro-re-entry the atria and ventricles depolarize sequentially → distinct P waves are virtually always seen.
- short-RP tachycardia, i.e. RP interval shorter than the PR interval, because of retrograde conduction via the bypass tract tends to be faster than antegrade conduction via the normal AV conducting system.
- P waves often negative in the inferior leads b/c atrial stimulation is in retrograde direction (P wave axis is superior/going upward)
- Treatment:
- BBs, CCBs, digoxin +/- Class Ia drugs
- ↑ refractory period of the AV node: BBs, CCBs, digoxin
- decreases the width of the tachycardia zone
- ↑ AV nodal block (→ induces Wenckebach when tachycardia begins)
- a single blocked beat will immediately terminate the tachycardia
- ↑ retrograde refractory period of the bypass tract with Class Ia drugs
- Downside: Class Ia drugs also ↑ the antegrade RP of the bypass tract → effectively ↑ the tachycardia zone. ∴ only use ‘em when trying to achieve “pharmacologic ablation”
- Anti-tachycardia Pacing (ATP): termination by programmed pacing
- Ablation is highly effective
- Intra-atrial reentry occurs when the reentrant circuit is completely within the atria, and does not include the AV node at all. This type of reentrant circuit generates P waves that look different from the standard sinus P wave. (Source)
- SA nodal re-entry, like the name implies, is contained within the SA Node. This type of reentry is interesting in that it is spontaneously occurring, and Atrial Fibrillation (AFib) does not exhibit the warm-up behavior that is usually observed with normal sinus tachycardia. The P waves it produces are identical to normal sinus P waves.