- All prosthetic heart valves have an expected amount of stenosis.
- Prosthetic valves are designed to have a small amount of regurgitation, i.e. “physiological closing volume.”
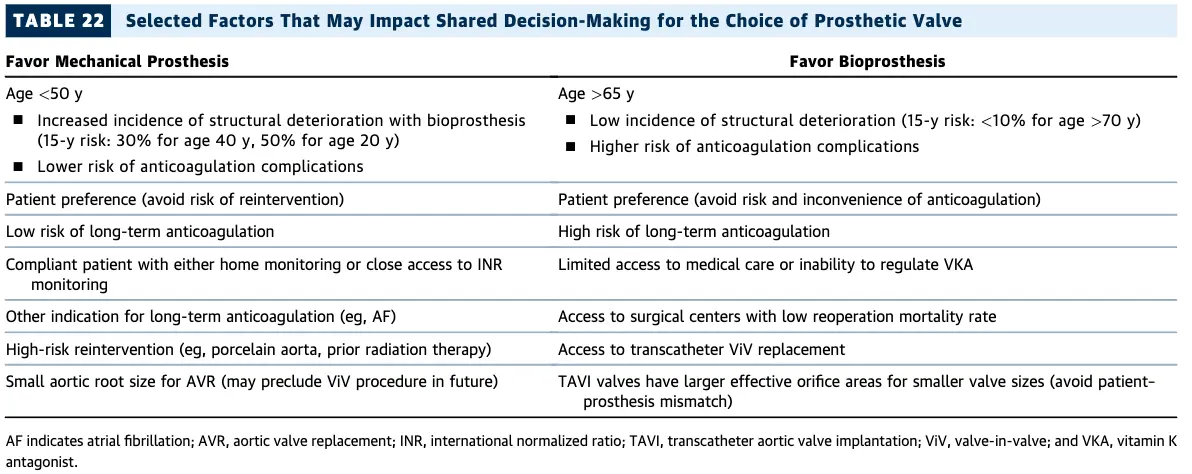
Which valve should they get?
Mechanical Prosthetic Valves
- Trade-off: More durable than bioprostheses, but more thrombogenic and require lifelong anticoagulation.
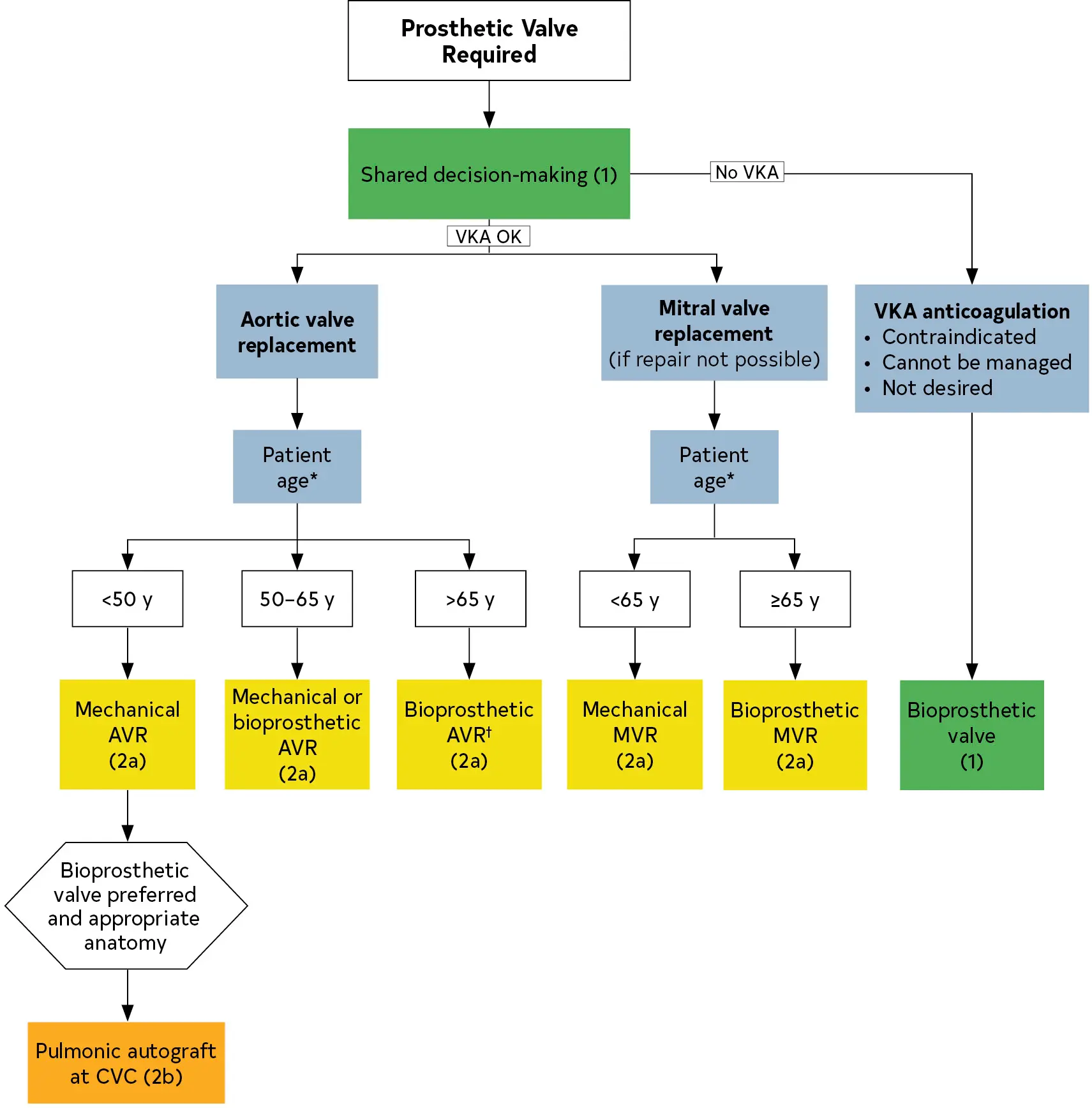
- Historically, MVs can be grouped into 3 major designs
- caged-ball
- tilting disk
- 🌟bileaflet valves
- the standard for modern valves as the previous two designs confer a higher thrombotic risk
- Mechanical valve dysfunction can be caused by 4 main phenomena:
- thrombosis
- fibrotic pannus ingrowth
- degeneration
- endocarditis
Management
- Asymptomatic patients can generally be followed with a clinician examination annually.
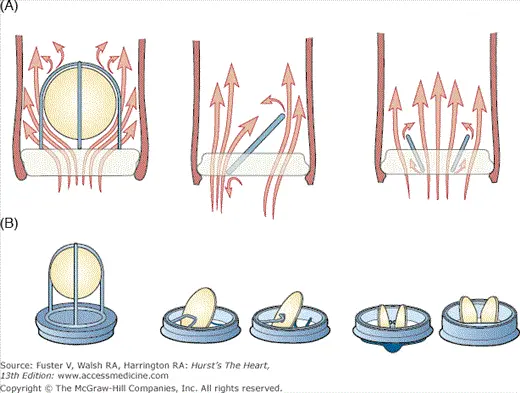
Anticoagulation
- In patients with a mechanical prosthetic valve, anticoagulation with warfarin is recommended (Class 1)
- Target INR of 2.5: aortic MVs in the absence of thromboembolic risk factors (eg, older-generation valves, AFib, previous thromboembolism, hypercoagulable states, and LV systolic dysfunction).
- Target INR of 3
- aortic MVs with risk factors
- all mitral MVs (regardless of risk factors)
- On-X valves have a lower INR goal
- Bioprosthetic valves
- TAVI:
- if low risk of bleeding, DAPT with aspirin 75 to 100 mg daily + clopidogrel 75 mg daily for 3-6 months post-implantation (Class 2a)
- aspirin 75 to 100 mg daily is reasonable (Class 2a)
- Bioprosthetic SAVR:
- TAVI:
Endocarditis Prophylaxis
Echo Surveillance
- Initial Echo
- “In patients with a surgical or transcatheter prosthetic valve and in patients who have had valve repair, an initial postprocedural TTE study is recommended for evaluation of valve hemodynamics and ventricular function” (Class 1)
- Surveillance Echo
- Guidelines recommend a follow-up echocardiogram 4-12 weeks after valve surgery to establish a new baseline.
- Waiting several weeks allows for recovery of anemia, stabilization from any early postoperative fluid shifts, and stabilization from perioperative medications, which may alter valvular gradients and/or ventricular mechanics early on.
- Bioprosthetic valves
- In patients with a bioprosthetic surgical valve, TTE at 5 and 10 years and then annually after implantation is reasonable, even in the absence of a change in clinical status. (Class 2a)
- In patients with a bioprosthetic TAVI, TTE annually is reasonable (Class 2a)
- Guidelines recommend a follow-up echocardiogram 4-12 weeks after valve surgery to establish a new baseline.
- Clinical deterioration → get a TTE (Class 1)
- If TTE doesn’t show valve dysfunction, get additional imaging (TEE, gated cardiac CT, or fluoro) (Class 1)
Bioprosthetic Valves
- Surveillance Echo
Complications
Thrombosis
- Poor adherence, brief interruption, or subtherapeutic anticoagulation are common.1
- On physical examination, there may be absent clicking associated with valve opening and closing, a new murmur, signs of pulmonary edema and heart failure, and sequelae of pulmonic or systemic thromboembolism.1
- Diagnosis depends heavily on a high index of suspicion and expedited imaging.
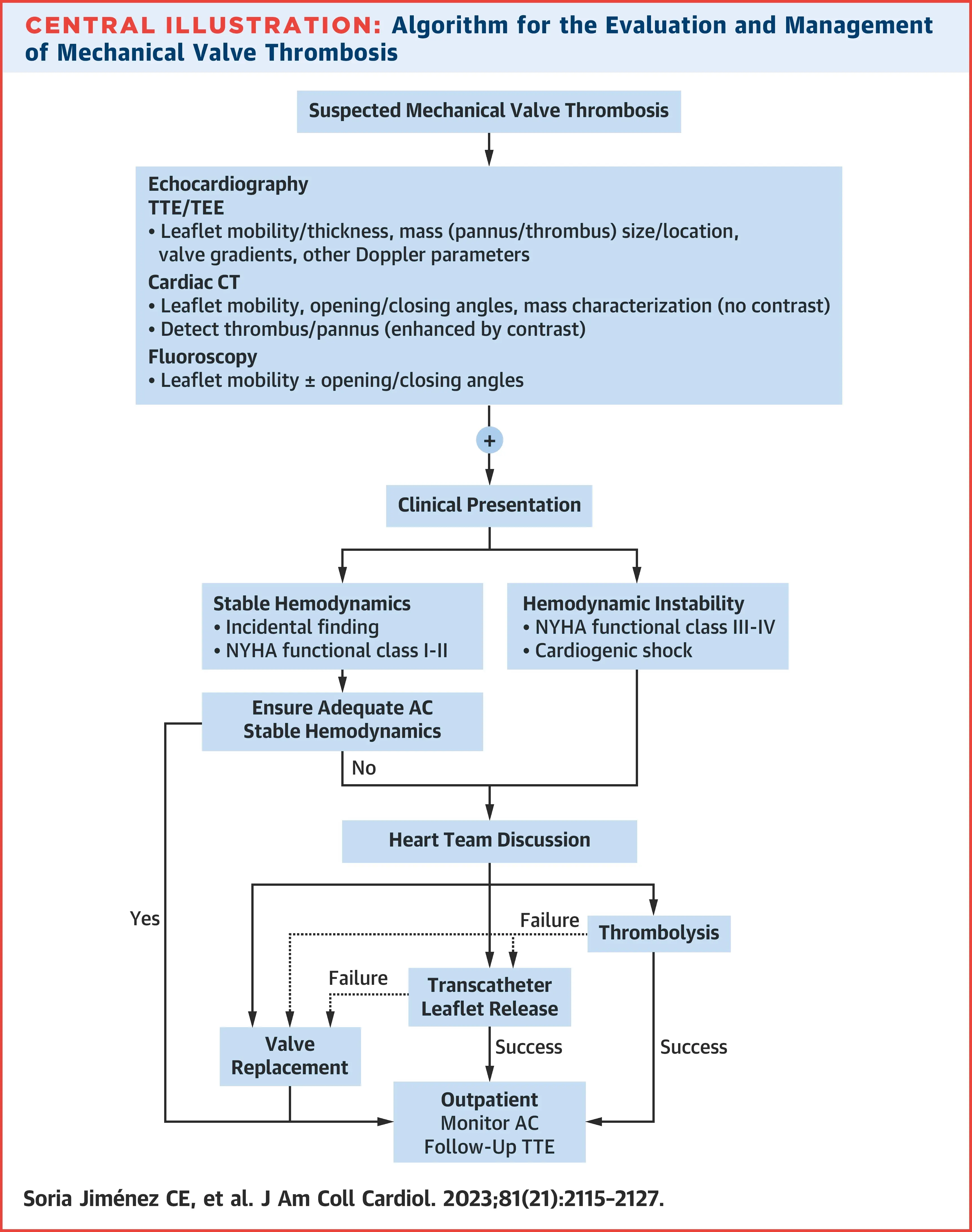 Figure source: 1
Figure source: 1
Diagnosis of mechanical valve thrombosis
Make sure it isn't pannus
Distinction of thrombus from pannus is essential, because thrombolytic therapy can be used for the former but is contraindicated in the latter. Current guidelines provide no diagnostic strategy to differentiate between thrombus and pannus.1 In general, pannus tends to be more circumferential and grows inward from the valve annulus. In contrast, thrombi are large and more asymmetric.1
- Echoecho
- focuses on valve appearance, leaflet mobility, and presence of thrombus
- Color Doppler
- Spectral Doppler
- Prosthetic valve obstruction is usually defined as a mean transvalvular gradient increase of >50% (or an increase >10 mm Hg across an aortic prosthesis) compared with the postoperative baseline value.1
- 📝 elevated gradients can also be observed with pannus formation, valve degeneration, high flow states, or patient-prosthesis mismatch
- An acceleration time (AT) >100 milliseconds is 86% sensitive and specific for prosthetic aortic valve obstruction.
- AT/ET ratio >0.37 provides 96% sensitivity and 82% specificity for stenosis, whereas an AT >128 milliseconds and AT/ET >0.58 is 100% specific for stenosis
- Diagnostic performance depends on which valve1
- Mitral Valve: opening/closing angles of mitral MVs can be correctly identified by TTE in 85% and by TEE in 100% of patients, regardless of valve.
- Aortic Valve: less accurate
- bileaflet → TTE and TEE correctly identifying opening angles only in 13% and 35%, respectively
- single-disk → TTE and TEE correctly identifying opening angles in 40% and 77% of cases, respectively
- Challenge: shadowing artifact being a main limitation
- Fluoroscopy
- Great non-invasive method to assess MV leaflet motion, especially in patients in whom TTE visualization of the valve is suboptimal or inconclusive.
- If bileaflet disks, compare the opening and closing angles measured in an orthogonal view, then compared to the “normal” angles reported by each valve manufacturer
- Cardiac CT
- The etiology of valve dysfunction can be discerned by using attenuation values to help differentiate thrombus from pannus. A cutoff point of ≥145 HU more likely represents pannus, with values below this more likely representing thrombus.
- ⚠️ mechanical valve artifacts may result in suboptimal image quality for analysis.
- Cardiac MRI
- ⚠️ significant artifacts often prevent accurate evaluation of structure and function. Currently, cardiac magnetic resonance is not recommended by any of the guidelines.1
Management of mechanical valve thrombosis
- Guideline-recommended treatments include heparin anticoagulation, thrombolysis, and surgery.1
- Transcatheter manipulation of immobile leaflets can be pursued when thrombolytic or surgical risk is prohibitive or as a bridge to surgery.
- Thrombolysis
- ACC/AHA guidelines give a Class I recommendation for either low-dose, slow thrombolytic therapy or surgery depending on clinical factors including clinical and surgical experience.1
- TROIA (Comparison of Different Transesophageal Echocardiography Guided Thrombolytic Regimens for Prosthetic Valve Thrombosis) trial
- 💊: low-dose (25 mg) and slow (6 hours) infusion of tPA without bolus
- PROMETEE (Prosthetic Mechanical Valve Thrombosis and the Predictors of Outcome) trial
- 💊: low-dose (25 mg), ultra-slow (25 hours) tPA infusion
- Important contraindications to thrombolysis in the above trials included left atrial thrombus, ischemic stroke within 3 weeks of presentation, history of hemorrhagic stroke, or a bleeding diathesis (generally an INR >3).
- ⚠️ The most important complications of thrombolytic therapy are pulmonary or systemic thromboembolic events and hemorrhage.
Hypoattenuated Leaflet Thickening (HALT)
See HALT
Footnotes
-
Soria Jiménez CE, Papolos AI, Kenigsberg BB, Ben-Dor I, Satler LF, Waksman R, Cohen JE, Rogers T. Management of Mechanical Prosthetic Heart Valve Thrombosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2023 May 30;81(21):2115-2127. doi: 10.1016/j.jacc.2023.03.412. PMID: 37225366. ↩ ↩2 ↩3 ↩4 ↩5 ↩6 ↩7 ↩8 ↩9 ↩10