Approach to WCT
- How does the QRS look in V1?
- i.e. is the terminal part positive or negative?
- Do you have marching QRS complexes in a wide complex rhythm?
- If so, that’s artifact.
- Look for VA dissociation, i.e. is the V faster than the A?
- In other words, do you have more QRS complexes than the P waves? If so, then that’s VT.
- If you cannot identify clear P waves, then the next step is to look at QRS morphology to ask the question, “is it physiologically possible to see such a QRS complex?”
- axis
- aVR with tall R wave (northwest axis)
- precordial transition
- positive or negative concordance
- septal activation (look for unexpected Q waves in V1 if RBBB-like or in V6 if LBBB-like)
- if patient has a RBBB-like morphology (terminal QRS is +) and it is aberrancy, the septum should be activated from L → R. ∴ physiologically, you would not expect a Q wave in V1 (or mirror image R wave in V6)
- if you have LBBB-like morphology, the septum should be activated from R → L with aberrancy, so it is not physiologically possible to see Q waves in V6
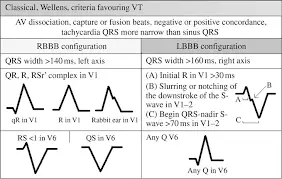
- initial versus terminal slope
- notch (Josephson’s sign) in predominantly negative QRS (V1 with LBBB-like morphology)
- initial slower than terminal → VT
- In VT, the initial part is going to be slow and the terminal portion will be fast as as it engages the His-Purkinje system
- initial faster than terminal → SVT
- with SVT, the unblocked bundle is going to be fast → the initial is fast and the terminal is slow
- axis
Differential Diagnosis
- DDx
- Ventricular Tachycardia (VT) (in 80% of cases)
- pre-excited Supraventricular Tachycardia (SVT)
- SVT with conduction down an accessory pathway (antridromic AVRT)
- pre-excited Atrial Fibrillation (AFib), i.e. WPW syndrome
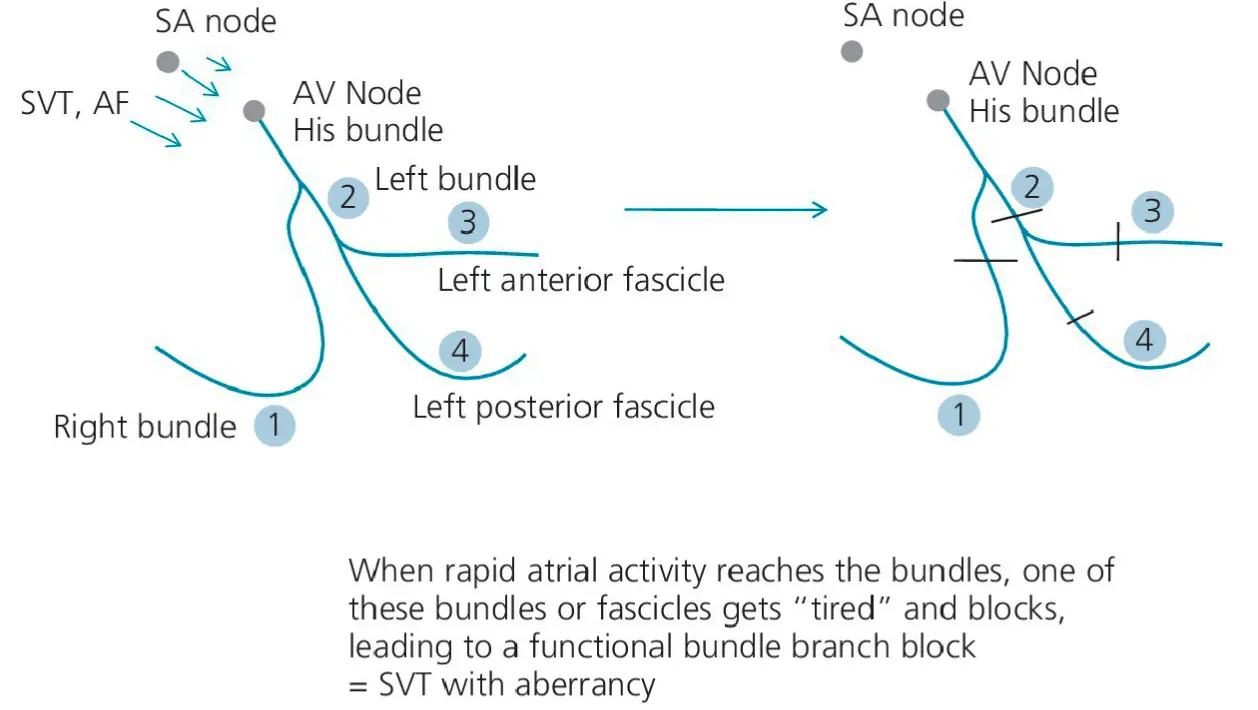
- Supraventricular Tachycardia (SVT) with aberrancy (abnormal intraventricular conduction)
- ventricular paced rhythm
- drug- and electrolyte-induced QRS widening
- Steps to evaluate and manage
- Assess vitals
- Assess clinical hx: CAD, COPD, etc.
- If HD stable → 12 lead EKG, vagal maneuvers/adenosine w/ the paper running!
- If HD unstable → ACLS protocol; Tx reversible causes
- urgent cardioversion should be done with procedural sedation when feasible
- fentanyl 50 or 2 of midazolam (usually work well)
- urgent cardioversion should be done with procedural sedation when feasible
- If WCT terminates w/ adenosine → Tx as SVT
- If WCT persists w/ adenosine and DDx still unclear → operate as if VT
- Amio generally most effective Tx for recurrent/refractory WCT, particularly VT
- If WCT d/t function over pacemaker → apply magnet over ppm → makes the pacemaker asynchronous and terminates ppm-related tachy
AV Dissociation Clues
P waves buried in QRS complexes may cause some QRS complexes to appear “notched.” Also, be on the look out for variable T wave morphology. This can be a hint to the presence of P waves that are dissociated from QRS/T and falling variably over some T waves.