- To read: 1
- ⚠️ Can also be present in patients with obstructive CAD
- ∴ unrecognized CMD may explain the 20-40% of patients who continue to experience angina following “technically successfully” revascularization
- CMD is the underlying cause of INOCA in one-half of cases2
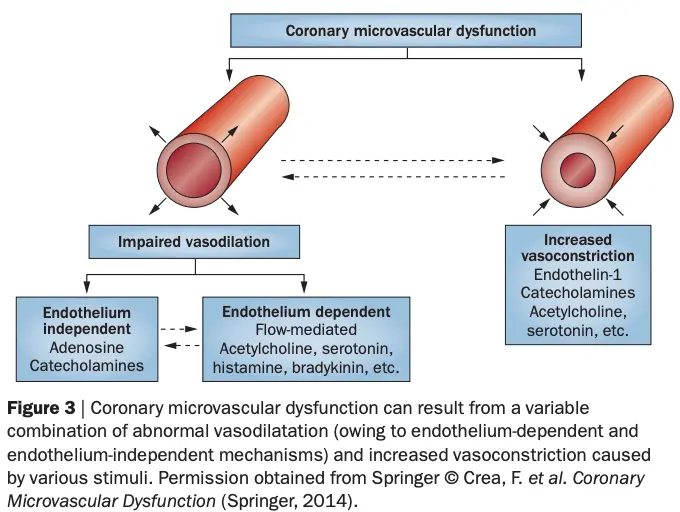
- Mechanisms of CMD
- impaired dilation (vasodilator abnormalities) and/or an ↑ constriction of coronary microvessels (microvascular spasm)
- Impaired vasodilation may be endothelium-dependent and/or endothelium-independent
- endothelium-mediated: ↓ production and/or ↑ degradation of NO
- tested using intracoronary infusion of Acetylcholine
- endothelium-independent is suggested by attenuated vasodilator responses to papaverine, adenosine, or dipyridamole
- likely involves an impaired relaxation of VSMCs
- endothelium-mediated: ↓ production and/or ↑ degradation of NO
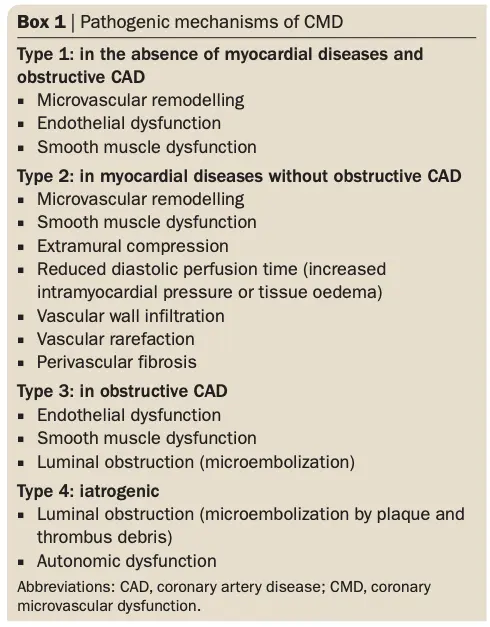
- Figure Source: Box 1 of 3
- CMD includes either
| Drug administered | Results | Diagnosis |
|---|---|---|
| Adenosine | Coronary flow reserve < 2.5 | Nonendothelial-dependent microvascular dysfunction |
| Acetylcholine | < 50% increase in coronary blood flow | Endothelial-dependent microvascular dysfunction |
| < 5% increase in coronary artery diameter | Endothelial-dependent macrovascular dysfunction | |
| > 90% decrease in coronary artery diameter Chest pain and ischemic ST-segment changes on electrocardiography | Epicardial coronary spasm | |
| Chest pain and ischemic ST-segment changes on electrocardiography in the absence of significant epicardial coronary vasoconstriction | Microvascular coronary spasm | |
| Nitroglycerin | < 20% increase in coronary artery diameter | Nonendothelial-dependent macrovascular dysfunction |
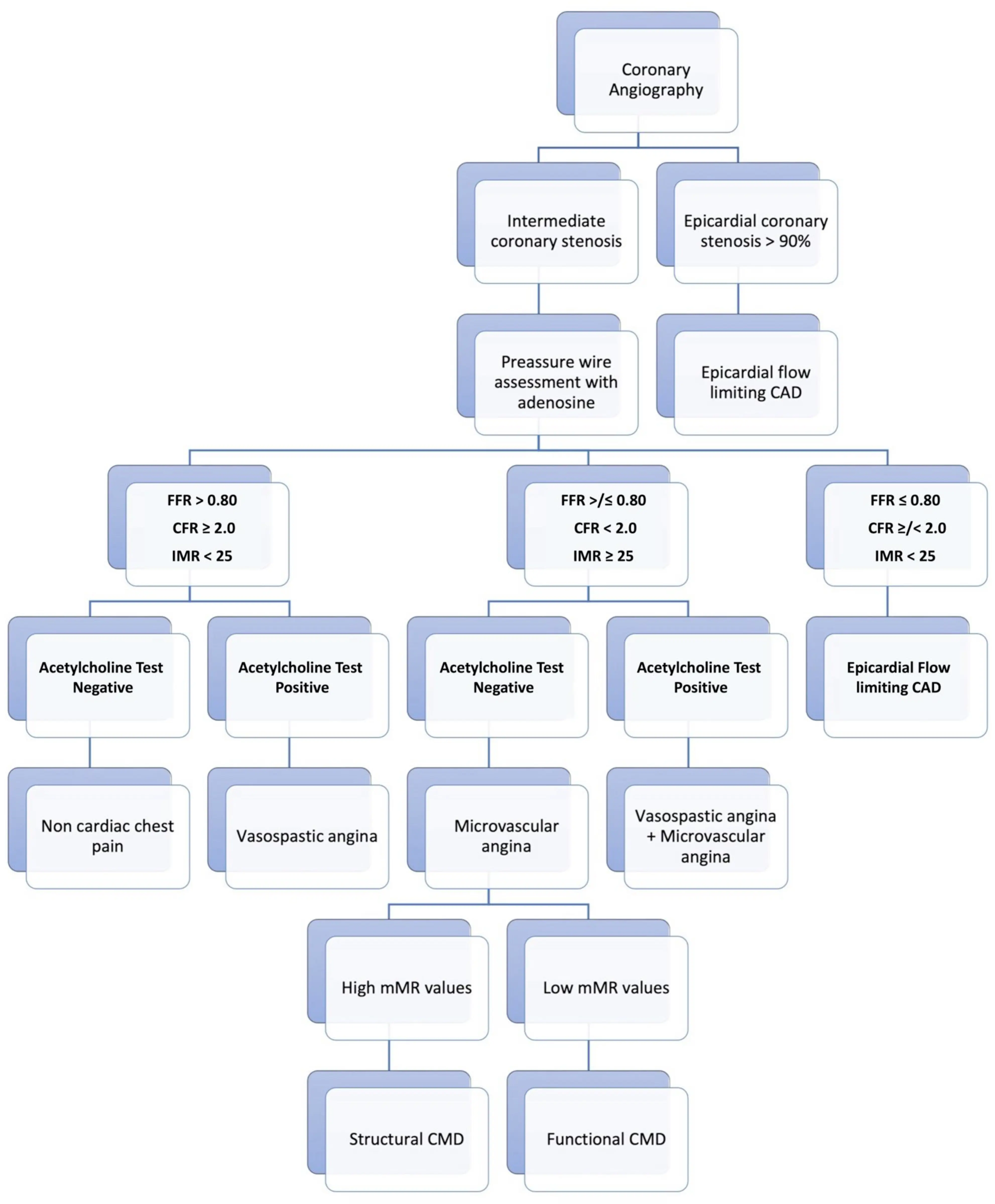
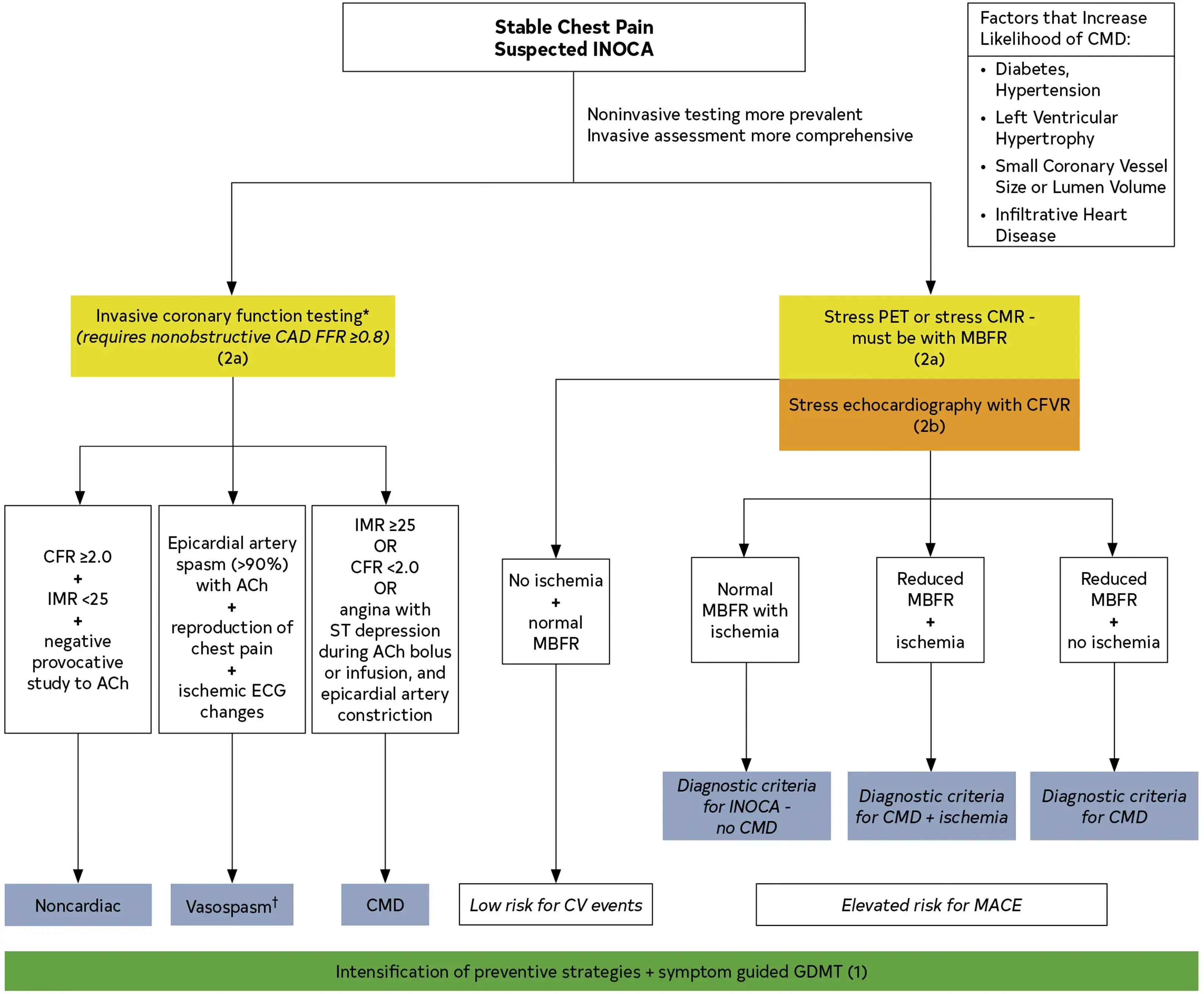
Adenosine testing
| CFR | IMR | Interpretation |
|---|---|---|
| ✅ (≥ 2) | ✅ (< 25) | Normal |
| ❌ (< 2) | ✅ (< 25) | Functional CMD |
| ✅ (≥ 2) | ❌ (≥ 25) | Structural CMD (early in course?) |
| ❌ (< 2) | ❌ (≥ 25) | Structural CMD |
- Acetylcholine testing
Treatments
Source: 2
| Endothelial dysfunction | Nonendothelial dysfunction | Vasospasm | Nociceptive abnormality |
|---|---|---|---|
| Angiotensin-converting enzyme inhibitor | Angiotensin-converting enzyme inhibitor | Calcium channel blocker | Tricyclic antidepressant |
| Angiotensin receptor blocker | Beta-blocker | Nitrate | Spinal cord stimulation |
| Statin | Alpha-/beta-blocker | Cognitive behavior therapy | |
| L-arginine | Ranolazine | ||
| Cardiac rehabilitation | Ivabradine | ||
| Enhanced external counterpulsation | Phosphodiesterase-5 inhibitor |
- To read: 4
Footnotes
-
Schindler TH, Dilsizian V. Coronary microvascular dysfunction: clinical considerations and noninvasive diagnosis. JACC Cardiovasc Imaging 2020;13:140-55. ↩
-
Tjoe B, Barsky L, Wei J, Samuels B, Azarbal B, Merz CNB, Shufelt C. Coronary microvascular dysfunction: Considerations for diagnosis and treatment. Cleve Clin J Med. 2021 Oct 1;88(10):561-571. doi: 10.3949/ccjm.88a.20140. PMID: 34598921; PMCID: PMC8813544. ↩ ↩2
-
Camici, P. G., d’Amati, G., & Rimoldi, O. (2014). Coronary microvascular dysfunction: mechanisms and functional assessment. Nature Reviews Cardiology, 12(1), 48–62. https://doi.org/10.1038/nrcardio.2014.160 ↩
-
Bairey Merz CN, Pepine CJ, Shimokawa H, Berry C. Treatment of coronary microvascular dysfunction. Cardiovasc Res 2020;116:856-70. ↩