# Endocarditis
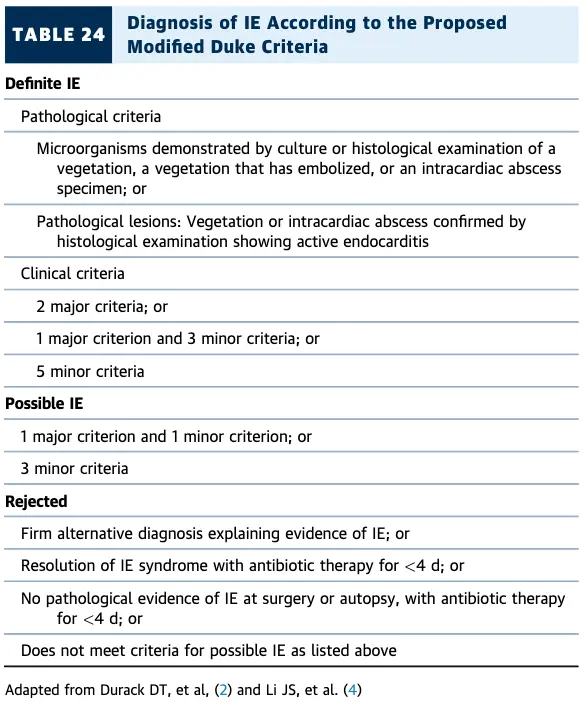
- Modified Duke Criteria: ***
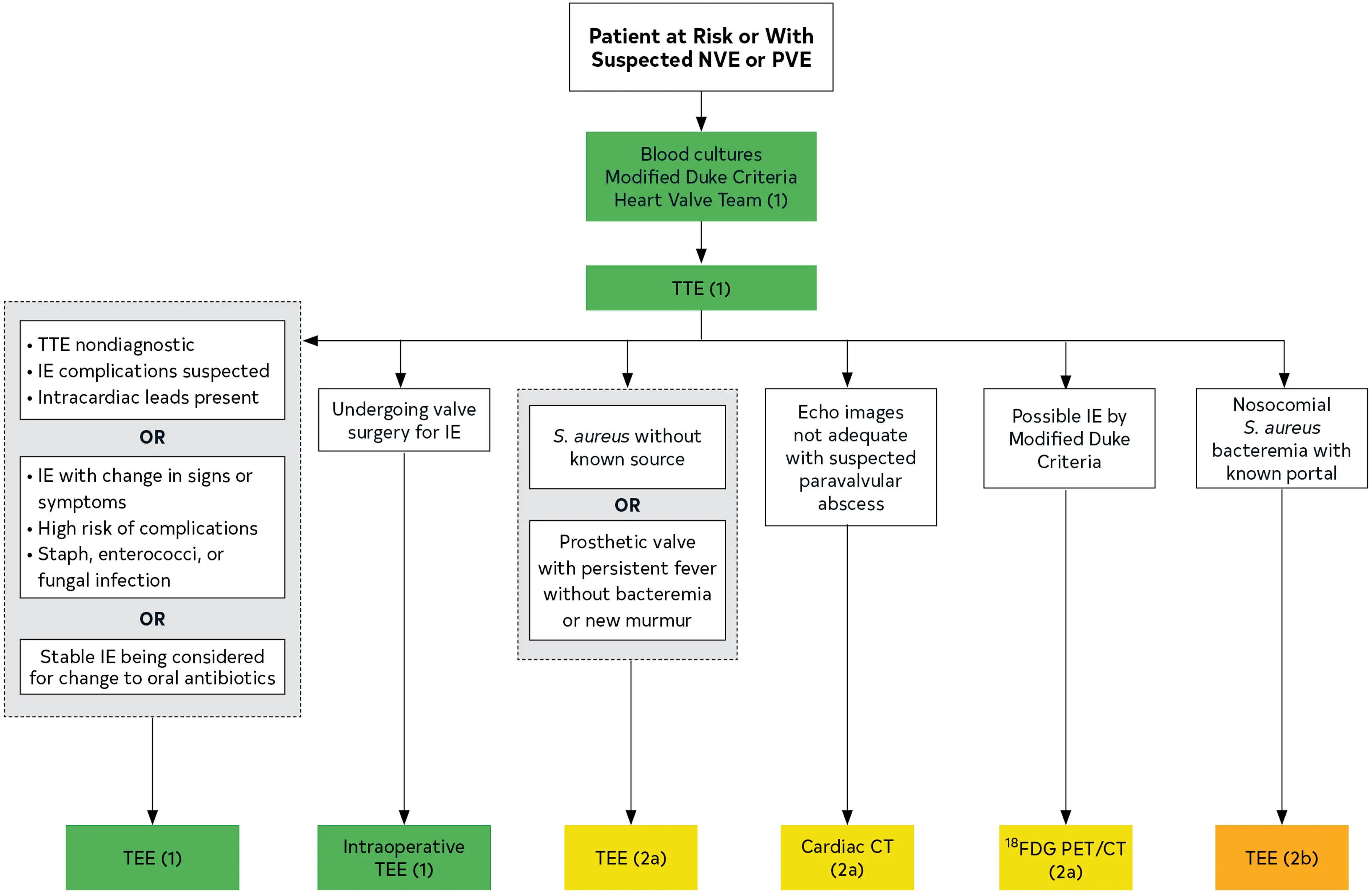
- If possible IE, plan for FGD-PET/CT
- BC x2
- TTE ordered to assess for vegetations, characterize the hemodynamic severity of valvular lesions, assess ventricular function and pulmonary pressures, and detect complications
- If TTE nondiagnostic, plan to proceed with TEE
- If paravalvular infection suspected, will order CT- Valves affected:
- MV > AV > TV > PV
- Microorganisms most commonly involved:
- Staph aureus (31%)
- Strep viridans (17%)
- Post-op: Staph epi early (within 2 months of valve surgery)
- Risk factors for IE:
- Age
- IVDU
- HD/IV lines
- Cancer
- Immunosuppression
- Structural heart disease
- Prosthetic valve/devices
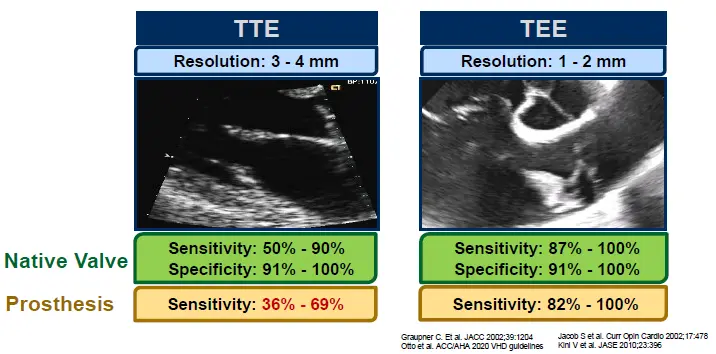
- TEE has better sensitivity for detecting bacterial endocarditis compared to TTE
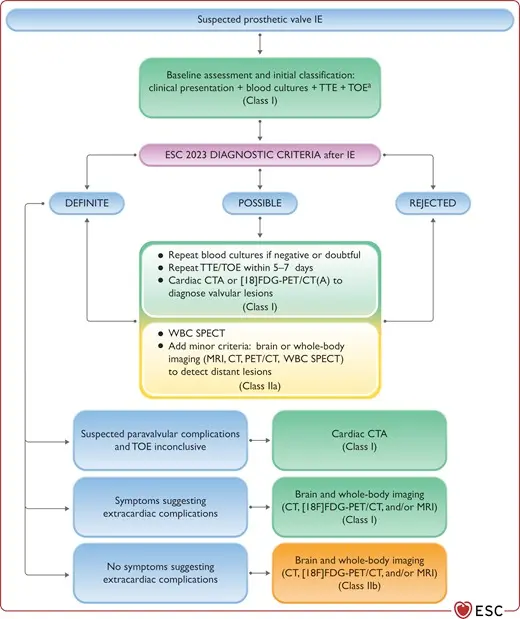
- Native valve vs. Prosthetic valve? - Timing of infection after valve intervention?
- Fatal if untreated
- in-hospital mortality rate is 15% to 20%, with a 1-year mortality rate approaching 40% 1
Diagnosis
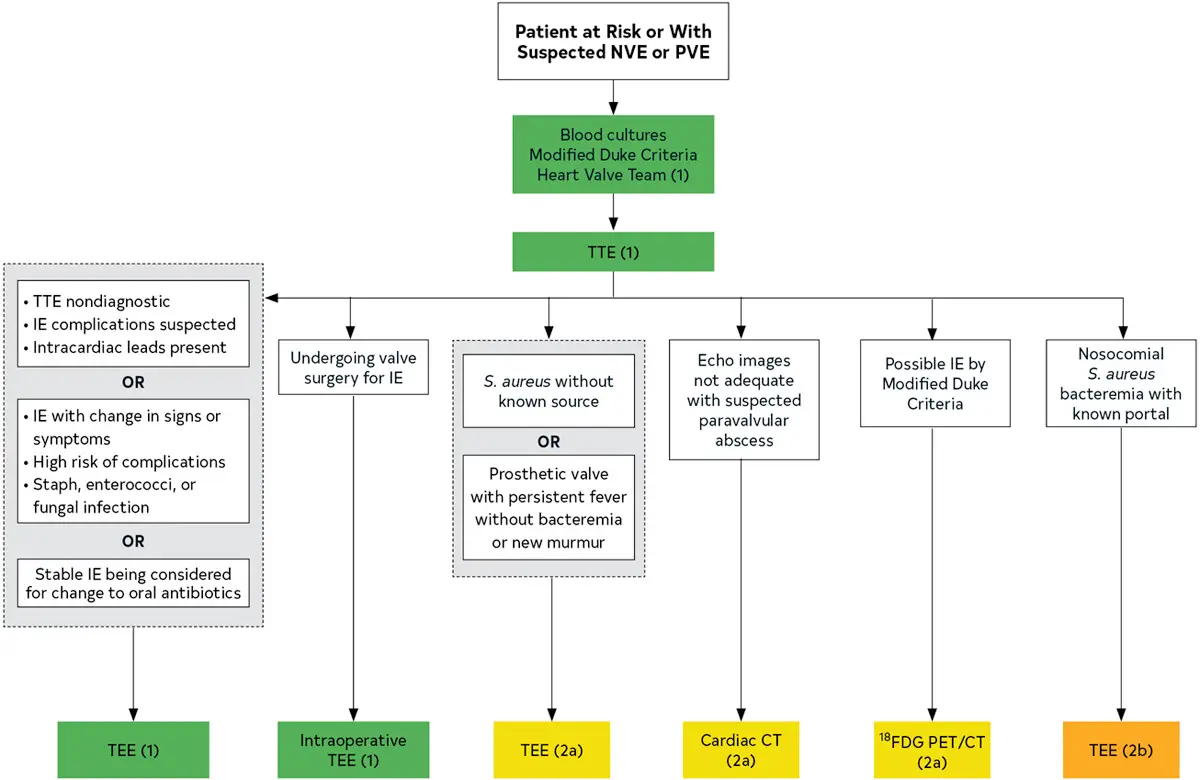 Figure source: 1
Figure source: 1
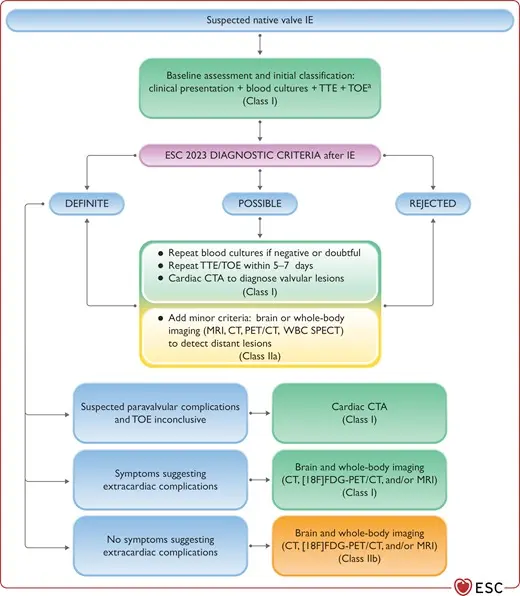
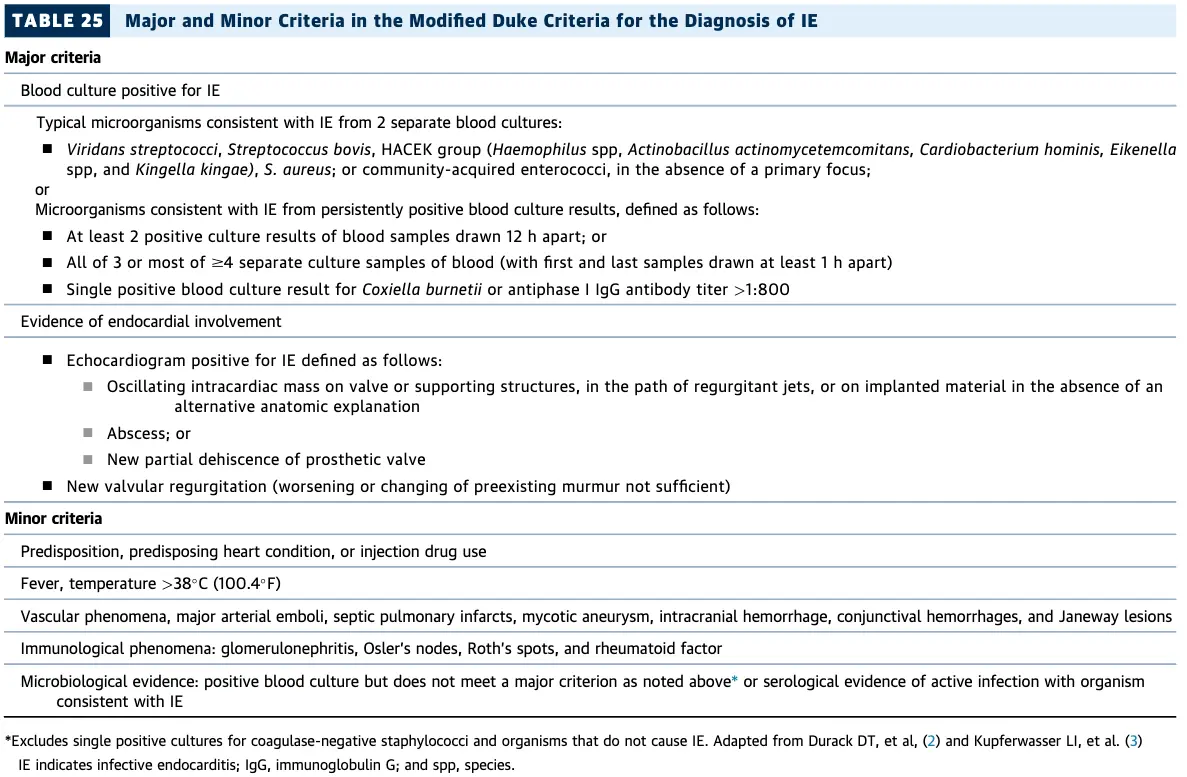
Modified Duke Criteria
Echo
Prosthetic valve endocarditis (PVE) may have NO vegetation
⚠️ 30-40% cases of prosthetic valve endocarditis (PVE) have NO vegetation attached to the prosthesis, only peri-annular infection. ∴, you may want to consider TEE or other imaging modalities for PVE.
- Echo reports for IE should comment on the following:
- Diagnosis: confirm presence, location, size, number & morphology of the vegetation(s)
- Structural complications
- Local severity of valve destruction
- Impact on surrounding structures abscess, fistula, aneurysm, dehiscence
- Systemic embolization
- Hemodynamic impact
- Acute regurgitation, CHF, shunt, tamponade, valve obstruction, hemolysis
- TTE vs TEE
- TTE can pick up a vegetation as big as 3-4 mm, whereas TEE can pick up a veg as small as 1-2 mm
- Class I indications for TEE?
- Suspected IE +
- non-diagnostic TTE, suspect IE complications, intracardiac leads present OR
- IE with change in Si/Sx, high risk of complications, Infection with Staph/Strep/Enterococci
- Stable IE and considering switch from IV → PO Abx
- Suspected IE +
- DDx for mobile endocardial echodensity:
- Lambl’s excrescence, fenestration
- Vegetation: infective/non-infective (healed)
- e.g. Libman-Sacks endocarditis
- Sclerosis/calcium artifact, MAC
- Ruptured/retracted chordae
- Myxomatous tissue
- Valvular strands, surgical remnants
- Papillary fibroelastoma, myxoma
- Thrombus (e.g. prosthetic thrombosis)
- Characteristics of vegetations (Major criteria of Duke’s for “Evidence of endocardial involvement”)
- Motion:
- oscillating intracardiac mass on valve, supporting structures, or prosthesis; independent motion
- Effects:
- new regurgitation (worsening or changing or pre-existing murmur is not sufficient)
- abscess
- new partial dehiscence of prosthetic valve
- Location:
- Upstream side of the valve in the path of the regurgitant jet or on prosthetic material
- No alternative anatomic explanation
- Texture:
- Gray scale, similar reflectance of myocardium
- Shape:
- Lobulated and amorphous
- Motion:
Cardiac CTA
Management
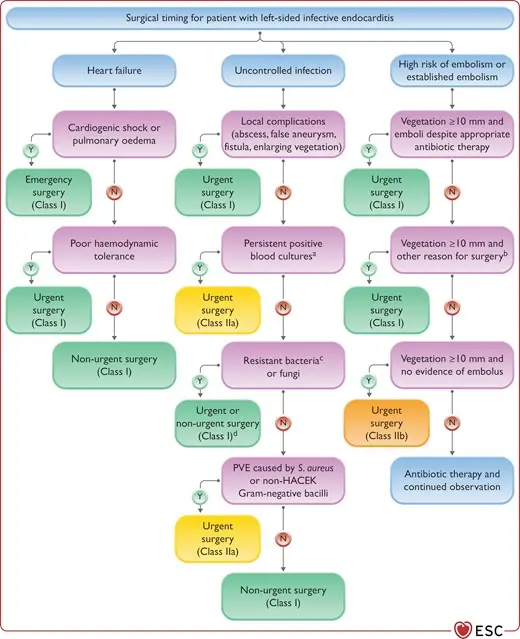
Complications
- Progression to involve the valve annulus → fistula between the LA and LV, which could result in significant regurgitation.
Footnotes
-
Otto, C. M., Nishimura, R. A., Bonow, R. O., Carabello, B. A., Erwin, J. P., Gentile, F., Jneid, H., Krieger, E. V., Mack, M., McLeod, C., O’Gara, P. T., Rigolin, V. H., Sundt, T. M., Thompson, A., & Toly, C. (2021). 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. Journal of the American College of Cardiology, 77(4), e25–e197. https://doi.org/10.1016/j.jacc.2020.11.018 ↩ ↩2