- Determining whether a patient needs a pacemaker depends on 3 things:
- is the conduction disorder producing symptoms?
- the site of the conduction disorder
- block in the AV node (proximal block) is usually benign, whereas block in the His-Purkinje system (infranodal) is potentially lethal
- the degree of the conduction block
- 1˚ and 2˚ AV block tend to be asymptomatic
| AV nodal block | Distal/Infranodal block | |
|---|---|---|
| First-degree | No | No (unless HV interval > 100 msec) |
| Second-degree | No (unless Sx brady) | Yes |
| Third-degree | No (unless Sx brady) | Yes |
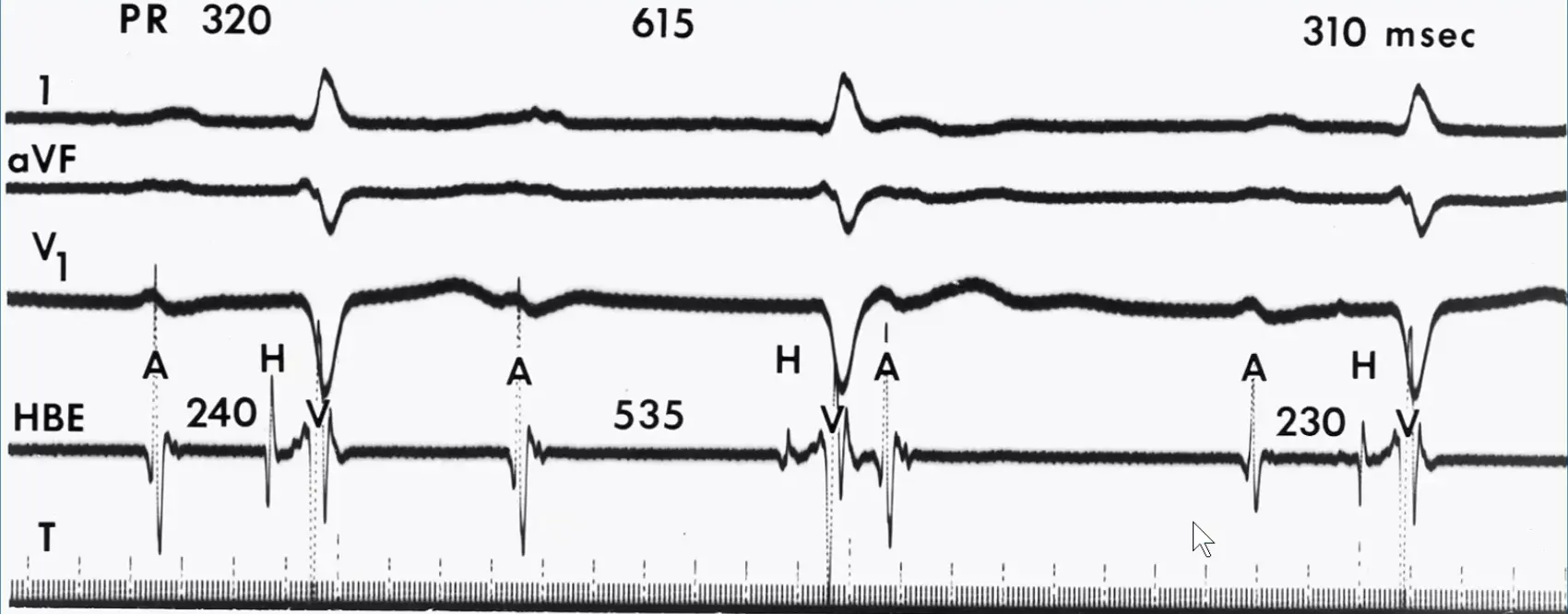 HBE - you see the A without an H after, so this is AV nodal block, i.e. above the His. The example here is Mobitz Type 1.
HBE - you see the A without an H after, so this is AV nodal block, i.e. above the His. The example here is Mobitz Type 1.
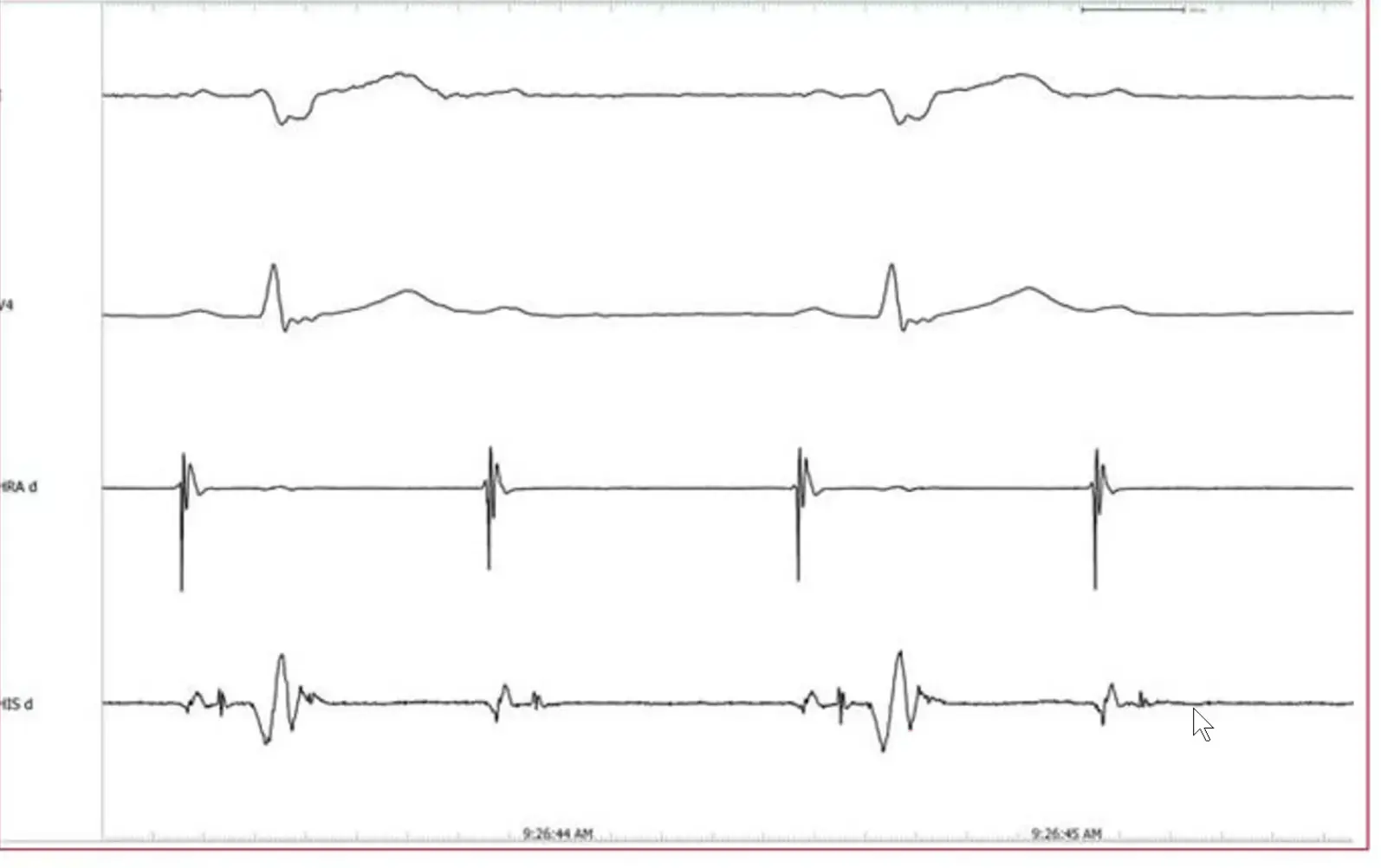 Here, you have A and H. This is an example of infranodal block as there is nothing after the H on a couple of these.
Here, you have A and H. This is an example of infranodal block as there is nothing after the H on a couple of these.
- If heart block is less than complete (i.e. first- or second-degree), it is still important to pinpoint the site of block to either the AV node (nodal) or the His–Purkinje system (infranodal). If in the AV node, it tends to be benign and non-progressive. If distal to the AV node (infranodal), it tends to progress to a higher degree of block; prophylactic pacing is often indicated.1
- Infranodal block is potentially life-threatening. This is largely d/t the unreliable, unstable, and slow escape pacemakers that tend to accompany this condition. Often discharge irregularly at a rate of 20-40 bpm and are prone to fail altogether.
- Infranodal block tends to be chronic and progressive in nature, i.e. not transient/reversible.
- You can often use the fact that the AV node has rich autonomic innervation in the His-Purkinje system to your advantage when trying to identify the site of the block when examining the surface ECG. 1
- maneuvers that ↓ vagal tone or ↑ sympathetic tone → expected to improve AV nodal block, but not distal block
- maneuvers that ↑ vagal tone or ↓ sympathetic tone → worsen AV nodal block, but not distal block
| AV nodal | Infranodal | |
|---|---|---|
| Exercise/isoproterenol | Improves | Conduction ratio may worsen |
| Atropine | Improves | Conduction ratio may worsen |
| Vagal maneuvers | Worsens | No change (maybe improve if can conduct 1:1) |
| Beta-blockers | Worsens | No change |
Vagal → slow them down if infranodal disease → conduct 1:1 An exercise test may help differentiate whether 2:1 atrioventricular block is due to Mobitz type I or II AV block. Exercise causes withdrawal of vagal tone and increased sympathetic tone leading to improved atrioventricular nodal conduction. If the baseline atrioventricular block is infranodal (Mobitz type II), the atrioventricular block will not resolve and will likely worsen as the sinus rate increases. If the latter ensues, a pacemaker would be indicated. If the atrioventricular block is Mobitz type I, then increased sympathetic tone would facilitate conduction through the AV node and may lead to resolution of the AV block.
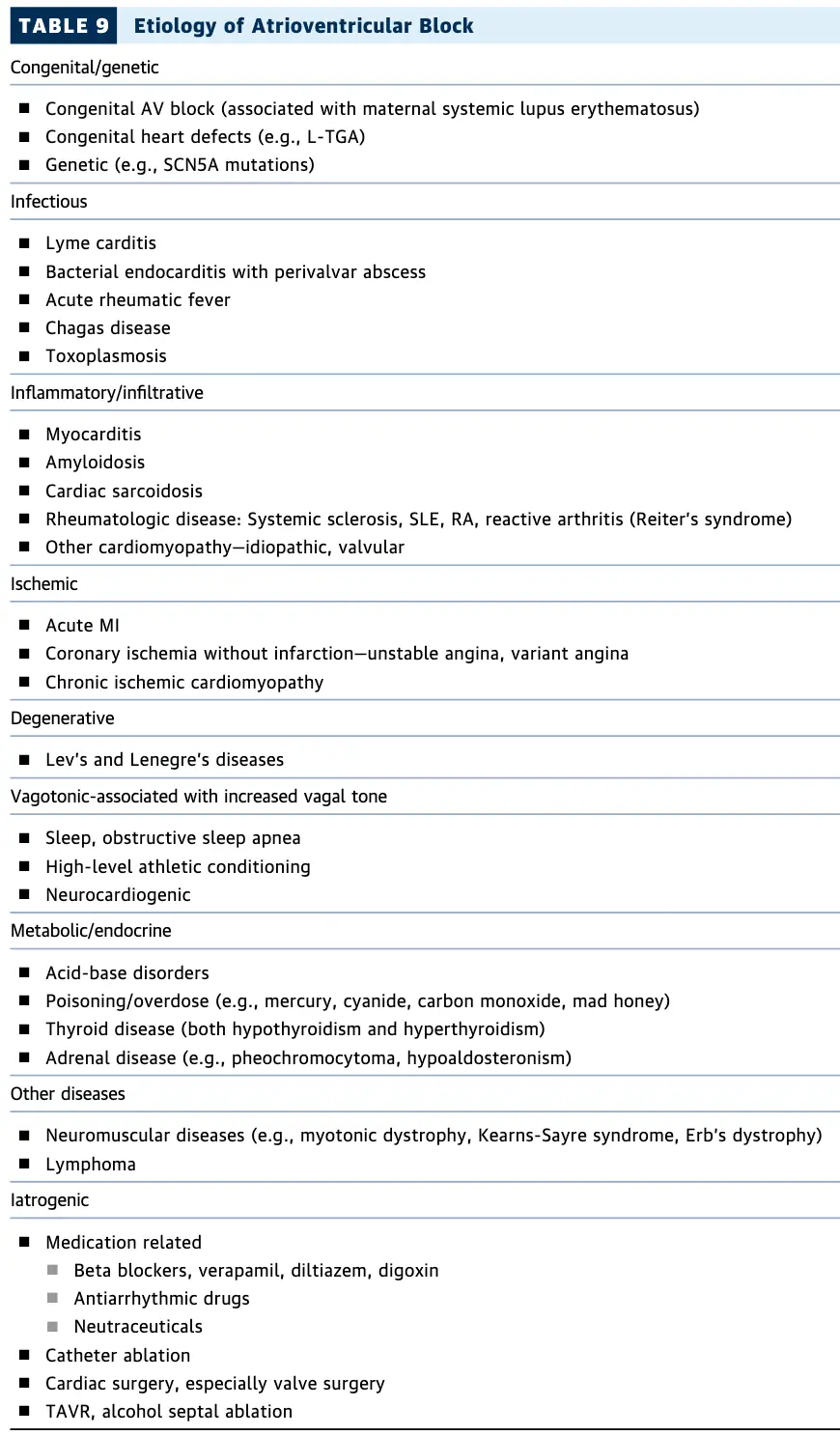
- Causes
- Ischemia or infarction
- the RCA gives off the AV nodal artery in ~90% of patients (inferior MI)
- tends to be transient
- LAD or anterior infarct tends to be associated with distal/infranodal AV block
- tends to be chronic and progressive
- the RCA gives off the AV nodal artery in ~90% of patients (inferior MI)
- Acute rheumatic fever and other cardiac inflammatory conditions
- Drugs, e.g. digoxin, BBs, CCBs
- typically the drug will cause 1˚ AVB and higher degree block suggests underlying intrinsic AV nodal dysfunction
- Ischemia or infarction
- 2:1 block
- 2 P waves for every QRS complex
- 📝 when you have 2:1 block, often can’t tell if Type I or Type II
- Clues to help differentiate Type I and II:
- QRS > 120 ms, e.g. RBBB morphology → you know conduction disease, which pushes you to Type II
- Exercise them, Wake them up and walk around → if conduction better then Type I. If worse (e.g. 2:1 → 3:1), then Type II.
- Carotid sinus massage and it goes from 2:1 → 1:1 conduction, it is Type II.
- carotid massage → ↑ vagal tone → conduction better b/c enough time to conduct every one of those beats
- If Type I, it should get worse
- Isoproterenol
- Clues to help differentiate Type I and II:
Initial Evaluation
Figure source: 2 Figure 3

Etiologies
First degree (1˚) AV Block
See First degree (1˚) AV Block
Second degree (2˚) AV Block
See Second degree (2˚) AV Block
Third degree (3˚) AV Block
Footnotes
-
Fogoros, R. N., & Mandrola, J. M. (2017). Fogoros’ electrophysiologic testing. John Wiley & Sons. ↩ ↩2
-
Kusumoto, F. M., Schoenfeld, M. H., Barrett, C., Edgerton, J. R., Ellenbogen, K. A., Gold, M. R., … & Varosy, P. D. (2019). 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Journal of the American College of Cardiology, 74(7), e51-e156. ↩