- Vasospastic angina is also called Prinzmetal angina or variant angina.
- Caused by spasm of a coronary artery → transient flow-limiting obstruction → angina
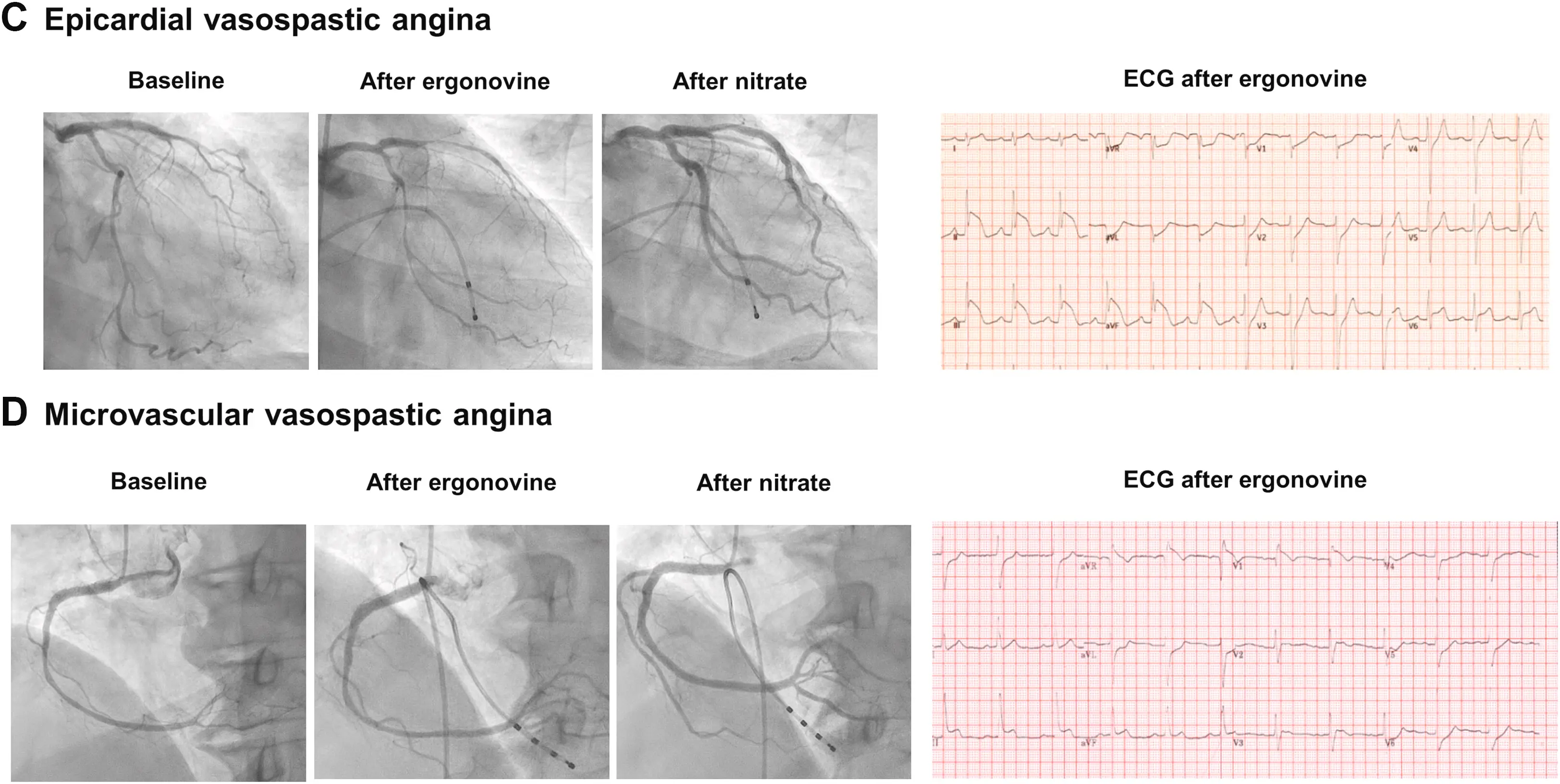
- 📝 A patient can have BOTH, i.e. concomitant epicardial and microvascular vasospastic angina
- coexistence confirmed in cases with microvascular vasospasm occurring with a lower dose of acetylcholine than epicardial artery spasm
- “Although it may potentially co-exist with coronary microvascular disorders and/or structural coronary artery disease, VSA is a clinical entity that is centred on the hyper-reactivity of large coronary arteries to vasoconstrictor stimuli.” 1
- Symptoms classically occur at rest, often from midnight to early AM. However, we now know that vasospastic angina can also occur with stress (physical/psychological) or even spontaneously.
- Angina attacks are usually short in duration (2-5 minutes, but sometimes only 30 sec) and may recur in clusters of more episodes within 20-30 minutes.2
- Main risk factor is cigarette smoking 🚬
- Provoking factors include alcohol 🍺, hyperventilation, epi, NE, cocaine, meth, exposure to cold temperature, exercise.
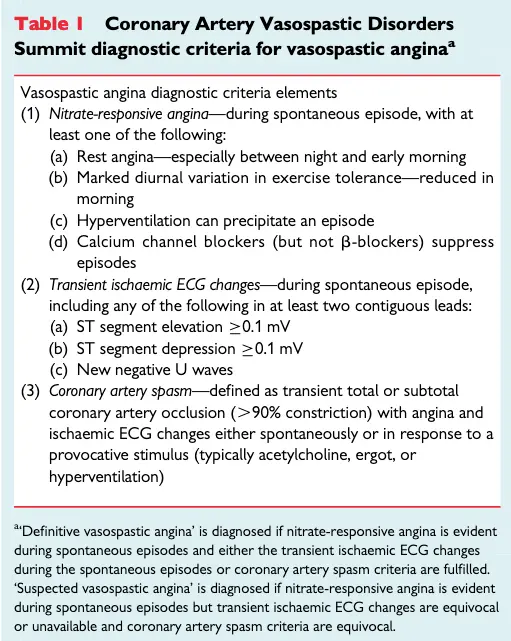
Diagnosis
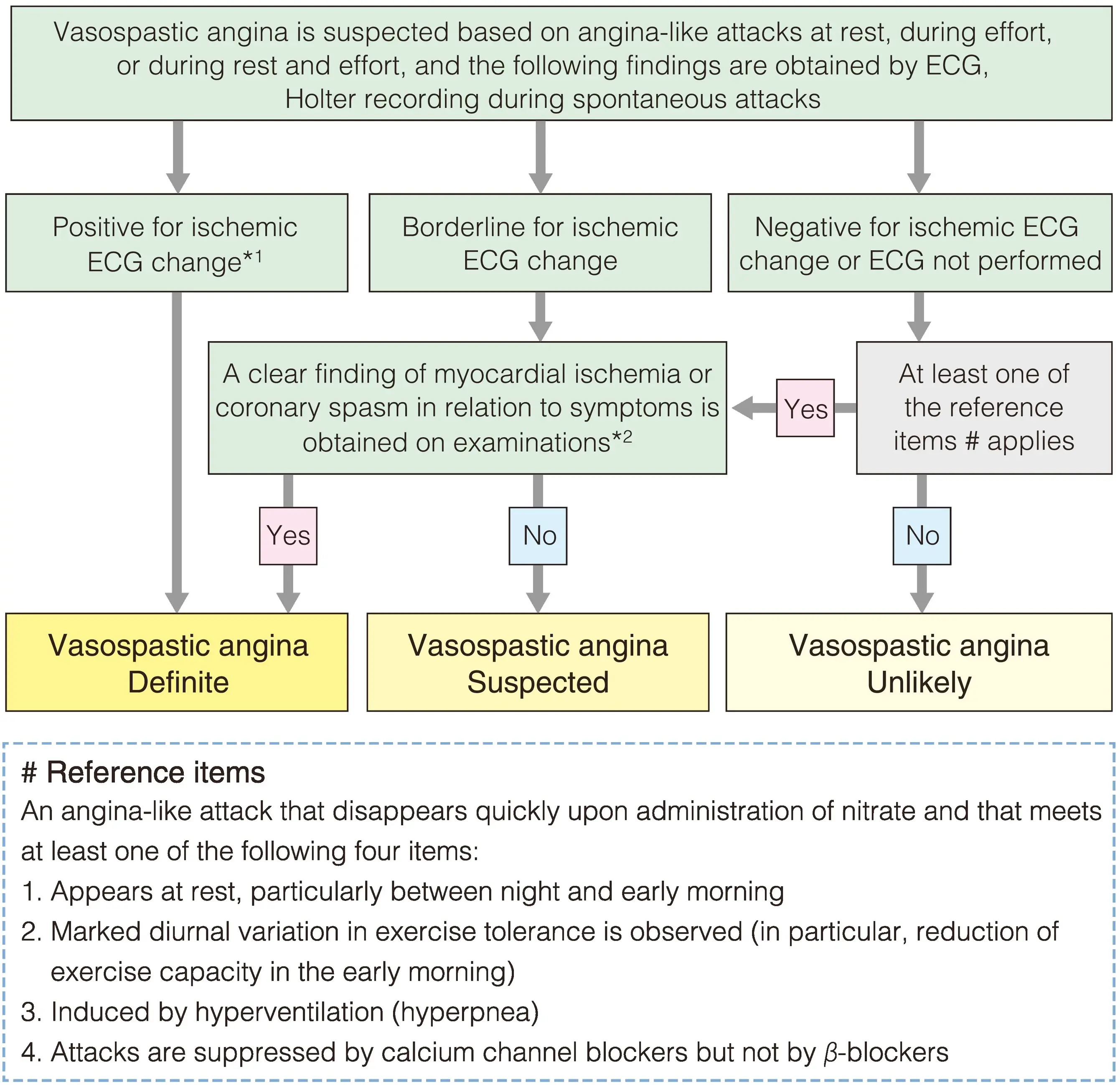
- ECG: transient ST-segment elevation (>1 mm) on the ECG during angina.
- Ambulatory ECG Monitoring: frequently reveals the presence of silent ischemic episodes, representing 75-80% of all ischemic attacks.
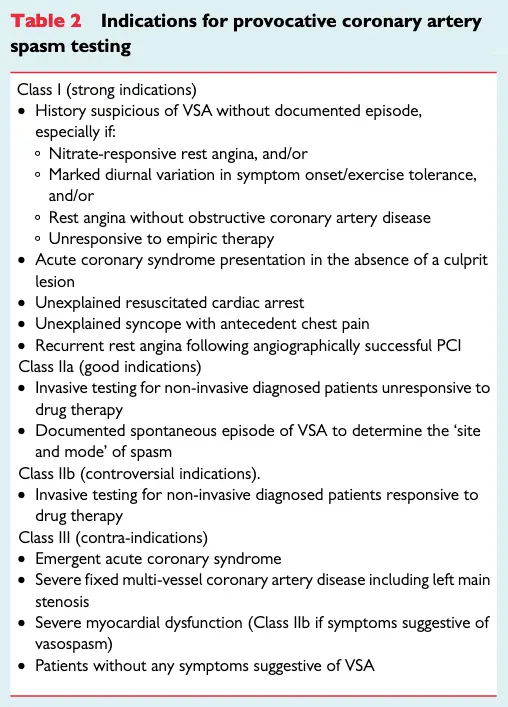
- Cath: observe spontaneous episode or provocative testing (typically with intracoronary acetylcholine) →
- “A positive provocative test for coronary artery spasm must induce all of the following in response to the provocative stimulus: (i) reproduction of the usual chest pain, (ii) ischemic ECG changes, and (iii) >90% vasoconstriction on angiography. The test result is considered equivocal if the provocative stimulus does not induce all three components.” 1
- followed by resolution w/ intracoronary nitroglycerin
- Classically: transient ST elevations are seen during an episode of chest discomfort without significant epicardial coronary artery disease (CAD) on cath. However, now that we recognize it can occur spontaneously or with stress, it is most often seen with ST depression and/or peaked T waves.
- “Documenting ischemic ECG changes during spontaneous episodes of rest angina occurs infrequently so that coronary artery spasm provocative testing is often required.” 1
- Figure source: 1
- Indications for provocative spasm testing:
Management
- 🚭 Smoking Cessation and avoiding other provoking agents
- Acute: nitroglycerin
- CCBs, such as amlodipine and diltiazem to prevent vasoconstriction.
- +/- long-acting nitrates (use in combination with CCBs)
- Timing of Rx
- Considering the diurnal variation of vasospastic attack, prescription time can be an important issue. To prevent angina in the early morning or at midnight, medication before sleep, not after dinner, can be useful to prevent the symptom 3
| Treatment | Mechanism of effect |
|---|---|
| CCBs (Amlodipine 10 mg or Verapamil 240 mg SR or Diltiazem 90 mg twice daily or 120–360 mg single or divided doses) | - ↓ Spontaneous and inducible coronary spasm via vascular smooth muscle relaxation - ↓ Oxygen demand |
| Nitrates (Isosorbide mononitrate XL 30 mg) | - ↓ Spontaneous and inducible coronary spasm via large epicardial vasodilation - ↓ Oxygen demand |
| Nicorandil (10-20 mg twice daily) | - Potassium channel activator with coronary microvascular dilatory effect |
Avoid non-selective BBs
Non-selective BBs, like propranolol, can worsen vasospasm!
Footnotes
-
Beltrame, J. F., Crea, F., Kaski, J. C., Ogawa, H., Ong, P., Sechtem, U., Shimokawa, H., & Bairey Merz, C. N. (2015). International standardization of diagnostic criteria for vasospastic angina. European Heart Journal, ehv351. https://doi.org/10.1093/eurheartj/ehv351 ↩ ↩2 ↩3 ↩4
-
https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-2/Vasospastic-Angina-Title-Vasospastic-Angina ↩
-
Hwang, D., Park, S.-H., & Koo, B.-K. (2023). Ischemia With Nonobstructive Coronary Artery Disease. JACC: Asia, 3(2), 169–184. https://doi.org/10.1016/j.jacasi.2023.01.004 ↩